What are the other Names for this Condition? (Also known as/Synonyms)
- Primary Osteoporosis
- Type I Osteoporosis
- Postmenopausal Osteoporosis
What is Primary Osteoporosis? (Definition/Background Information)
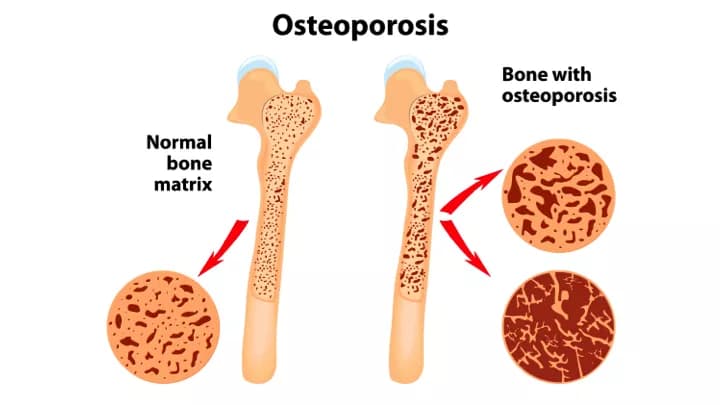
- Primary Osteoporosis is a type of Osteoporosis that typically occurs in postmenopausal women. It is associated with the decline in estrogen levels that happens when a woman experiences menopause
- When estrogen levels decline, the skeleton becomes more sensitive to parathyroid hormone (PTH). PTH causes increased calcium resorption from the bone and results in bone thinning and bone weakening.
- Osteoporosis has very mild visible signs. Typically, people do not realize that they have Osteoporosis until they injure themselves and break or fracture a bone. Most injuries occur after minor trauma or missteps, including bending over, lifting things, jumping, or falling.
- While it is not possible to completely cure Osteoporosis, medications can be taken to ease any pains that exist due to injury, block and slow down calcium resorption, and rebuild bones.
Who gets Primary (Type I) Osteoporosis? (Age and Sex Distribution)
- Women over the age of 50 are most susceptible to getting Primary Osteoporosis. This is due to the fact that they may have already experienced menopause.
- The highest incidence rate of Primary Osteoporosis is in women in their 60s and 70s.
- While Primary Osteoporosis can occur in males, the incidence in women is estimated to be eight times higher. Furthermore, bone loss percentage is lower in males than in females.
What are the Risk Factors for Primary Osteoporosis? (Predisposing Factors)
Common risk factors of Primary Osteoporosis include:
- Gender - women are more likely to suffer from Osteoporosis due to their lower peak bone mass and a higher rate of bone loss
- Ethnicity - Caucasian and Asian individuals are at a greater risk compared to African Americans and Hispanics, who have greater peak bone masses
- Age - increased age means that your bones are weaker
- Hormone imbalances - low estrogen can increase your risk of Osteoporosis
- Body size - smaller individuals have a higher risk of developing Osteoporosis because of their smaller peak bone mass
- A family history of Osteoporosis
- Malnutrition
It is important to note that having a risk factor does not mean that one will get the condition. A risk factor increases ones chances of getting a condition compared to an individual without the risk factors. Some risk factors are more important than others.
Also, not having a risk factor does not mean that an individual will not get the condition. It is always important to discuss the effect of risk factors with your healthcare provider.
What are the Causes of Primary Osteoporosis? (Etiology)
- Primary Osteoporosis is caused by the age-related, postmenopausal symptom of declining estrogen levels. Research has shown that estrogen slows down calcium resorption time from bones, which prevents rapid breakdown of bones. When estrogen levels decline, calcium resorption time increases and bones weaken more quickly.
- In men, Primary Osteoporosis is thought to be caused by declining testosterone levels, which also quickens the calcium resorption time from bones.
- Research has also found that low levels of vitamin D can cause Primary Osteoporosis. Vitamin D is an essential vitamin in calcium absorption and normal bone growth. When vitamin D levels are low, calcium is not absorbed as efficiently and bones are not as strong. Furthermore, vitamin D has been shown to increase parathyroid hormone (PTH) levels.
