What are the other Names for this Condition? (Also known as/Synonyms)
- Jungle Rot
- Malabar Ulcer
- Tropical Phagedenic Ulcer
What is Tropical Ulcer? (Definition/Background Information)
- Tropical Ulcer is an infectious disease that results in the formation of painful and destructive skin lesions. It is caused by a variety of microorganisms, chiefly bacteria, and is mostly observed among younger populations in the tropical ‘economically-poorer’ regions of the world
- Tropical Ulcer is also variously known as Jungle Rot and Tropical Phagedena. The infection is transmitted through small open wounds on the leg or foot and is associated with overall poor health or recent illness
- The lesions that form may develop rapidly to involve deeper skin tissues, muscles, and bones, in the absence of adequate treatment. Tropical Ulcer has the potential to cause permanent disabilities including loss of limb
- The treatment involves the use of topical creams, administration of antibiotics, and surgical debridement/removal of damaged tissue. The prognosis of Tropical Ulcer is generally excellent with appropriate (early) treatment
Who gets Tropical Ulcer? (Age and Sex Distribution)
- Tropical Ulcer can affect individuals of any age group; however, a vast majority of cases are observed among children, teens, and young adults
- Even though both males and females are affected, males are affected more than females
- All races and ethnic groups are at risk. But, the condition is almost only seen in hot-wet areas - in the tropical and sub-tropical regions of the world
- In the country of Papua New Guinea, Tropical Ulcer is a very common condition
What are the Risk Factors for Tropical Ulcer? (Predisposing Factors)
In many cases, the onset of Tropical Ulcer is due to a combination of factors. The risk factors for infection may include:
- Individuals belonging to low income levels and poor socioeconomic status, particularly residing in country sides or rural regions, are vulnerable to the condition
- Individuals who are malnourished; poor nutrition is a high risk factor
- Farmhands, plantation workers, laborers, forest-dwellers - individuals who are regularly exposed to the ‘elements’ (unprotected from rain, sun, etc.)
- Children walking or playing barefoot in the high-risk areas
- Individuals with chronic conditions including stomach/intestinal worms, malaria, etc.
- Intravenous drug user having open skin injection wounds
- Individuals with weakened immune systems
It is important to note that having a risk factor does not mean that one will get the condition. A risk factor increases one’s chances of getting a condition compared to an individual without the risk factors. Some risk factors are more important than others.
Also, not having a risk factor does not mean that an individual will not get the condition. It is always important to discuss the effect of risk factors with your healthcare provider.
What are the Causes of Tropical Ulcer? (Etiology)
Tropical Ulcer is a polymicrobial infection that usually affects malnourished individuals against a background of a chronic disease or infection and poor immunity. The infection can be contagious.
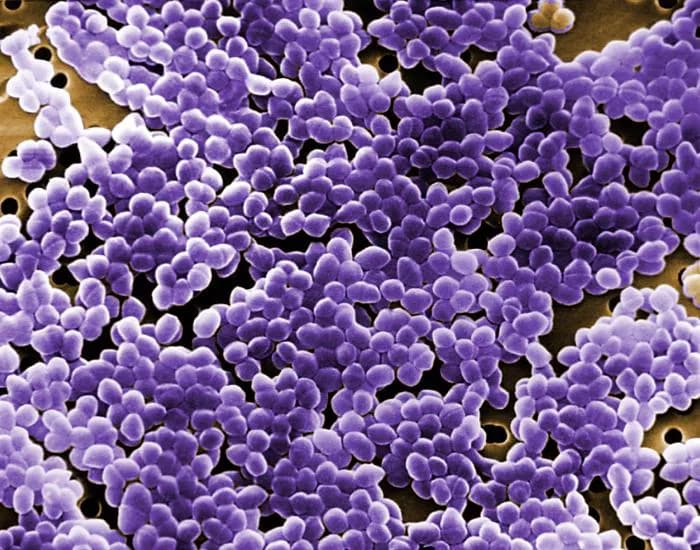
- Many bacterial species have been detected as being involved, notably Mycobacterium ulcerans, Enterococcus, and E. coli, including other anaerobic organisms and bacterial spirochetes
- If Mycobacterium ulcerans is detected, the disease is known as Buruli Ulcer. These are typically not painful
- Although, the most commonly seen bacterium is Bacillus fusiformis; another bacterium Treponema vincenti is observed in the later stages
- The start of infection is generally from an insect bite or minor injury to skin on the leg and poor hygiene. A higher incidence is observed during the wet (rainy) periods
- Following the onset of Tropical Ulcer, other superimposed infections involving staphylococcus and streptococcus bacteria may be noted
What are the Signs and Symptoms of Tropical Ulcer?
Tropical Ulcer usually affects the lower legs; a majority is observed below the knees on exposed skin areas. The ulcerative lesions may start from pre-existing cuts and sores (areas of minor trauma).
