What are the other Names for this Condition? (Also known as/Synonyms)
- Bannwarth Syndrome
- LD (Lyme Disease)
- Lyme Borreliosis
What is Lyme Disease? (Definition/Background Information)
- Lyme Disease (LD) is a non-contagious bacterial infection, caused by Borrelia burgdorferi. The disease is transmitted through the bites of infected blacklegged ticks
- Lyme Disease is reported to be the most prevalent tick-borne illness in Europe and North America. Typically, young children (below 15 years) and middle-aged and older adults (over 50 years) are more vulnerable to the infection
- The infected ticks lurk in grassy and heavily-wooded areas in the endemic regions, and therefore, such areas pose a potential risk for tick bites and consequently Lyme Disease
- Lyme Disease is categorized into three stages, depending on the progression of infection in the body. The symptoms experienced by an individual are dictated by the stage of the disease
- Stage 1 or ‘early localized Lyme Disease’, when the individual’s skin at the implantation site is infected, but the infection has not spread to other parts of the body
- Stage 2 or ‘early disseminated Lyme Disease’: In this stage, the causative bacteria begin to spread throughout the body
- Stage 3 or ‘disseminated Lyme Disease’, when infecting bacteria have spread throughout the body, including to internal organs
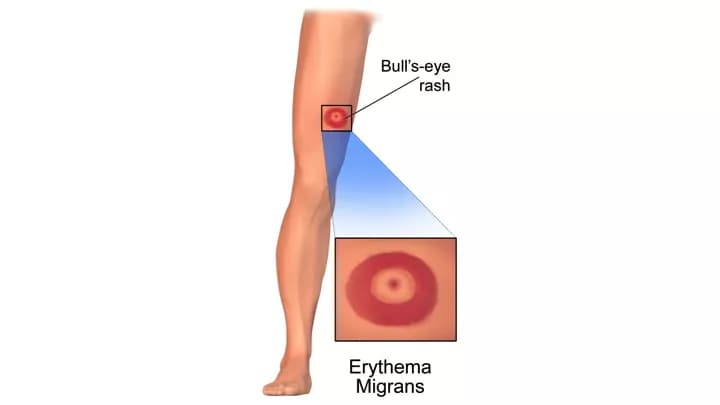
- In stage 1 of the disease, an infected individual could have a non-painful, non-itchy rash on the skin, and flu-like symptoms (fever, tiredness, and headaches). The rash presents a characteristic “bull’s eye” appearance (called erythema migrans)
- If not treated promptly, the disease can progress to stage 2, spreading to other parts of the body. The symptoms can include rashes on other parts of the body, away from the first rash, as well as joint pain and neurological problems. In severe cases, internal organs, such as the heart and liver, may be affected
- A healthcare provider might perform a physical examination, evaluate possibility of tick bites, and assess symptoms to diagnose Lyme Disease. Enzyme-linked immunosorbent assay (ELISA) test and western blot test are the commonly used laboratory procedures for the diagnosis of the infection
- The standard treatment for Lyme Disease is through antibiotics. Whether the affected individual needs oral or intravenous antibiotics is dictated by the severity and spread of infection
- Some potential complications from severe infection in Lyme Disease can include neurological symptoms (such as facial palsy), joint inflammation and pain, meningitis, and heart arrhythmia
- Lyme Disease may be prevented through using an insect repellant, keeping lawns/bushes trimmed, clearing piles of leaves, wearing clothes that leave the least amount of skin exposed, and looking for ticks on skin and removing them, following an outdoor activity in the endemic area
- The prognosis for Lyme Disease is favorable, if it is diagnosed and treated without any delay following the appearance of early-stage symptoms
Who gets Lyme Disease? (Age and Sex Distribution)
- Lyme Disease is the most prevalent illness spread by ticks in certain regions of North America and Europe (endemic regions)
- The disease can affect individuals of all ages and both male and female genders
- However, children under 15 years of age and adults over the age of 50 years are reported to be more susceptible to Lyme Disease
What are the Risk Factors for Lyme Disease? (Predisposing Factors)
The risk for contracting Lyme Disease is greatest in the endemic regions. When people spend considerable time outdoors (in the forests or grassy plains), either due to an occupation or for recreation, they increase the chances of tick bites, and hence, of Lyme Disease.
The risk factors for Lyme Disease may include:
- Frequenting areas that have overgrown grass, bushes, or are heavily-wooded: The blacklegged ticks, which reside in heavily-wooded and grassy areas, overgrown bushes, and leaf piles, spread the disease when they bite people
- Occupations that necessitate frequent outdoor works
- Recreational outdoor activities
- Exposed skin while being in tick-infested areas
- Letting pets wander in areas where blacklegged ticks may potentially lurk
- Not conducting self-checks (and checking the pets) after an outdoor activity for ticks and not removing them promptly
- Not seeking medical attention when the symptoms are still localized
It is important to note that having a risk factor does not mean that one will get the condition. A risk factor increases one’s chances of getting a condition compared to an individual without the risk factors. Some risk factors are more important than others.
Also, not having a risk factor does not mean that an individual will not get the condition. It is always important to discuss the effect of risk factors with your healthcare provider.
What are the Causes of Lyme Disease? (Etiology)
Lyme Disease is caused due to infection by Borrelia burgdorferi, a flat bacterial species.
- The bacterium is transmitted to humans by bites of infected blacklegged ticks. The bacteria enter through the broken skin caused by a tick bite
- The ticks must be attached to the skin of an individual (or a pet) for 36 hours or longer for the bacteria to enter the bloodstream
- It may be difficult to spot the ticks owing to their small size. Female ticks are larger than the males; a fully-grown female measure about 5 mm in size
- The immature ticks (nymphs) are even smaller, about the size of a pinhead. The ticks might become visible when they are swollen, after they have fed on blood for a few hours
Lyme Disease is not contagious, and it does not spread from one individual to another.