- PTH is important in regulating calcium levels in the blood. When low levels of calcium are found in the body, the glands are stimulated to produce more PTH. PTH then stimulates bone resorption to increase blood calcium levels, which leads to bone breakdown and weakening.
What are the Signs and Symptoms of Primary Osteoporosis?
Common signs and symptoms of Primary Osteoporosis include:
- Joint problems
- Injury after minor trauma
- Fractures
- Broken bones
- Low estrogen levels
- High PTH levels
- Kyphosis (stooped posture; results from compression fractures on the spine)
In most cases, Primary Osteoporosis does not become apparent until injury has already occurred. It is often called the “silent disease” because people do not know they have Osteoporosis until they break or fracture a bone.
How is Primary Osteoporosis Diagnosed?
- Primary Osteoporosis is often difficult to diagnose because it does not become apparent until the individual has already injured themselves.
- Bone density testing is recommended for individuals who are likely to develop Osteoporosis. These individuals include people over the age of 60 and people who showcase any of the risk factors of Osteoporosis. A number of tests exist to measure bone density, including:
- Bone densitometry: detects bone density by detecting how much bones absorb photons made by x-rays
- Ultrasound: ultrasounds can be done to determine bone density by imaging bones
- X-rays
- Primary Osteoporosis can also be confirmed by conducting blood tests that measure vitamin D levels, calcium levels, and PTH levels in the blood.
Many clinical conditions may have similar signs and symptoms. Your healthcare provider may perform additional tests to rule out other clinical conditions to arrive at a definitive diagnosis.
What are the possible Complications of Primary Osteoporosis?
- The biggest complication that can arise from Primary Osteoporosis is the risk of fracturing or breaking bones due to the low bone density that results from the disease. Hip and wrist fractures are the most common Osteoporosis-related injuries.
- A stooped, hunched posture can also occur due to Primary Osteoporosis. This results from vertebral fractures in the spine.
How is Primary Osteoporosis Treated?
- A variety of medications and lifestyle changes can be used to treat Primary Osteoporosis.
- Antiresorptive drugs, including bisphosphonates, calcitonin, and selective estrogen-receptor modulators work to slow down bone breakdown by blocking calcium resorption. While this may help in the short run, by blocking this process bone formation may also be reduced as it lowers calcium levels in the bloodstream as well.
- Anabolic drugs can also be used to treat Primary Osteoporosis. These drugs are bone-forming drugs that can help restore bone and prevent fractures and breakages. The most common anabolic drug is low-dose parathyroid hormone, which is taken by injection.
- Medical professionals also suggest changing your diet to include more vitamin D and calcium. Both will aid in bone formation and bone maintenance. In some cases, vitamin D or calcium supplements may be prescribed.
How can Primary Osteoporosis be Prevented?
- The most effective way to prevent Primary Osteoporosis is through regular exercise and a balanced diet.
- Exercise is important as it will make the bones grow stronger. Jogging, stairs, dancing, tennis, walking, and hiking have all been found to strengthen bones effectively.
- Dietary changes can also reduce your chances of developing Primary Osteoporosis. A diet high in calcium and vitamin D is recommended. It is also suggested that alcohol consumption is slow and smoking is stopped.
What is the Prognosis of Primary Osteoporosis? (Outcomes/Resolutions)
- While it is difficult to undo the damage caused by Primary Osteoporosis, with proper medical care, regular exercise, and a balanced diet, most individuals can mend their bones and resume relatively normal functioning.
Additional and Relevant Useful Information for Primary Osteoporosis:
The following DoveMed website link is a useful resource for additional information:
Related Articles
Test Your Knowledge
Asked by users
Related Centers
Related Specialties
Related Physicians
Related Procedures
Related Resources
Join DoveHubs
and connect with fellow professionals

0 Comments
Please log in to post a comment.