The signs and symptoms of Tropical Ulcer may be described as:
- The condition starts off as a small round superficial skin ulcer with purple-colored boundaries
- The lesions are characteristically yellowish, raised and poorly-bounded; the base of the ulcer appears necrotized
- Severe pain may be felt at the site of the ulcer
- The ulcers may remain stable for a long period of time. Or, they can progressively increase in size and involve larger areas of skin, which is often the case
- Over weeks, the ulcer may grow from a few mm to several cm in size - edges show thickening, while the center shows dead tissue (necrosis) that may turn black
- Pungent odor may emanate from the wound
The condition may be accompanied by fever and chills, sweating, general feeling of sickness, and fatigue.
How is Tropical Ulcer Diagnosed?
The following tests and procedures may be used to diagnose Tropical Ulcer:
- Complete physical examination with medical history evaluation
- Blood tests
- Imaging tests, such as X-rays, or CT and MRI scans, to study muscle and bone damage, if any
- Culture studies: Culture swabs for detecting the bacterial species involved
- Skin biopsy: A biopsy is performed and sent to a laboratory for a pathological examination. The pathologist examines the biopsy under a microscope. After putting together clinical findings, special studies on tissues (if needed) and with microscope findings, the pathologist arrives at a definitive diagnosis
- A differential diagnosis may be necessary to exclude certain infections that present similar symptoms such as:
- Atypical mycobacterial infections
- Cutaneous leishmaniasis
- Cutaneous tuberculosis
- Treponemal diseases of yaws, bejel, and pinta
- Pyoderma gangrenosum
- Venous stasis
Many clinical conditions may have similar signs and symptoms. Your healthcare provider may perform additional tests to rule out other clinical conditions to arrive at a definitive diagnosis.
What are the possible Complications of Tropical Ulcer?
The complications from Tropical Ulcer could include the following:
- Prolonged signs and symptoms
- Chronic ulcerative lesions that are recurrent
- If left untreated, the infection can involve and erode deeper skin and tissue layers affecting the tendons, muscles, periosteum (outer fibrous layer of bone) and bones. This can result in permanent and often severe scarring and disfigurement
- Gangrene formation
- Tetanus
- Bone infection (osteomyelitis) or bone inflammation (osteitis), which can lead to disabilities
- Amputation of limb or digit
- Tropical Ulcer may develop into squamous epithelioma after many years (over 10 years) and, in turn to squamous cell carcinoma (a malignant condition)
- There may be permanent skin color changes to blue/green/orange/red after healing of the ulcers
How is Tropical Ulcer Treated?
It is important to treat Tropical Ulcer during the initial stages, which can prevent its progression to severe and debilitating infection. The treatment measures may include:
- Topical application of aluminum diacetate, silver nitrate solution, or potassium permanganate - which in most cases stops further progression of the disease and causes the lesions to heal
- Prescription antibiotic medications include tetracycline and metronidazole
- In children below age 12 years, the antibiotic procaine G penicillin is recommended for a period of 2 to 4 weeks
- Nutritional supplementation may be needed to address any vitamin or mineral deficiencies
- Proper dressing of wounds and elevating limb, especially while sleeping or resting
- Debridement of larger ulcers
- Skin grafting and reconstructive surgery, if needed
- Amputation for severe bone and tissue infection, in rare cases
Some cases of Tropical Phagedenic Ulcers are known to rarely resolve on their own, in the absence of any treatment.
How can Tropical Ulcer be Prevented?
Prevention techniques in the high-risk areas for Tropical Ulcer may include:
- Protect feet while walking on the ground; use of proper footwear
- Wear protective clothing to prevent injuries and cuts while walking in tropical regions/forests
- Treat minor cuts and scratches on skin early
- Maintain overall good health and immunity
- Maintain proper hygiene; wash hands frequently, especially before eating and after going to toilet
- Seek proper treatment for pre-existing diseases and conditions that may result in a compromised immune system
Educate people staying in Tropical Ulcer prone regions about the condition; provide information on the measures they may take to prevent infection.
What is the Prognosis of Tropical Ulcer? (Outcomes/Resolutions)
The prognosis of Tropical Ulcer with early diagnosis and prompt treatment is generally excellent.
- Without treatment, the infection may progress rapidly and become chronic. The ulcers may persist for even 10 years or more
- In such cases, it can severely affect the muscles and bones resulting in amputation and/or permanent disability
Additional and Relevant Useful Information for Tropical Ulcer:
The following DoveMed website link is a useful resource for additional information:
https://www.dovemed.com/diseases-conditions/infection-center/
Related Articles
Test Your Knowledge
Asked by users
Related Centers
Related Specialties
Related Physicians
Related Procedures
Related Resources
Join DoveHubs
and connect with fellow professionals


0 Comments
Please log in to post a comment.