What are the other Names for this Condition? (Also known as/Synonyms)
- NASH (Non-Alcoholic Steatohepatitis)
What is Non-Alcoholic Steatohepatitis? (Definition/Background Information)
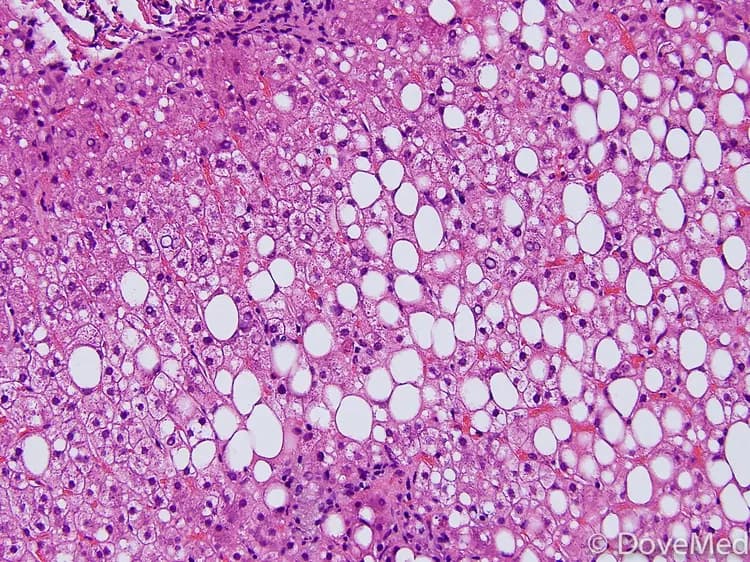
- Non-Alcoholic Steatohepatitis (NASH) is a condition that is characterized by fat accumulation (steatosis) followed by inflammation (hepatitis) due to unknown reasons, other than alcohol, drugs, and medications. This inflammation can derange liver function and damage the liver structure
- NASH is a condition on the spectrum of non-alcoholic fatty liver diseases (NAFLD). The spectrum includes:
- Steatosis (fatty liver)
- NASH (fatty liver with accompanying inflammation)
- Cirrhosis (irreversible liver scarring)
- And eventually, hepatocellular carcinoma (liver cancer)
- Non-Alcoholic Steatohepatitis can occur in individuals of all ages and can be seen worldwide. There is no racial or ethnic preference for NASH, though it is more severe in Asians and Hispanics. Children and adolescents may be affected by pediatric NASH
- Obesity, diabetes mellitus type 2, insulin resistance, and hypertriglyceridemia all increase one’s risk of developing the condition. However, the cause of Non-Alcoholic Steatohepatitis is unknown
- Typically, individuals with NASH do not have any symptoms, which make it difficult to diagnose the condition. It is usually identified during routine checkups and confirmed by blood tests, imaging tools, or liver biopsies
- NASH may be treated through a combination of weight loss programs and medications to treat diabetes mellitus and hypertriglyceridemia. Most individuals with the condition have a good prognosis, when lifestyle changes are made to control weight. Untreated or severe progressive conditions may lead to liver cirrhosis and liver failure
Who gets Non-Alcoholic Steatohepatitis? (Age and Sex Distribution)
- Non-alcoholic steatohepatitis can affect individuals of any age
- It affects both male and female genders at equal rates
- NASH can be seen worldwide. Even though there is no ethnic or racial preference for NASH, the condition is noted to be more severe in Asians and Hispanics than Caucasians and African Americans
What are the Risk Factors for Non-Alcoholic Steatohepatitis? (Predisposing Factors)
Risk factors of Non-Alcoholic Steatohepatitis include:
- Obesity, which causes individuals to carry extra fat deposits. One function of the liver is to break down fats. If excess fat is found in the body, the liver cannot efficiently break down fats, which may lead to fat accumulation in the liver. A sedentary lifestyle and over-nutrition (adding extra calories at mealtimes regularly) can lead to weight gain and obesity
- Individuals who are insulin resistant can develop diabetes mellitus type 2. This increases the risk of developing NASH
- Hypertriglyceridemia (high blood triglyceride levels) and hyperlipidemia increases the risk
- Exposure to certain medications and toxins can increase the risk of getting NASH
- Genetic factors: Some genetic factors, such as PNPLA3 polymorphisms, can increase the risk. However, there may be other, unknown genetic factors that may also increase one’s risk of NASH
It is important to note that having a risk factor does not mean that one will get the condition. A risk factor increases one's chances of getting a condition compared to an individual without the risk factors. Some risk factors are more important than others.
