What are other Names for this Condition? (Also known as/Synonyms)
- Bed Sores
- Decubitis Ulcers
- Pressure Ulcers
What is Pressure Sores? (Definition/Background Information)
- A Pressure Sore is caused by constant rubbing or pressing against a certain area of skin resulting in its break down. This prolonged pressure reduces blood flow in that area and injures the surface skin and its underlying tissues
- Pressure Sores are also commonly known as Bed Sores, which can occur from remaining in the same position for too long, such as being bedridden for a prolonged duration of time
- These sores commonly form on skin that covers the bony areas or where the skin folds over itself. The most common sites for Pressure Sores are the back of the head, the back of the ears, the shoulders, the elbows, the lower back, the buttocks, the hips, the inner knees, and the heel
- Most Pressure Sores occur in individuals admitted to hospitals. In fact, studies indicate that Bed Sores can affect up to 5% of the hospitalized individuals
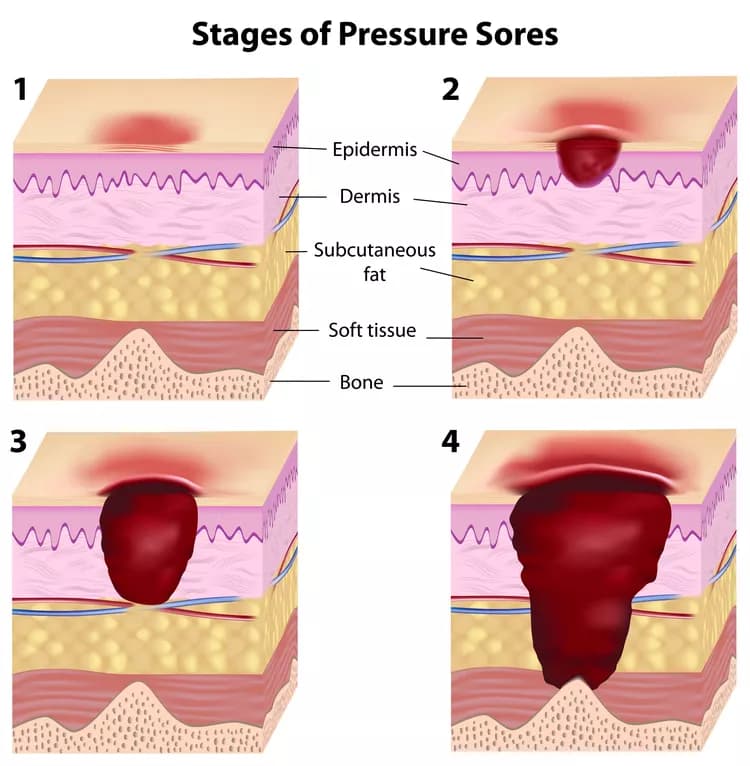
- Pressure Sores are categorized into 4 different stages from the first stage, which is generally mild to the final stage, that potentially results in an exposure of bones
- The treatments differ with each stage. The process of treatment includes cleaning and dressing the affected region, removing damaged (infected or dead) tissues, managing pain, antibiotic therapy, and exercising
- Early stages of Bed Sores can heal within several weeks through conservative care, but later stages are more difficult to treat. Pressure Sores usually take a long time to heal, especially if the individual was immobile for a long period that resulted in severe infections
- Pressure Sores may be prevented through changing positions of immobilized individuals frequently, keeping the skin dry and clean, and exercising to increase blood circulation
- The normal behavior of changing positions while sleeping is triggered in response to discomfort triggered by tissue responses to low blood flow and oxygen. Turning from side to side or other innate repositioning permits the previously compressed tissues to reperfuse. Any interruption of this cycle is the underlying cause of Pressure Sores
Who gets Pressure Sores? (Age and Sex Distribution)
- Pressure Sores are more commonly seen in older adults, although individuals of any age can be at risk for the condition
- No gender preference is noted and both males and females are affected
- All racial and ethnic groups are affected and no specific preference is observed
What are the Risk Factors for Pressure Sores? (Predisposing Factors)
Any condition that leads to prolonged bed rest or confinement is a big risk factor for the development of Pressure Sores. The immobility may occur due to:
- Coma
- Sedation
- Post-surgery: After a major surgery requiring prolonged bed rest
- Severe illness
- Paralysis
- Poor health, such as individuals with uncontrolled congestive heart failure, poorly-controlled diabetes, immunosuppression, etc.
