What are the other Names for this Condition? (Also known as/Synonyms)
- Atherosclerotic Parkinsonism
- Parkinson Disease
- PD (Parkinson’s Disease)
What is Parkinson’s Disease? (Definition/Background Information)
- Parkinson’s Disease (PD) is a progressive neurodegenerative disorder that results from depletion of the neurotransmitter dopamine in the brain. It mostly affects elderly adults over the age of 55
- Individuals with Parkinson’s Disease mainly experience motor symptoms including impaired movement, balance, and posture. Cognitive, psychiatric, sensory, and autonomic symptoms may also be present
- Some forms of Parkinson’s Disease are familial (due to inherited genetic factors), while most are idiopathic (where the factors are not known). The disorder may also develop due to secondary causes such as injury to the brain or an infection
- A diagnosis of Parkinson’s Disease may be made by recognizing the classical signs and symptoms and through a neurological evaluation
- Currently, there is no cure for the condition, but the symptoms of Parkinson’s Disease may be treated using medications and physiotherapy. This can also slow the progression of the condition
- The prognosis of Parkinson’s Disease depends on many factors. Some forms of PD are better controlled than others. For a majority of people, the disorder is known to progress; but in others, and for some unknown reason, the symptom progression may be rapid
Who gets Parkinson’s Disease? (Age and Sex Distribution)
- Parkinson’s Disease is common and typically occurs in middle-age and older adults. The average age of symptom onset is 55-65 years, although 5% of the cases are observed to occur in adults younger than 40 years
- As many as 15% of the individuals between ages 65 and 74, and 50% of the individuals over age 85 have symptoms of Parkinson’s Disease
- When the condition develops in adults less than 50, it is termed early-onset Parkinson’s Disease, and the cause is largely associated with a positive family history
- Men have a slightly higher incidence of the condition than women
- Parkinson’s Disease is seen worldwide affecting individuals of all racial and ethnic groups
What are the Risk Factors for Parkinson’s Disease? (Predisposing Factors)
The risk factors of Parkinson’s Disease include the following:
- The main risk factor for Parkinson’s Disease is advancing age. Most cases are noted in individuals older than 60.
- There is also some genetic susceptibility, as first degree relatives of patients diagnosed with Parkinson’s are twice as likely to develop the condition
- Environmental risk factors include exposure to certain toxins and medications, living in rural areas, drinking well water, working with pesticides, and working in wood/paper mills. These risk factors are not yet well categorized and are still being researched into
- Repeated head trauma and prior brain infection are also risk factors
It is important to note that having a risk factor does not mean that one will get the condition. A risk factor increases one's chances of getting a condition compared to an individual without the risk factors. Some risk factors are more important than others.
Also, not having a risk factor does not mean that an individual will not get the condition. It is always important to discuss the effect of risk factors with your healthcare provider.
What are the Causes of Parkinson’s Disease? (Etiology)
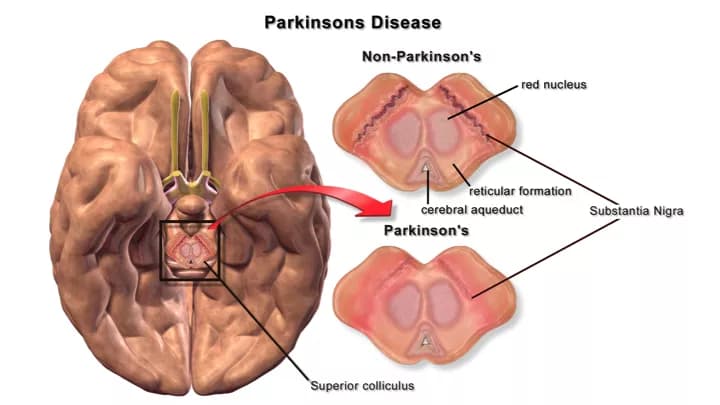
- The cause of the symptoms of Parkinson’s Disease (PD) is a result of the death of neurons (brain cells) in localized brain structures, called the substantia nigra and locus coeruleus. These neurons normally produce dopamine, a neurotransmitter that acts as a chemical signal to brain regions responsible for motor activity
- As a consequence of impaired neurons (or their death), fewer dopaminergic neurons result in decreased excitation of the brain regions that initiate and coordinate movement. Additionally, there is a loss of norepinephrine (both a neurotransmitter and a hormone) that causes non-movement associated signs and symptoms of the disease
- The underlying cause of dopaminergic neuron loss is unknown in most cases. Parkinson’s Disease due to unknown causes is termed as Idiopathic Parkinsonism or Primary Parkinsonism. It is the most common form
- 5% of the cases are inherited (familial forms of Parkinson’s Disease due to genetic mutations) that tend to have an earlier onset of symptoms (typically before age 45-50) and a longer course of illness. PD due to genetic factors is known as Hereditary Parkinsonism
- Secondary Parkinson’s Disease can however result from vascular diseases, AIDS, and other infections
- In some patients, toxins (such as copper, iron, lead, manganese, cyanide, methanol, and carbon monoxide) and certain medications (such as antipsychotics, antiseizure, and anti-nausea) may be the cause of Parkinson-like symptoms
What are the Signs and Symptoms of Parkinson’s Disease?
Patients may experience weakness, fatigue, aches, and shoulder pain early in the course of the disease. Usually, one side of the body is initially affected. The classic signs and symptoms of Parkinson’s Disease include:
- Tremors that involve the limbs, jaw, or head
- Muscular rigidity
- Poor balance and coordination
- Slow movement (bradykinesia)
- Shuffling gait
- Stooped posture
Tremors are usually worse at rest and begin in the hands or feet on one side of the body. A continuous ‘pill-rolling’ motion of the hand and wrist is very common. Later in the disease course, tremors of the lips, tongue, and chin may develop.
