What are the other Names for this Condition? (Also known as/Synonyms)
- Progressive Systemic Sclerosis
- Skin Thickening due to Scleroderma
- Systemic Sclerosis
What is Scleroderma? (Definition/Background Information)
- Scleroderma is a chronic connective tissue disorder of unknown cause that most commonly affects young and middle-aged women. The term Scleroderma indicates “hard skin”; “sclera” means hard, and “derma” means skin. The condition is also termed Systemic Sclerosis
- Connective tissues provide structural support to the organs and skin. Individuals with Scleroderma have thick or hard connective tissue. The signs and symptoms are variable and depend upon the Scleroderma type. Systemic Sclerosis manifests in two forms - limited and diffuse
- The most typical skin findings seen in both limited and diffuse forms, include firm bound down skin of the fingers, Raynaud’s phenomenon of blanching of fingers in response to cold exposure, and tighter, wrinkle-free skin of the face
- The complications of diffuse Systemic Sclerosis include the hardening of organs due to abnormal fibrosis of the tissue that can severely affect the organ function of the heart, lungs, and kidneys. Limited Systemic Sclerosis, previously called CREST syndrome, besides the skin findings, involves the esophagus, lungs, and intestines
- There is currently no cure for Scleroderma. But medications, therapy, and surgery may be used to control the symptoms and prevent complications. The treatment measures are dependent upon the tissues or organs affected
- The way Scleroderma changes and progresses over time vary among individuals. The rapidity of progression of signs and symptoms and the organs involved affects the prognosis. Typically, individuals who respond to treatment have a better prognosis than individuals who do not respond well to treatment
There is currently a debate about how Scleroderma should be classified. A majority believe that it should be classified as an autoimmune rheumatic disorder. Due to this, many researchers believe that the damage is caused by immune cells mistakenly attacking one’s own healthy tissue.
Scleroderma can be classified into two broad categories, which include Localized Scleroderma and Systemic Scleroderma:
- Localized Scleroderma:
- It only affects the skin structures and does not cause harm to the other major organs
- There are two types of Localized Scleroderma, namely Morphea and Localized Linear Scleroderma
- Systemic Scleroderma:
- It affects the skin, the tissues beneath the skin, major organs, and blood vessels
- Systemic Scleroderma also has two different types, namely Limited Systemic Scleroderma and Diffuse Systemic Scleroderma
Who gets Scleroderma? (Age and Sex Distribution)
- Individuals of any age (both adults and children) can be affected by Scleroderma; however, this connective tissue disorder usually occurs from ages 25 to 55 years
- Scleroderma is much more prevalent among females than males with a prevalence ratio of 4:1
- A majority of Localized Scleroderma cases appear before age 40, whereas Systemic Scleroderma cases often occur in individuals between the ages of 30 and 50
- Scleroderma is known to occur worldwide in all races and ethnic groups
- Systemic Scleroderma is more common in Native Americans and African Americans than individuals of European decent
What are the Risk Factors for Scleroderma? (Predisposing Factors)
The risk factors for Scleroderma may include:
- Gender: Women are more likely than men to be affected by Scleroderma
- Some studies have shown that individuals who have worked with or been exposed to silica dust and polyvinyl chloride (PVC) may have an increased incidence of the same
It is important to note that having a risk factor does not mean that one will get the condition. A risk factor increases one’s chances of getting a condition compared to an individual without the risk factors. Some risk factors are more important than others.
Also, not having a risk factor does not mean that an individual will not get the condition. It is always important to discuss the effect of risk factors with your healthcare provider.
What are the Causes of Scleroderma? (Etiology)
The exact cause of Scleroderma is unknown. Research is being currently performed to identify the relevant causal factors.
- Many researchers believe that Scleroderma is an autoimmune disorder where the body’s immune system mistakenly attacks healthy tissues resulting in damage of the tissues and organs
- Supporting the immune basis of Scleroderma is the pact that autoantibodies are detected in the blood of patients, and immune system cells are found infiltrating the affected tissues
- Some studies have revealed that there may be a higher risk for the condition in those with occupational exposure to chemicals such as silica dust and PVC
However, research has established the following on Scleroderma:
- It is not an infectious or contagious condition, which means that it cannot be passed on from one individual to another through contact. It is also not a malignant condition
- About 1.5 % of Systemic Sclerosis patients have a first degree relative with the same condition, which means they have a parent, a full sibling, or a child with Systemic Sclerosis
- However, this association has not yet led to a proven genetic linkage or specific gene change
What are the Signs and Symptoms of Scleroderma?
