Pulmonary Tuberculosis
What are the other Names for this Condition? (Also known as/Synonyms)
- Lung TB
- Pulmonary TB
- Respiratory Tuberculosis (RTB)
What is Pulmonary Tuberculosis? (Definition/Background Information)
- Pulmonary Tuberculosis (TB) is a contagious bacterial infection of the lungs, which is caused by Mycobacterium tuberculosis. This infection is reported worldwide and can affect all individuals
- The disease spreads through respiratory droplets from an infected individual, when the individual coughs or sneezes. It commonly affects individuals with weak immune system, infants, and elderly adults
- Individuals with Pulmonary Tuberculosis may present signs and symptoms including cough, fever, and weight loss. It can cause permanent lung damage, if early treatment is not provided
- Pulmonary TB is normally treated with a combination of 4 antibiotics over a period of 6 months. The treatment has to be followed for the entire prescription period
- Since tuberculosis is a highly contagious disease, prevention is best achieved by avoiding individuals infected with TB, mainly in crowded and closed spaces
- The prognosis of this infectious disease is generally good, if it is diagnosed early, and the treatment is followed through properly and completely
Who gets Pulmonary Tuberculosis? (Age and Sex Distribution
- Pulmonary Tuberculosis can affect individuals of any age; however, infants and children, the elderly, and immunocompromised individuals are easily infected
- There is no gender predilection; both males and females are affected
- The condition is seen worldwide, although people living in low-income and middle-income countries are affected the most (per World Health Organization).
What are the Risk Factors for Pulmonary Tuberculosis? (Predisposing Factors)
The following are some known risk factors associated with Pulmonary Tuberculosis:
- Age: The elderly individuals and infants are at an increased risk
- A weak immune system, due to AIDS infection, chemotherapy, and diabetes (TB is the leading cause of death in HIV infected patients)
- Frequent contact with infected individuals
- Poor nutritional status
- Living in crowded places such as slums, prisons, juvenile homes, military quarters, etc.
- Poor sanitary conditions
- Working in the medical profession; doctors, nurses, social workers, or healthcare providers are at a high risk
- Excessive use of drugs and alcohol
- Travelling to geographical regions, such as Latin America, Africa, Asia, parts of Europe and Russia, where untreated Pulmonary Tuberculosis is common
- Chronic lung disease
- Cigarette smoking
- Use of certain medications (corticosteroids and infliximab) that suppress the immune system
It is important to note that having a risk factor does not mean that one will get the condition. A risk factor increases ones chances of getting a condition compared to an individual without the risk factors. Some risk factors are more important than others.
Also, not having a risk factor does not mean that an individual will not get the condition. It is always important to discuss the effect of risk factors with your healthcare provider.
What are the Causes of Pulmonary Tuberculosis? (Etiology)
- Pulmonary Tuberculosis is an infection of the lungs that is caused by the bacteria Mycobacterium tuberculosis (M. tuberculosis)
- The disease is transmitted by inhaling contaminated respiratory droplets that are released into air through cough and sneeze, by an infected individual
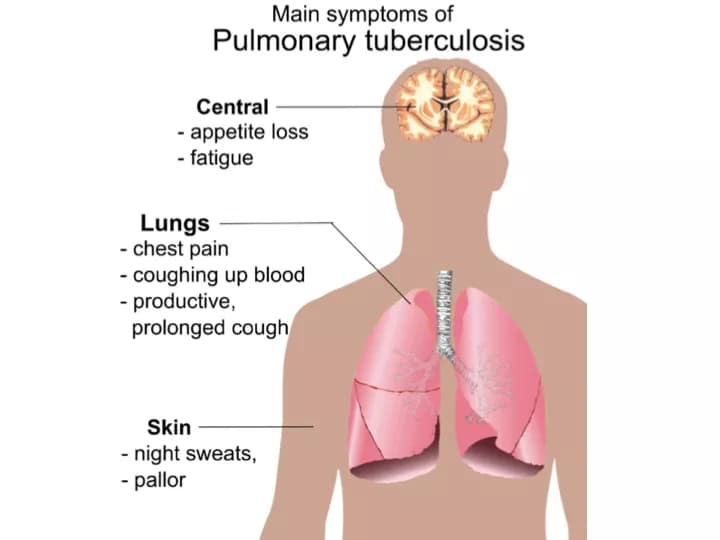
What are the Signs and Symptoms of Pulmonary Tuberculosis?
The signs and symptoms manifested by Pulmonary Tuberculosis include:
- Cough with thick sputum; the sputum may contain blood
- Tiredness, fatigue
- Weight loss
- Fever, night sweats
- Shortness of breath, wheezing
- Chest pain
In some cases, no symptoms may be observed even though the TB bacterium is present in the body. Such a state is termed as latent tuberculosis. Latent TB may turn into an active form of TB with characteristic signs and symptoms, if the immunity weakens.
How is Pulmonary Tuberculosis Diagnosed?