- Many patients have a flexed posture when standing due to increased muscular rigidity
- Initiation of voluntary movements and fine motor movements, such as handwriting, are often impaired
- Walking without swinging the arms and shuffling the feet are common features
- Facial expressions may be decreased, and voice changes may occur (speaking difficulties)
- Chewing and swallowing difficulties affecting food intake
- Patients may also develop anxiety, depression, sleep problems, blurry vision, decreased sense of smell (anosmia), and urinary problems
- Memory loss and cognitive function impairment
The rate of progression and severity of Parkinson’s Disease can vary from one individual to another.
How is Parkinson’s Disease Diagnosed?
The diagnosis of Parkinson’s Disease may involve the following:
- Physical examination and medical history evaluation: The condition is diagnosed by the presence of clinical symptoms in adults experiencing tremor, slow or stiff movements, and balance or gait problems. Improvement of symptoms after starting medications may help confirm the diagnosis
- Thorough neurological examination by a qualified healthcare professional
- There are no specific laboratory tests or imaging studies to aid a diagnosis. Diagnosis early in the disease course, when symptoms are mild, can be difficult
- The individual’s family members may be the first to notice the appearance of symptoms, which may be subtle
Many clinical conditions may have similar signs and symptoms. Your healthcare provider may perform additional tests to rule out other clinical conditions to arrive at a definitive diagnosis.
What are the possible Complications of Parkinson’s Disease?
The complications of Parkinson’s Disease may include:
- Depression and anxiety occur in 50% of the individuals; it can be treated though
- Dementia is common with advanced Parkinson’s Disease
- Symptoms of autonomic dysfunction, such as urinary incontinence and constipation, excessive sweating, orthostatic hypotension (feeling lightheaded upon standing), and sexual dysfunction may develop
- Postural instability and balance problems may lead to falls and related injuries/fractures. Injuries from falls are a major cause of hospitalization and death
How is Parkinson’s Disease Treated?
There is no cure for Parkinson’s Disease. Currently, there are no medications available that can slow the disease progression or completely restore normal movement. The symptoms are treated so that the affected individuals can continue to work and maintain a good quality of life.
There are many different types of medications for Parkinson’s Disease.
- Overall, tremors, rigidity, and bradykinesia respond better to treatment than cognitive and autonomic symptoms
- Drugs that are precursors to dopamine or that mimic dopamine often provide good symptom relief
- Other types of medications can help by increasing the production and release of dopamine, or by preventing its breakdown
- Most medications have side effects, and so adjustments are often required to find optimal doses
- Following prolonged treatment, patient responses to medications may decrease over time
Most specialists believe that medications should be started when symptoms begin to interfere with normal functioning. Regular physical exercise is also very important to maintain strength, range of motion and balance, and to prevent further disability related to a sedentary lifestyle.
Other therapies that may help individuals with Parkinson’s Disease include:
- Physical and occupational therapy
- Speech therapy
- Healthy lifestyle with balanced diet and exercise
- Therapies based on complementary medicine such as yoga, tai chi, or massage therapy
- Enlisting the support of family members and friends
Occasionally, surgery is done to relieve symptoms that do not respond to medication. Tremors that are resistant to medication have been treated with high-frequency stimulation of particular brain areas with implanted electrodes (deep brain stimulation). Current research is focused on gene therapy and stem cell transplantation to replace the dying dopaminergic neurons, as well as neuro-protective strategies to prevent neuron loss.
How can Parkinson’s Disease be Prevented?
Currently, there are no specific methods or guidelines to prevent most cases of Parkinson’s Disease. However, recognition of the following factors are helpful:
- Avoidance of repeated head trauma, certain toxins, and occupations and medications known to be associated with Parkinson’s Disease
- Early diagnosis with close monitoring and treatment of Parkinson’s Disease is important. Prompt treatment and early recognition of the condition will help in having improved outcomes
- Genetic testing of the expecting parents (and related family members) and prenatal diagnosis (molecular testing of the fetus during pregnancy) may help to better the understanding of the risks during pregnancy
- If there is a family history of the condition, then genetic counseling will help assess risks before planning for a child
Taking the prescribed medications for Parkinson’s Disease regularly is important. Voluntarily discontinuing the medications can result in serious side effects.
What is the Prognosis of Parkinson’s Disease? (Outcomes/Resolutions)
- Parkinson’s Disease is a degenerative disorder affecting the brain and nervous system that cannot be cured, but only managed through proper treatment (medication, exercises, and surgery in some cases). This can help decrease the rate of progression of the condition
- The symptoms of Parkinson’s Disease may progress and worsen over many months to years. A slow increase in impairment may occur over 10 to 25 years
- In some patients, the disease may progress slowly; while in others, the symptom progression is rapid. Research is underway to understand the reason for this occurrence
Additional and Relevant Useful Information for Parkinson’s Disease:
- After Alzheimer’s disease, Parkinson’s Disease is recognized as the second most common neurodegenerative condition affecting millions of individuals around the world
- Consumption of coffee/caffeine, smoking, use of NSAIDs (non-steroidal anti-inflammatory drugs), and postmenopausal estrogen replacement therapy are all factors that are associated with decreased risk of the condition
Related Articles
Test Your Knowledge
Asked by users
Related Centers
Related Specialties
Related Physicians
Related Procedures
Related Resources
Join DoveHubs
and connect with fellow professionals

0 Comments
Please log in to post a comment.