What are the other Names for this Condition? (Also known as/Synonyms)
- Jumper's Knee
- Patellar Tendinopathy
What is Patellar Tendinitis? (Definition/Background Information)
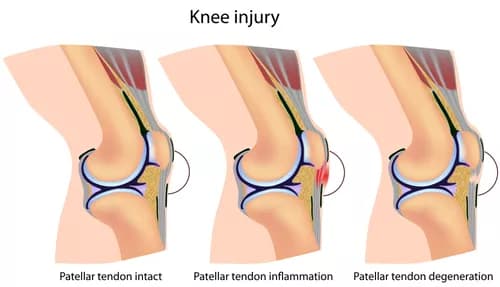
- Patellar Tendinitis is characterized by inflammation of the patellar tendon (the tendon connecting the patella (kneecap) to the shinbone
- It is usually caused by any physical activity, such as an athletic sport, which results in repetitive stress on the knee. Overall, there is a high rate of incidence of this condition among young athletes
- Rest, physical therapy, and over-the-counter medications, are usually the initial recommended measures to treat Patellar Tendinitis. However, surgery is an option, mostly if the pain does not improve after several months of nonsurgical treatment measures
- The prognosis of Patellar Tendinitis is usually excellent with appropriate treatment
Depending on the severity of the injury, physicians usually classify Patellar Tendinitis into three different grades. These grades include:
- Grade I Patellar Tendinitis: The pain occurs after exercising
- Grade II Patellar Tendinitis: The pain occurs before and after exercising; though, it subsides after the individual is warmed up
- Grade III Patellar Tendinitis: The pain occurs while exercising, which limits the individual’s performance
- Grade IV Patellar Tendinitis: There is a continuous pain that occurs during everyday activities
Who gets Patellar Tendinitis? (Age and Sex Distribution)
- Patellar Tendinitis may occur in individuals of all ages, races, ethnic groups, and genders
- The condition is most commonly observed among adolescents and young adults
- Patellar Tendinitis occurs in approximately 20% of the individuals who take part in sports that involve a lot of jumping such as basketball and volleyball
What are the Risk Factors for Patellar Tendinitis? (Predisposing Factors)
Common risk factors for Patellar Tendinitis include:
- Adolescents and young adults who are physically active, participate in sports activities
- Any sport that involves a lot of jumping such as basketball and gymnastics
- The presence of physical abnormalities or defects such as flatfeet
- Poor physical conditioning, such as tight thigh and hamstring muscles, can increase stress on the patellar tendon
- Muscle imbalance, muscular fatigue and weakness
It is important to note that having a risk factor does not mean that one will get the condition. A risk factor increases ones chances of getting a condition compared to an individual without the risk factors. Some risk factors are more important than others.
Also, not having a risk factor does not mean that an individual will not get the condition. It is always important to discuss the effect of risk factors with your healthcare provider.
What are the Causes of Patellar Tendinitis? (Etiology)
A few causal factors of Patellar Tendinitis include:
- Individuals participating in certain sports activities that put a lot of stress on the kneecap tendon such as basketball, badminton, volleyball, gymnastics, and certain track and field events
- Individuals with tight calf and hamstring muscles
- Suffering a traumatic injury to the knee or patellar tendon
What are the Signs and Symptoms of Patellar Tendinitis?
The signs and symptoms of Patellar Tendinitis include:
- Pain and swelling around the kneecap tendon, while walking or running
- Worsening pain when participating in sports
- Difficulty performing simple daily tasks
How is Patellar Tendinitis Diagnosed?