The signs and symptoms of Scleroderma can vary greatly from individual to individual. This might create confusion in many since one may not have all of the signs and symptoms described for Scleroderma. In some cases, Scleroderma can be severe with significant signs and symptoms and complications.
The skin-related signs and symptoms of Scleroderma, both limited and diffuse can include:
- Hardening and tightening of the skin of the fingers and up the hands and face. This can cause restricted movement of the affected area of the skin. In SSc-Limited type, the sclerotic skin is limited to the hands and feet. In SSc-Diffuse type, the distribution is more extensive; it extends up the arms and legs, involves the face, and even the trunk
- Raynaud’s phenomenon: In Raynaud’s phenomenon, the blood vessels of the hands and feet constrict either due to cold weather or when the individual is anxious. This constriction of blood vessels causes severe pain in the hands and feet. It also results in skin color changes in the fingers and toes
- The facial skin becomes firmer and tighter. Older patients with Scleroderma have fewer wrinkles than would be expected for their age
- Irregular pigmentation of skin
- Ulcer formation at the tips of fingers from poor blood flow and inflexibility when subjected to trauma
- Telangiectasias (visible superficial broken blood vessels) appear on the face, often many in numbers
- The skin at the base of the fingernails shows many superficial dilated blood vessels
- Small hard deposits of calcium form on the skin of the fingers
- Joint stiffness and pain in the hands and feet
Limited Cutaneous Systemic Sclerosis (lcSSc) has fewer signs and symptoms related to internal organs than the diffuse type. The issues with lcSSc are generally:
- Esophageal immobility, with difficulty swallowing
- Pulmonary arterial hypertension affecting the lungs and putting a strain on heart function. This can lead to coughing
- These patients can also present fibrosis of lungs leading to difficulty breathing seen in the diffuse type, but less frequently though
- Overall, the progression of both skin and internal organ involvement is slower than in the diffuse type
Diffuse Cutaneous Systemic Sclerosis (dcSSc) has more extensive, serious, and rapidly progressive internal organ involvement. dcSSc also shows all the same skin findings listed under lcSSc, so those should be reviewed. Internal organ system involvement is more severe and more rapidly progressive.
- The lungs become stiff with excess collagen, leading to shortness of breath
- Constipation or diarrhea based on poor intestinal motility
- Malabsorption of nutrients
- Decreased renal (kidney) function with eventual complete renal failure possible
- The changes in kidney function, as well as arterial involvement, can lead to high blood pressure
- Heart failure can occur because the collagen infiltrating the muscle leads to stiffness and pump failure
- Pulmonary arterial hypertension can put addition strain on the heart
How is Scleroderma Diagnosed?
