What are the other Names for this Condition? (Also known as/Synonyms)
- Libman-Sacks Disease
- Lupus
- Lupus Erythematosus Disseminatus
What is Systemic Lupus Erythematosus? (Definition/Background Information)
- Systemic Lupus Erythematosus (SLE or Lupus) is an autoimmune disorder that may affect any area of the body, such as the skin, joints, blood cells, kidneys, brain, heart, and lungs. Women are more commonly affected by SLE than men
- Autoimmune disorders cause the body to mistake normal healthy tissues and organs for dangerous foreign material and attack them leading to long-term chronic inflammation. The disease-causing autoantibodies can attack the tissues and organs. Also, lymphocytes (a form of white blood cells) can attack the tissues
- Such an attack by the body’s immune cells can be severe, resulting in significant signs and symptoms. The key symptoms depend upon the part of the body that is affected. Sometimes, early manifestations are observed on the skin. The classical symptoms of Systemic Lupus Erythematosus include a “butterfly-shaped” rash on the face and sensitivity to sunlight. Cutaneous lupus erythematosus (CLE) has findings mostly confined to the skin. It is a separate but related disease that overlaps with SLE
- Systemic Lupus Erythematosus may be diagnosed through physical examination, complete medical history, skin biopsy, and specialized blood tests. SLE frequently has cutaneous findings along with internal organ involvement, and hence, the cutaneous findings may be helpful in diagnosing the condition
- There is no cure for Systemic Lupus Erythematosus, but there are many treatment methods that may help control the flare-ups and other symptoms of the condition. There is no effective preventive method for SLE onset that is caused by genetic predisposition. Drug-Induced Lupus can be prevented by avoiding known medications implicated in causing Lupus-like symptoms
- Systemic Lupus Erythematosus can range in severity from mild to very severe. The prognosis depends on the severity of the disorder and also its response to therapy. Individuals who respond well have a better prognosis than those who do not respond well to treatment
Who gets Systemic Lupus Erythematosus? (Age and Sex Distribution)
- Individuals of any age may be affected by Systemic Lupus Erythematosus (SLE), but it is more commonly seen between the ages of 10 and 50 years
- Women are more prone than men to be affected by SLE
- A higher prevalence rate is noted among people of African American and Asian descent
What are the Risk Factors for Systemic Lupus Erythematosus? (Predisposing Factors)
The risk factors associated with Systemic Lupus Erythematosus (SLE) may include:
- Female gender
- Individuals of African American and Asian race
- Genetic predisposition, with family members with SLE
- Medication that has been known to cause Drug-Induced Lupus
It is important to note that having a risk factor does not mean that one will get the condition. A risk factor increases one’s chances of getting a condition compared to an individual without the risk factors. Some risk factors are more important than others.
Also, not having a risk factor does not mean that an individual will not get the condition. It is always important to discuss the effect of risk factors with your healthcare provider.
What are the Causes of Systemic Lupus Erythematosus? (Etiology)
The exact cause of Systemic Lupus Erythematosus is not fully known or understood.
- The use of some drugs may cause the onset of Drug-Induced Lupus Erythematosus
- Some individuals may have a genetic predisposition for the condition; which may then be triggered by infections, certain drugs, or on exposure to the sun
What are the Signs and Symptoms of Systemic Lupus Erythematosus?
The signs and symptoms of Systemic Lupus Erythematosus (SLE) may vary from one individual to another and can be mild or severe. These may include:
- A rash on the face in the shape of a “butterfly” Involving the upper cheeks and skin around the nose
- Other skin findings may be noted
- Fatigue
- Low-grade fever
- Loss of appetite
- High blood pressure
- Anemia
- Muscle pain
- Hair loss (alopecia)
- Arthritis; joint pain and inflammation
- Oral and nasal ulcers
- Sensitivity to sunlight
- Inflammation of the lining of the lungs and heart
- Poor kidney function with weight gain from fluid retention; visible changes in the urine
- Swollen lymph nodes
- Memory problems, confusion
- Chest pain while taking deep breaths
- Eye inflammation, dry eyes, and eyelid rashes
How is Systemic Lupus Erythematosus Diagnosed?
The American College of Rheumatology (ACR) has established a set of 11 criteria to make (or rule out) the diagnosis of Systemic Lupus Erythematosus (SLE). These criteria are closely related to the symptoms of Lupus, which include:
- Skin signs and symptoms of Lupus:
- Malar rash (butterfly-shaped rash stretching across the cheeks and nose)
- Photosensitivity rash due to sunlight
- Discoid (red and raised) rashes on the skin
- Mouth and nose signs and symptoms of Lupus that include oral and nasal ulcers
- Joints signs and symptoms of Lupus, such as joint pain or arthralgia
- Blood changes in Lupus, including decreased red blood cells, white blood cells, and platelets
- Renal signs and symptoms of Lupus that may range from proteinuria (presence of proteins in urine) to end-stage kidney disease
- Brain signs and symptoms of Lupus, such as seizures, stroke, meningitis (infection of the protective coverings of the brain), and psychosis
- Heart and lung signs and symptoms of Lupus that include chest pain, pulmonary hypertension, pleuritis, myocarditis (inflammation of heart muscle), or pericarditis
- Serology test: Antinuclear antibody (ANA) positive
- Serological blood test: Anti-double-stranded DNA (ds-DNA) positive
Out of these 11, 4 criteria are needed to make a diagnosis of SLE.