Tests and exams a physician may use to help diagnose Patellar Tendinitis include:
- Physical examination: During a physical examination, the physician will apply pressure to certain areas of the affected knee that is in pain. Individuals are also expected to provide an explanation of the circumstances that caused the injury. In addition to this, a complete medical history may aid in arriving at a definitive diagnosis
- X-ray of the knee: X-rays use radiation to produce images of the joints. Even though x-rays cannot visualize soft tissues (such as tendons), it can help the physician rule out other possible conditions that cause similar symptoms
- Magnetic resonance imaging (MRI) of the knee: An MRI is a more detailed scan that uses radio waves and strong magnetic fields to produce clearer images of the patellar tendon. This allows the physician to view any damage to the affected area
- General ultrasound imaging of the knee: Ultrasounds are high-frequency sound waves that generate a more detailed image of the soft tissues such as tendons
Many clinical conditions may have similar signs and symptoms. Your healthcare provider may perform additional tests to rule out other clinical conditions to arrive at a definitive diagnosis.
What are the possible Complications of Patellar Tendinitis?
A few complications of Patellar Tendinitis include:
- Decreased range of motion and function in the leg, if the condition is left untreated
- Prolonged and chronic pain
- Recurrence of symptoms if exercise or sports activities are resumed too quickly
How is Patellar Tendinitis Treated?
Initially, Patellar Tendinitis is usually treated with nonsurgical interventions. However, surgery is an option if the pain does not improve.
Nonsurgical treatments for Patellar Tendinitis may include:
- Any activity that further aggravates the condition should be avoided. The physician usually recommends refraining from all such activities until the symptoms get better and the tendons are healed
- Applying ice to the knee can help reduce pain and swelling
- Non-steroidal anti-inflammatory oral medications, such as ibuprofen or naproxen, may be used to treat Patellar Tendinitis. These medications can help decrease the pain and swelling
- Ultrasound-guided corticosteroid injections into the sheath around the patellar tendon (region near the spine, inside the vertebral column) help provide temporary relief of symptoms and in improving the range of motion. It is important to note that corticosteroid injections only give temporary relief. Prolonged episodes of such injections may injure the joints in the long-run
- Platelet-rich plasma (PRP): Platelet-rich plasma is a nonsurgical procedure that utilizes an individual's platelets to rebuild a damaged tendon or cartilage. The procedure is designed to treat athletes and active individuals who suffer from chronic tendon pain or osteoarthritis
- Therapists usually prescribe certain stretching and strengthening exercises that could aid in strengthening and improving the flexibility of the patellar tendon and also help reduce any discomfort
- Extracorporeal shock wave therapy (ESWT) is an increasingly popular (US FDA-approved) therapeutic approach in which high-energy sound waves are sent to the affected region. However, this therapy is still considered experimental by many physicians; even though research has shown that it may be effective
- In rare cases, surgery is an option if nonsurgical treatment methods are unsuccessful
How can Patellar Tendinitis be Prevented?
A few recommendations to help prevent Patellar Tendinitis include:
- Warming-up prior to exercising
- Stretch before exercising or taking part in sports activities, which increases flexibility in the tendons
- Maintain physical fitness, which helps keep strength, flexibility, and endurance in the patellar tendon
- Allow for an adequate recovery time between exercises
- To help prevent the recurrence of Patellar Tendinitis, individuals should wear appropriate safety equipment such as tape, protective strap or brace, or an adhesive bandage. However, this may be required for several weeks, even after the injury has healed
What is the Prognosis of Patellar Tendinitis? (Outcomes/Resolutions)
- A high percentage of Patellar Tendinitis heals without any serious complications. When properly treated under the guidance of a healthcare specialist, a high percentage of individuals regain their full strength and range of motion in the injured leg
- A full recovery and return to sports or normal daily activities may usually require about six weeks. This also depends on whether the patellar tendon is partially torn or completely torn
- However, complications, such as decreased range of motion in the knee, may develop in some individuals if the patellar tendon is left untreated
Additional and Relevant Useful Information for Patellar Tendinitis:
The following DoveMed website link is a useful resource for additional information:
Related Articles
Test Your Knowledge
Asked by users
Related Centers
Related Specialties
Related Physicians
Related Procedures
Related Resources
Join DoveHubs
and connect with fellow professionals

0 Comments
Please log in to post a comment.