Scleroderma can be difficult to diagnose, as other conditions may have similar signs and symptoms. The presence of common symptoms or skin that thickens quickly makes it easier to diagnose Scleroderma. The following tests and procedures may be used to diagnose Scleroderma:
- A thorough physical examination along with a complete medical and family history
- Blood tests, such as anti-nuclear antibody (ANA) panel, erythrocyte sedimentation rate (ESR), complete blood count (CBC), rheumatoid factor (RF) levels, antibody testing for other autoimmune disorders, and other tests
- Kidney function tests including creatine level, BUN level, glomerular filtration rate (GFR), and urine analysis
- Chest X-ray and CT scan of the lungs to determine the extent of lung scarring (pulmonary fibrosis)
- Pulmonary function test (PFT)
- Electrocardiogram and echocardiogram to determine the extent of heart involvement caused by heart scarring (cardiac fibrosis)
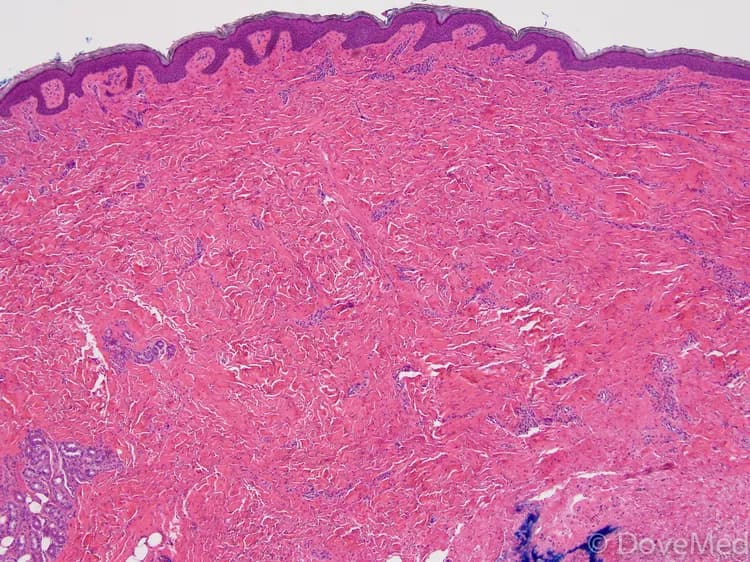
- Skin biopsy: Cells and tissues are examined by a pathologist under a microscope. Pathological examination is generally considered to be a ‘gold standard’ for a definitive diagnosis. The pathologist arrives at a diagnosis after analyzing pathology findings along with clinical information of the patient. A pathologist may perform special studies on tissue samples to aid in the final diagnosis
Many clinical conditions may have similar signs and symptoms. Your healthcare provider may perform additional tests to rule out other clinical conditions to arrive at a definitive diagnosis.
What are the possible Complications of Scleroderma?
Complications due to Scleroderma can range from mild to severe and could include:
- Scarring of lung tissue can occur with reduced lung function, lessened ability to breathe, and decreased tolerance for physical activity. This is known as pulmonary fibrosis. One may also develop hypertension (high blood pressure) in the arteries that supply the lungs, known as pulmonary hypertension
- If Scleroderma affects the kidneys, there may be elevated blood pressure and protein in urine. More severe kidney complications could include renal crisis, leading to rapid kidney failure
- If Raynaud’s phenomenon that develops from Scleroderma is severe enough, then restricted blood flow at the fingertips can cause damage to the tissue, leading to the formation of pits or skin ulcers. In severe cases, amputation may be necessary to avoid gangrene formation
- Increased blood pressure can also raise the pressure on the heart’s right side and cause wear and tear, leading to scarring of heart tissue. This condition increases the risk for cardiac arrhythmias and congestive heart failures
- Tightening of the facial skin to a great degree can cause the mouth to become narrower and smaller, making it difficult to clean the teeth. It is common for individuals with Scleroderma to produce inadequate amounts of saliva, which also increases the risk for dental decay
- Complications with the digestive system can occur leading to acid reflux and swallowing difficulties. Alternating episodes of constipation and diarrhea are often seen
- Men may experience erectile dysfunction, whereas women experience decreased lubrication and constriction of the vaginal opening
How is Scleroderma Treated?
Currently, Scleroderma is a condition that has no cure but is managed through medications, lifestyle modifications, therapy, and surgery. These measures can help control symptoms and prevent complications. The skin-related signs and symptoms may fade on their own within 3-5 years. Systemic Scleroderma usually worsens over time, as it affects the internal organs.