What are the Signs and Symptoms of Lyme Disease?
The signs and symptoms of Lyme Disease depend on the stage of infection.
Early stage symptoms, observed 3-30 days after the infected tick bite, may include:
- A red bump at the site of tick bite (though it may not indicate Lyme Disease)
- Skin rash, small to begin with, but expanding if infected with Borrelia burgdorferi
- The rash, also known as Erythema Migrans, can get as large as 30 cm across, and might have a clearing in the center, giving an appearance of “bull’s eye”
- The rash may be localized to one spot or could appear on multiple spots
- Fever, chills
- Muscle ache, headaches
- Tiredness
Later stage symptoms, observed a few weeks to months after the tick bite, when the individual ignores the initial symptoms, may include:
- Erythema Migrans on one or several areas of the body
- Severe joint pain
- Neurological symptoms such as:
- Weakness in arms and legs
- Problems with movement, muscle weakness
- Facial palsy or Bell’s palsy (temporary paralysis on one side of the face)
- Meningitis
- Infrequently, some individuals might develop symptoms such as:
- Hepatitis
- Extreme weakness and tiredness
- Irregular heartbeat
- Eye inflammation
How is Lyme Disease Diagnosed?
A diagnosis of Lyme Disease may be difficult, owing to the following:
- The wide range of symptoms associated with Lyme disease overlapping with other conditions
- The fact that blacklegged ticks are known to spread other diseases concomitantly
However, a healthcare provider might diagnose the disease based on:
- A physical examination of the affected individual
- An assessment of the presenting symptoms, in conjunction with the individual’s personal medical history, recent outdoor activity, time of year (the risk of human infection is greatest in late spring and summer), etc.
- Lab tests, such as enzyme-linked immunosorbent assay (ELISA) to check for Lyme Disease, and western blot to check for the presence of Borrelia burgdorferi with antibodies, thus confirming the disease
Many clinical conditions may have similar signs and symptoms. Your healthcare provider may perform additional tests to rule out other clinical conditions to arrive at a definitive diagnosis.
What are the possible Complications of Lyme Disease?
Some potential complications that arise from untreated Lyme Disease may include:
- Lyme arthritis; chronic joint pain and inflammation, particularly of the knee
- Arrhythmia or irregular heartbeat
- Meningitis
- Facial palsy
- Confusion, memory-related issues
- Side-effects of antibiotics treatment, such as diarrhea, low white blood cells count, secondary infections due to drug-resistant bacteria, etc.
- Post-treatment Lyme Disease syndrome: A small number of individuals might have continuing symptoms, such as muscle ache, fatigue, etc., even after treatment with antibiotics
How is Lyme Disease Treated?
The standard treatment for Lyme Disease is administration of antibiotics. Depending on the stage of the disease, oral antibiotics or intravenous antibiotics may be prescribed.
- Early-stage Lyme Disease: Oral antibiotics, such as doxycycline, amoxicillin or cefuroxime, may be prescribed. The affected individuals may have to take antibiotics for a period of up to 21 days. Patients are advised to finish the prescribed course of antibiotics, even if they feel better or symptoms disappear in a few days
- Late-stage Lyme Disease: Intravenous antibiotics may be administered for a period of 14-21 days, if the infection spreads to other parts of the body (such as to the internal organs and central nervous system)
- Post-treatment: Some individuals might continue to feel tired and have muscle pain even after treatment. This is known as post-treatment Lyme Disease syndrome, the cause of which is unknown
- If symptoms continue to occur after antibiotics are stopped, it is not indicative of an active infection, and antibiotic treatment is not additionally recommended
Note:
- Oral antibiotics might lead to side effects such as diarrhea
- Intravenous antibiotics administration could lead to side effects, such as diarrhea, low count of white blood cells, colonization by opportunistic drug-resistant bacteria, etc.
- It is very important to note that bismacine is not approved as an injectable treatment by the Food and Drug Administration, USA. However, some alternative and complementary medicine practitioners do prescribe the injectable form, which may result in harm. The medicine contains bismuth that can cause heart and kidney failure
How can Lyme Disease be Prevented?
The following steps may help in the prevention of Lyme Disease:
- Avoid visiting tick-infested areas when possible, or take adequate protection while doing so
- Leave the least amount of skin exposed, while in tick-infested areas
- Use insect repellents (20% or higher concentration of DEET)
- Use permethrin-treated clothes
- Shower immediately after any outdoor activity
- Wash clothes worn outdoors separately and dry them in high heat
- Keeping grass mowed, the undergrowth and bushes cleared, yard cleaned, etc.
- Checking self and pets for ticks on skin, immediately after finishing the outdoor activities
- Remove the ticks promptly with tweezers and apply an antiseptic cream to the skin
What is Prognosis of Lyme Disease? (Outcomes/Resolutions)
- The prognosis of Lyme Disease is good with early diagnosis and prompt treatment
- However, if treatment is delayed till the later stages of infection, an individual might develop severe complications such as nerve and heart problems
- An individual might develop post-treatment Lyme Disease syndrome and keep having symptoms even on completion of full course of treatment
Additional and Relevant Useful Information for Lyme Disease:
- Babesiosis is a rare and severe tick-borne disease, caused by a parasite. The ticks (blacklegged ticks, deer ticks, or bear ticks) are carriers to parasites of the genus babesia
The following link may help you find useful additional information on babesiosis:
Related Articles
Test Your Knowledge
Asked by users
Related Centers
Related Specialties
Related Physicians
Related Procedures
Related Resources
Join DoveHubs
and connect with fellow professionals


0 Comments
Please log in to post a comment.