In addition to the above 11 criteria, other tests may help determine the involvement of various organs. The healthcare provider may choose the tests depending on the patient’s presentation (signs and symptoms and medical history). Some of these include:
- Routine blood testing: Erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) blood tests
- Blood chemistry panels
- Lupus panel testing with additional tests, including rheumatoid factor, anti-histone antibodies, anti-ro (SSA) and anti-la (SSB) antibodies, antiphospholipid antibodies, anti-Smith, anti RNP, and LAC (aCL, abeta2GPI)
- Complement levels- C3, C4, CH50
- Body fluid analysis such as pleural (lung cavity) fluid and pericardial (heart cavity) fluid analysis
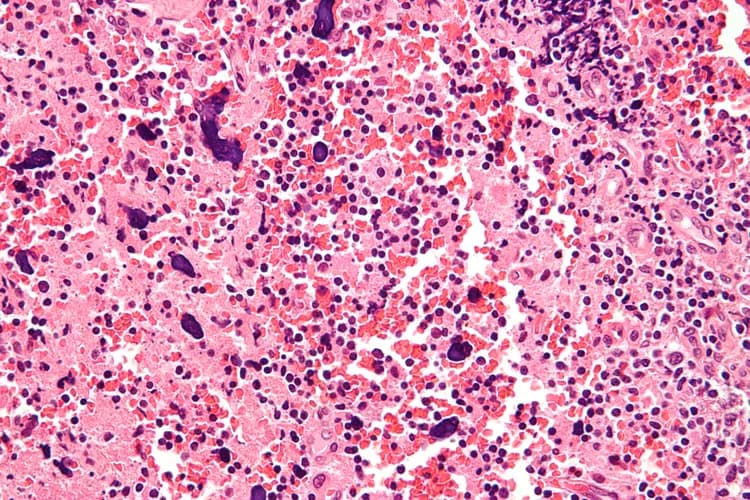
- Tissue biopsies of the affected organs, such as skin and kidney biopsies
- Biopsies are processed with routine and immunologic stains
Many clinical conditions may have similar signs and symptoms. Your healthcare provider may perform additional tests to rule out other clinical conditions to arrive at a definitive diagnosis.
What are the possible Complications of Systemic Lupus Erythematosus?
The complications that might occur due to Systemic Lupus Erythematosus (SLE) include:
- Complications with pregnancy, such as early termination and stillbirth; repeated miscarriages
- Blood clots in the legs and lungs (thrombosis and thromboembolism)
- Kidney failure
- Hemolytic anemia (destruction of red blood cells)
- Inflammation of the heart (pericarditis and myocarditis) and inflammation of the blood vessels (vasculitis)
- Fluid around the heart and lungs (pericardial effusion and pulmonary effusion, respectively)
- Brain inflammation leading to confusion or stroke
- Spinal cord inflammation with possible paralysis (transverse myelitis
- Low platelet count in blood resulting in clotting complications (thrombocytopenia)
- Women with SLE may be at an increased risk for heart disease (SLE-induced heart damage), including heart attack
- Increased risk of developing cancers such as leukemia and lymphoma (SLE-induced lymphoma and leukemia)
- There is also an increased risk of breast cancer
How is Systemic Lupus Erythematosus Treated?
There is currently no cure for Systemic Lupus Erythematosus (SLE). The treatment undertaken consists of decreasing inflammation and autoimmune activity in the body and minimizing the occurrence of flare-ups.
The following medications have been found to be helpful in the treatment of SLE:
- Non-steroidal anti-inflammatory drugs (NSAIDs)
- Systemic and topical corticosteroids
- Antimalarial medications, including hydroxychloroquine, quinacrine, and chloroquine
- Immunosuppressive drugs that include methotrexate, azathioprine, cyclophosphamide, mycophenolate, mofetil, cyclosporin, voclosporin, thalidomide, lenalidomide, and pomalidomide
- Biologic drugs, such as rituximab, obinutuzumab, eculizumab, and belimumab
A procedure termed plasmapheresis may be intermittently used to remove autoantibodies from blood.
How can Systemic Lupus Erythematosus be Prevented?
- Currently, there is no effective preventive method for the onset of Systemic Lupus Erythematosus
- Flare-ups can be prevented by managing medications, avoiding sun exposure, utilizing suitable sunscreens and clothing (to cover up), and closely monitoring the symptoms
What is the Prognosis of Systemic Lupus Erythematosus? (Outcomes/Resolutions)
Systemic Lupus Erythematosus (SLE) is an autoimmune disorder that can range in severity from mild to severe to fatal; the outcome of the disorder depends on the severity of the disease. Through proper treatment and monitoring of the condition, many individuals with SLE are able to lead normal, healthy lives while managing flares.
- SLE tends to be more active in younger individuals under the age of 40 years and in those who are newly diagnosed with the condition
- Pregnant women are often able to deliver at full term safely. It is essential that treatment during pregnancy is adequate, with close monitoring of both the mother and the developing baby by a team with experience in this patient cohort
- Drug-Induced SLE is infrequent (less than 5% of the cases) and most often resolved upon discontinuation of the medication
Additional and Relevant Useful Information for Systemic Lupus Erythematosus:
- According to the Lupus Foundation of America, approximately 5 million people worldwide suffer from a form of Lupus
- For patients with kidney disease, the Six-Class scale based on microscopic findings has useful treatment and prognostic criteria
Related Articles
Test Your Knowledge
Asked by users
Related Centers
Related Specialties
Related Physicians
Related Procedures
Related Resources
Join DoveHubs
and connect with fellow professionals


0 Comments
Please log in to post a comment.