The treatment options for Scleroderma include:
- Occupational or physical therapists can help individuals with Scleroderma manage pain, increase their strength, and uphold their independence in their everyday lives
- Surgery is considered to be a last resort. Amputation may be necessary in patients whose finger ulcers have developed gangrene. Those with high blood pressure in the lung arteries due to Scleroderma may need lung transplants
The following are the treatment measures for Raynaud’s phenomenon:
- Cessation of smoking: Smoking causes constriction of blood vessels, which causes an increase in symptoms due to Raynaud’s phenomenon
- Keeping hands and feet warm (particularly in colder temperatures), taking medications for anxiety, taking medications that open up the small blood vessels, all are factors that cause a better blood flow to the hands and feet (vasodilators)
- These medications include calcium channel blockers, phosphodiesterase type 5 inhibitors, alpha adrenergic blockers, angiotensin II receptor blockers, endothelin receptor antagonists, and serotonin uptake inhibitors
- Regular exercise can also help with blood flow to the hands and feet
Treatment measures for painful joints with or without restricted movements include:
- Regular exercise and stretching that helps loosen up the joints
- Pain medication to reduce joint pain
Treatment measures for skin signs and symptoms include:
- Regular use of sunscreen, avoiding hot showers, and regular exercising
- For individuals living in a dry climate with low humidity, the use of a humidifier can help with the signs and symptoms
- Antibiotic ointment for fingertip ulcers
- Low dose aspirin, clopidogrel, or IV prostanoid treatment
- Plastic surgery may be an option for cosmetic issues; a plastic surgeon can advise on the available treatment options
- It is always important to follow the physician’s advice and take the prescribed medication regularly
- A therapist or certain support groups may be consulted on the variety of social issues that can be caused by Scleroderma, which include self-esteem issues, depression, anxiety, and relationships with friends, family, and partners
- UVA1 phototherapy has been investigated for Scleroderma skin findings. It is not widely available
- Oral medications methotrexate, D-penicillamine, minocycline, and mycophenolate mofetil are used with variable success
Treatment measures for dry mouth and dental issues include:
- Individuals with Scleroderma could experience tightening of the facial skin that may prevent adequate oral care; this can result in the development of tooth decay
- The following measures can help decrease the signs and symptoms:
- Regular brushing and flossing of teeth
- Regular dental check-ups
- Keeping mouth wet by frequently sipping water
- Avoid mouthwash that contains alcohol, since alcohol in mouthwashes can cause dryness of the mouth
Individuals with Scleroderma can have a variety of gastrointestinal symptoms such as diarrhea, constipation, excess gas formation, difficulty in swallowing, and heartburn. The following treatment measures can help in such cases:
- Medication for heart burn, diarrhea, and constipation
- Eating small and frequent meals, which helps with movement of the food and digestion
- Avoidance of spicy and fatty foods, alcohol, and caffeinated drinks
- Avoiding food items that are hard and difficult to swallow
Individuals with Scleroderma can have a variety of signs and symptoms related to the lungs, which include difficulty in breathing due to excessive scarring and high blood pressure in the lungs (pulmonary hypertension). Lung infection, in an individual with poor lung function, may result in severe complications such as severe pneumonia.
The following treatment options may be beneficial:
- It is important to see a pulmonologist on a regular basis to manage one’s signs and symptoms
- Getting regular flu shots and pneumonia shots will help prevent unnecessary infection
Individuals with heart and kidney symptoms should get regular health check-ups from a cardiologist and nephrologist respectively.
How can Scleroderma be Prevented?
Currently, there are no specific methods or guidelines to prevent Scleroderma. However, through proper dietary and lifestyle changes, some of the signs and symptoms may be controlled.
What is the Prognosis of Scleroderma? (Outcomes/Resolutions)
- Scleroderma changes and progresses over time; this varies from one individual to another
- Some individuals respond well to treatment and generally have a better prognosis than those who do not respond well to treatment
- The prognosis for individuals with Systemic Scleroderma (both limited and diffuse types) is worse than with Localized Scleroderma (both morphea and linear types)
- The prognosis for Limited Cutaneous Systemic Sclerosis is better than Diffuse Cutaneous Systemic Sclerosis
- Generally, Morphea and Linear Scleroderma have an excellent prognosis
Additional and Relevant Useful Information for Scleroderma:
- Research is currently underway to identify and understand more about Scleroderma. Studies are being completed to understand the genes that may be involved with the development of the condition, medicines to prevent the skin from thickening, and to treat the kidney/lung conditions, as well as medicines to completely treat Scleroderma
Scleroderma used to be called progressive systemic sclerosis, but this term is no longer used since Scleroderma does not always progress by nature. This means that the signs and symptoms do not progress with equal severity in all individuals
Related Articles
Test Your Knowledge
Asked by users
Related Centers
Related Specialties
Related Physicians
Related Procedures
Related Resources
Join DoveHubs
and connect with fellow professionals


0 Comments
Please log in to post a comment.