Some other associated risk factors for Pressure Sores include:
- Age: Older adults have more vulnerable skin
- Smoking status: Individuals who smoke (especially chronic smokers) have poor wound healing capacity
- Lack of sensory perception due to neuropathy: This causes individuals to have altered touch and pain sensation resulting in increased risk to skin damage
- Longstanding diabetes
- Alzheimer’s disease
- Heart failure
- Various health conditions causing poor blood flow or blood circulation
- Weight loss: The loss of fat and muscle results in less cushioning between bones and a hard surface (such as a bed or wheelchair). This can lead to Pressure Ulcers
- Poor nutrition
- Prolonged dehydration
- Mechanical ventilation or other reasons for medically-induced coma
- Overuse of narcotics leading to coma
- Bowel incontinence
- Frequent muscle spasms (frequent friction and shearing can cause Pressure Ulcers)
It is important to note that having a risk factor does not mean that one will get the condition. A risk factor increases ones chances of getting a condition compared to an individual without the risk factors. Some risk factors are more important than others.
Also, not having a risk factor does not mean that an individual will not get the condition. It is always important to discuss the effect of risk factors with your healthcare provider.
What are the Causes of Pressure Sores? (Etiology)
The causes of Pressure Sores are irritation (friction) and continuous pressure on a certain part of the body, usually from the weight of the body pressing down on the skin.
- Constant rubbing or compression of the skin due to a hard surface can harm the underlying tissues and damage blood vessels. This damage leads to the Bed Sores
- Bed Sores occur from too much time being spent on a bed (or chair) that places continuous pressure on the skin
- Another cause can be excess moisturizing, which causes the skin to become damp, soft, and fragile
What are the Signs and Symptoms of Pressure Sores?
Pressure Sores are categorized by their severity into one of the four stages.
Stage I signs and symptoms:
- The site of the ulcer may be painful, soft, warm, solid, or cool compared to the surrounding skin
- The color of the impacted area may be bright red in lighter-skinned individuals and discolored on darker-skinned individuals
- The affected area of pressurized skin is not yet broken
Stage II signs and symptoms:
- The skin begins to break damaging the epidermis and the underlying tissue is damaged or lost
- The color of the impacted area may be turning pink or red
- The pressured region may be shallow and resemble a ruptured blister
Stage III signs and symptoms:
- The ulcer is developing into a deep wound and transforms into a shape similar to a crater or a volcano
- The color changes to yellowish where the tissue is dead
- Foul odor emanates from the ulcer
- The skin is ulcerated exposing the underlying fat and subcutaneous tissues
Stage IV signs and symptoms:
- The ulcer results in excessive to extreme tissue loss
- The region has lost so much skin that muscles, bones, or tendons are exposed
- Dark, yellow, and crusty dead tissue cells are present in the ulcers
The stage may be unidentifiable when the ulcer is covered in yellow, brown, or black dead tissue. It is deemed unidentifiable or ‘un-stageable’, as it is impossible to see how deep the wound is in order to classify the sore.
How is Pressure Sores Diagnosed?
The process to evaluate and diagnose Pressure Sores includes:
- Complete physical examination and medical history including:
- Determining the depth and size of the ulcer
- Monitoring the region around the pressurized area for signs of spreading tissue damage or infection
- Checking for infection indications such as bleeding, fluids, or debris in the area of concern
- Detecting odors which point to an infection or the presence of dead tissue
- Blood tests
- Biopsies may be done to detect deep tissue infections and carcinomatous degeneration due to prolonged ulceration
A healthcare provider may diagnose the condition based on the following factors:
- The magnitude of pain
- History of Pressure Sores
- The appearance of the first Pressure Sore
- Hydration status of the individual
- Causes of pressure on the skin
Many clinical conditions may have similar signs and symptoms. Your healthcare provider may perform additional tests to rule out other clinical conditions to arrive at a definitive diagnosis.
What are the possible Complication of Pressure Sores?