The diagnosis of Pulmonary Tuberculosis may involve the following tests and procedures:
- Complete evaluation of medical history
- Thorough physical examination, which may reveal the following:
- Unusual breathing sounds such as crackles or wheezing
- Clubbing of finger or toes in those with advanced disease
- Unintended, severe weight loss
- TB skin test, also known as tuberculin test or purified protein derivative (PPD) test
- The skin test involves an injection of a small amount of tuberculin (which contains the tuberculosis bacteria) into the lower arm
- 48-72 hours after the injection, a healthcare provider examines the site of injection
- If there is swelling in the area, the test is positive and it indicates that the individual is infected with Mycobacterium tuberculosis
- If no swelling is noted, the test is negative and the individual is not infected
- TB screening blood test, also called interferon-gamma release assay or IGRA:
- A blood sample is collected and tested, to see how the individual’s immune system responds to the tuberculosis bacteria
- Like the TB skin test, a positive test indicates the presence of TB bacteria in the individual; a negative test indicates that there is no infection
- If the blood or skin TB test is positive, follow-up tests are conducted to confirm latent or active infection:
- Chest X-ray
- Chest CT scan
- Bronchoscopy: A technique for visualizing the insides of the airways for diagnostic purposes
- Sputum examination for culture: In this test, bacteria are made to grow in the lab by providing an artificial medium
- Lung biopsy (performed in very rare cases)
Many clinical conditions may have similar signs and symptoms. Your healthcare provider may perform additional tests to rule out other clinical conditions to arrive at a definitive diagnosis.
What are the possible Complications of Pulmonary Tuberculosis?
The complications of Pulmonary Tuberculosis may include:
- Permanent lung damage, if not treated early
- Spread of infection to other organs of the body such as to the intestine, liver, ovaries, and uterus
- Side effects from medicines used in the treatment of TB, such as:
- Liver abnormalities
- Changes in vision
- Orange or brown colored tears or urine
- Skin rashes
How is Pulmonary Tuberculosis Treated?
The treatment for Pulmonary Tuberculosis is based on whether the affected individual has a latent or an active TB infection:
- The treatment for TB infection involves the use of antibiotics to destroy the bacteria causing the infection. The treatment regimen may vary between latent and active infections. Whereas both are treated with antibiotics, an active TB disease may require a combination of drugs for a longer time period to completely rid the body of the pathogen. The type of medication, dosage, combination of drugs and duration of treatment are determined by the healthcare provider, based upon each individual’s particular health condition and other factors (such as age, pre-existing medical conditions, etc.)
- Directly observed therapy (DOT): Here, the treatment is directly supervised by a healthcare provider, who provides each dose of the prescribed (oral) medication, and ensures that it is swallowed by the patient (this may even be on a daily basis). The WHO recommends DOTS (directly observed treatment, short-course) as the best and complete curative method for TB infection
- It is extremely important to take the full regimen of medications, so that the bacteria may be eliminated from an individual’s body. Otherwise, the infection may linger and become active later on.
Additionally, inappropriate or insufficient treatment can lead to the development of multidrug resistant forms of the TB-causing bacterium.
- A multidrug resistant Tuberculosis (MDR-TB) develops when:
- The prescribed drug course/regimen is not followed properly
- The drugs being used have not been formulated properly, or are of poor quality
- Improper storage of drugs takes place, such that their efficiency is compromised
- Stopping drugs prematurely when the symptoms improve, without regard for the prescribed treatment duration
- The MDR-TB is resistant to at least 2 of the most effective drugs to treat the disease. This form of disease is more difficult to treat
- A form of disease known as extreme drug-resistant TB (XDR-TB) may develop when the bacterium develops resistance to several of the most effective drugs against TB
How can Pulmonary Tuberculosis be Prevented?
Pulmonary Tuberculosis is a preventable and curable infection. The preventive measures may include:
- Avoid contact with infected individuals, especially in closed and crowded areas. If such a contact is unavoidable, then proper respiratory protective equipment, such as a mask, should be used
- Getting vaccinated against TB - vaccines called Bacilli Calmette-Guerin (BCG) are available against the disease. However, the effectiveness of the vaccine is currently being debated upon. BCG has been shown to reduce the rate of tuberculosis in children in developing countries
- Skin testing in high-risk population or in individuals who have been exposed to the disease
- Getting treated once an individual has come into active contact with TB-infected individuals (i.e., those having confirmed tuberculosis infection)
- Getting treatment for any underlying medical condition(s) that may decrease immunity in the individual
Regular medical screening at periodic intervals with tests, and physical examinations are crucial, and highly recommended (for prevention and early diagnosis).
What is the Prognosis of Pulmonary Tuberculosis? (Outcomes/Resolutions)
- The prognosis of Pulmonary Tuberculosis is good with treatment using medications, which are taken regularly and for the entire length of the prescribed period. The symptoms usually start to subside with 2-3 weeks of treatment
- Without proper treatment, the infection may worsen and spread from the lungs to other body parts, and evolve into disseminated disease. Complications arising from untreated disease may be fatal
- In individuals with HIV infection and other conditions that weaken the immune system, the prognosis depends on many factors and is usually guarded
Additional and Relevant Useful Information for Pulmonary Tuberculosis:
- According to the World Health Organization (WHO), after HIV/AIDS, tuberculosis is the leading global killer caused by a single infectious pathogen. Annually, nearly 1.5 million individuals die of this disease and over 9 million are affected
- The evolution of multi-drug resistant tuberculosis (MDR-TB) is a significant public health concern around the world
Related Articles
Test Your Knowledge
Asked by users
Related Centers
Related Specialties
Related Physicians
Related Procedures
Related Resources
Join DoveHubs
and connect with fellow professionals

0 Comments
Please log in to post a comment.