What is Kneecap Dislocation?
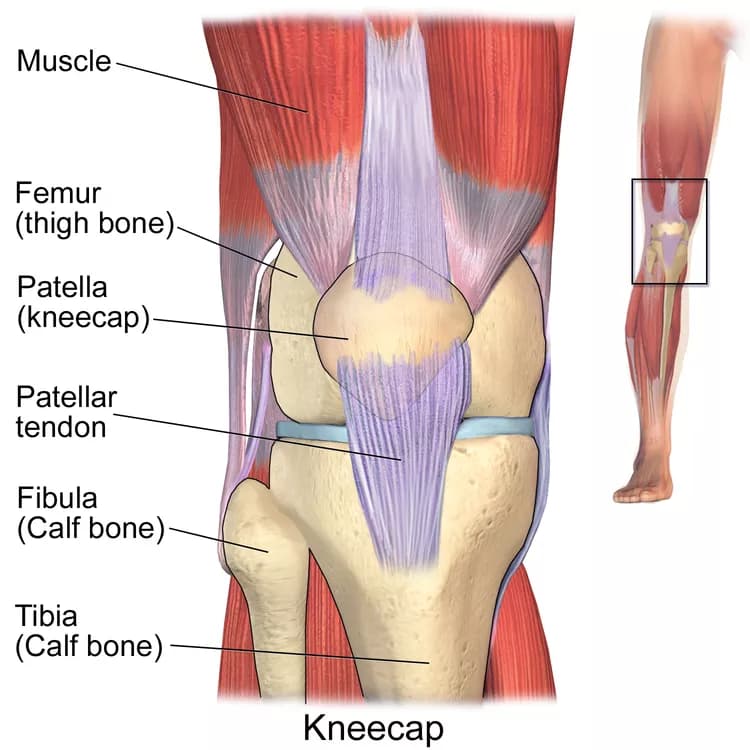
- A Kneecap Dislocation occurs when the kneecap (or patella) is forcefully moved out of its normal position in the knee joint. It is also known as a Patellar Dislocation
- The injury is more often seen in young sports athletes, older adults, and individuals with predisposing risk (genetic) factors, including those having a history of Kneecap Dislocation
What are the Causes of Kneecap Dislocation?
Kneecap Dislocation may be caused by a variety of factors including:
- Trauma to the knee, usually due to a direct impact or twisting motion of the ankle/knee
- Injury during sports activities
- Fall injuries, such as due to slipping or stumbling over objects/steps
- Motor vehicle accidents
What are the Signs and Symptoms of Kneecap Dislocation?
The signs and symptoms of a Kneecap Dislocation include:
- Tenderness and severe pain in the affected knee
- Obvious deformation of the joint; the kneecap is movable to the right and left, to a much greater degree than normally possible
- Unable to walk
- Inability to move the knee joint; in some cases, the injured leg comes back to its original position after it is flexed
- Swelling and redness
- Bruising or contusion, depending on the type of trauma
- Sensory disturbances (tingling or numbness, or both) in the distal limb
How is First Aid administered for Kneecap Dislocation?
First Aid tips for Kneecap Dislocation include:
- Call 911 (or your local emergency number), if there is a medical emergency due to the accident/trauma
- DO NOT move the individual, if there is a suspicion of other injuries, or if he/she is unable to walk/move
- DO NOT move the knee joint; doing so may aggravate the injury
- Try to sit without much movement in a comfortable position
- If the kneecap has returned to its original position, do not put pressure on the affected limb or try to walk; but, seek medical evaluation and help
- Apply ice on the injured site to reduce pain and swelling, only if there are no open wounds/injuries
- If there is bleeding from an associated wound, then take suitable steps (such as direct pressure for severe bleeding) to arrest the bleeding
Depending on the extent of dislocation, the healthcare provider may undertake a simple reduction procedure (to put the kneecap back in place) followed by physical therapy to restore the muscles; or the healthcare provider may perform a surgery, if the injury is severe such that the cartilage, bone, and muscles are damaged.
Who should administer First Aid for Kneecap Dislocation?
The injured individual or any bystander can administer first aid; however, the affected individual must seek medical assistance for a definitive management of Kneecap Dislocation.
What is the Prognosis of Kneecap Dislocation?
The prognosis of Kneecap Dislocation is usually good, if appropriate medical treatment is provided.
- In most cases, the affected individual can regain use of the injured knee within a few days
- In some cases of a more severe dislocation that necessitate surgery, it may take about 6 weeks for the condition to heal and to resume normal activity
How can Kneecap Dislocation be Prevented?
A few helpful tips to prevent Kneecap Dislocations:
- Use appropriate safety equipment, especially while participating in sports. Also, learn the correct sports techniques
- Wear seat-belt while driving
- Fall-proof the home; address slippery smooth surfaces that pose risk of falls
- Close supervision of children during their outdoor activities
What are certain Crucial Steps to be followed?
- Apply icepack to reduce swelling and take a suitable painkiller for pain
- Immobilize the joint
- Call 911 (or your local emergency number) or seek medical attention, based on the extent of injury
Related Articles
Test Your Knowledge
Asked by users
Related Centers
Related Specialties
Related Physicians
Related Procedures
Related Resources
Join DoveHubs
and connect with fellow professionals

0 Comments
Please log in to post a comment.