Pressure Sores, especially severe ulcers, can cause a variety of complications including:
- Cellulitis: Although uncommon, cellulitis is a potentially serious bacterial skin infection. It may first appear as a red, swollen area which can eventually cause drastic pain, swelling, and even life-threatening complications
- Bone and joint Infections: Bone and joint infections, such as osteomyelitis, are possible complications of Pressure Sores, as it invades the joints and bones. Bone infections can reduce the functionality of joints and limbs, while joint infections can severely damage the tissues
- Sepsis: Sepsis is a life-threatening complication of an infection that occurs when biochemicals, which are released in the bloodstream trigger inflammation, or when bacteria enter the bloodstream and spread throughout the body. This can potentially damage multiple organ systems
- Cancer: Pressure Ulcers, or more specifically the ‘Marjolin ulcers’, can cause the development of squamous cell carcinoma, which is a type of aggressive cancer
How is Pressure Sores Treated?
Early stage sores are easily treatable and can be relieved with time and proper conservative care. It is more difficult to treat stage III and IV Pressure Sores. Treatments of such sores usually require a team of healthcare professionals.
Steps in treatment of Pressure Sores may include:
- Repositioning the individual to avoid placing pressure on the same area
- Using support surface to relieve pressure
- Cleaning and dressing the impacted area
- Removing damaged (infected or dead) tissues
- Managing pain: Non-steroidal anti-inflammatory drugs may be used to manage pain. Such painkillers can help the individual feel comfortable during cleaning and dressing of the ulcers
- Antibiotic therapy in case of bacterial infections
- A healthy diet and active exercise
- Negative pressure therapy: This is also known as vacuum-assisted closure and involves the application of suction to a clean wound. This method helps in faster wound healing
- Hyperbaric oxygen therapy: In this procedure, the region of the ulcer is placed in a hyperbaric chamber containing oxygen at increased pressure. This can help promote wound healing and decrease the incidence of bacterial infections
- Surgery. This is the last step a healthcare provider might consider, when all other treatments fail and the Pressure Ulcer fails to heal. Surgery would help improve the hygiene of the sore, prevent or treat any underlying infection, lower the risk for cancer, and reduce further fluid loss
- The surgeries required for deep Pressure Sores are often complex, with a reconstructive surgeon moving intact muscle, subcutaneous fat, and skin over the site, while maintaining the vascular supply
How is Pressure Sores Prevented?
It is much easier to prevent Pressure Sores than to medically treat them. The key prevention technique is ‘position change’. For individuals who are confined to their bed or chair, it is important that a caretaker change their position regularly. Constantly altering position limits the amount of constant pressure or friction in an area of skin over a long time. In this way, stress can be avoided on the skin and the skin kept ‘ulcer free’.
Other prevention techniques for Pressure Sores may include:
- Proper caretaking of skin, such as cleaning the affected areas with soap, protecting the skin by applying lotion to dry areas, examining the skin for new signs of sores, and ensuring that the skin does not get exposed to excessive moisture and bacteria
- Maintaining a healthy diet (even if one is immobile)
- Remaining hydrated, which is important for skin vitality
- Stopping smoking (smoking can contribute to the severity of the Pressure Sores)
- Another effective prevention technique is daily or regular exercise. The biggest contributing factor to Pressure Sores is severely limited mobility. However, a regimen of daily exercise can help maintain the skin and improve blood flow
What is the Prognosis of Pressure Sores? (Outcomes/Resolutions)
- Mild cases of Pressure Sores/Bed Sores, treated during the earlier stages, have better outcomes than severe cases treated during their later stages
- As long as the ulcers are not severe, Pressure Sores heal over time with proper positional adjustments/changes, good nutrition, and adequate wound management
- However, due to poor nutrition and immobility of most patients, Pressure Sores/Ulcers are often slow to heal, due to continuing unfavorable conditions. The treatment of other underlying conditions may also delay the healing process
- Bed Sores can lead to many infections including bone and joint infections. These ulcers may spread to other tissues and result in a systemic infection (such as sepsis)
- Pressure Sores are considered as indicators for several other diseases. If individuals with such sores have other potentially life-threatening health conditions, treating the underlying condition appropriately improves the prognosis for Pressure Sores
Additional and Relevant Useful Information for Pressure Sores:
- Studies indicate that for every 100 patients admitted into hospitals, 1-5 patients may get Pressure Sores
- In some cases, pain relief is required and patients may need to be referred to a pain clinic
Related Articles
Test Your Knowledge
Asked by users
Related Centers
Related Specialties
Related Physicians
Related Procedures
Related Resources
Join DoveHubs
and connect with fellow professionals


0 Comments
Please log in to post a comment.