Also, not having a risk factor does not mean that an individual will not get the condition. It is always important to discuss the effect of risk factors with your healthcare provider.
What are the Causes of Non-Alcoholic Steatohepatitis? (Etiology)
The cause and mechanism of Non-Alcoholic Steatohepatitis is currently unknown. Researchers have observed that NASH may be multifactorial (many factors may be involved):
- Metabolic disorders, including obesity, diabetes mellitus type 2, hypertriglyceridemia, and endocrine disorders, such as hypothyroidism and hypopituitarism, can contribute to the development of NASH
- Rapid and extreme weight loss is a known cause of Non-Alcoholic Steatohepatitis. Jejunoileal bypass surgery is a common method of rapid weight loss procedure that can result in NASH
- Various drugs, including amiodarone, perhexiline maleate, estrogen, and methotrexate, have been noted to cause NASH
- Occupational hazards can also contribute to the development of NASH:
- Hepatotoxicity (chemical-driven liver damage) has been reported to cause NASH
- Toxins from vinyl chloride and copper have also been associated with the condition
- When NASH is associated with chronic viral hepatitis C, the disease progresses at a faster rate and results in cirrhosis
- Genetic abnormalities have also been seen to increase the likelihood of NASH
What are the Signs and Symptoms of Non-Alcoholic Steatohepatitis?
Most individuals with Non-Alcoholic Steatohepatitis are usually asymptomatic, until it becomes severe (advanced). If NASH remains undiagnosed and untreated, signs and symptoms may arise that may include:
- Mild symptoms: Fatigue, malaise (general discomfort or unease), and abdominal pain
- When the liver is functioning properly, it carries out essential functions related to digestion, metabolism, immunity, and nutrient storage. When the liver is not functioning properly:
- It cannot synthesize blood proteins to maintain oncotic pressure in blood. As a result, edema, or abnormal fluid accumulation in the belly, can occur
- Liver function abnormalities can also result in jaundice or yellowing of the skin. When the liver is unable to process red blood cells as they break down, bilirubin can build up in the body causing the skin to become yellow
- Abnormalities in liver functioning can also make it difficult to properly metabolize sex steroids
- Liver enlargement due to fat deposits and inflammation can result in abdominal pain
- Signs of portal hypertension, such as blood in the stool, enlargement of the spleen, development of ascites (fluid accumulation in the peritoneal cavity), and hepatic encephalopathy (confusion or forgetfulness as a result of liver dysfunction), may signify that cirrhosis, or irreversible scarring of the liver, has occurred
How is Non-Alcoholic Steatohepatitis Diagnosed?
Non-Alcoholic Steatohepatitis is diagnosed using the following tools:
- Thorough evaluation of the individual’s medical history and a complete physical examination. An evaluation of medical history will determine if there is a presence of predisposing factors such as obesity or diabetes mellitus, or occupational exposure. Physical examination and clinical workup may uncover findings such as liver enlargement or edema (swelling)
- Liver function tests, which are done by collecting blood samples, can determine if aspartate transaminase (AST) or alanine transaminase (ALT), both liver enzymes, are present at abnormal levels. When the liver becomes damaged, AST and ALT blood levels become elevated
- Ultrasounds, MRIs, and CT scans can be used to image the liver and determine if fat deposits and enlargement are present
- Scoring systems have been developed to predict the development of NASH and associated fibrosis. The combination of factors (or tests) used for scoring are:
- Age, race, body mass index (BMI), the presence or absence of diabetes mellitus type 2 or high blood sugar levels, presence or absence of hypertension, presence or absence of sleep apnea, liver transaminase level, triglyceride levels, albumin levels, blood platelet count, etc.
These scoring systems help the physicians decide whether to perform a liver biopsy or not
- A percutaneous liver biopsy is the most definitive diagnostic tool to establish NASH. In this procedure the physician removes a sample of the liver tissue and sends it to the laboratory for a histopathological examination. The pathologist examines the biopsy under a microscope. After putting together the clinical findings, special studies on tissues (if needed), and the microscope findings, he/she arrives at a definitive diagnosis. The biopsy may help identify fat deposits, inflammation, or fibrosis (scarring) of the liver
Many clinical conditions may have similar signs and symptoms. Your healthcare provider may perform additional tests to rule out other clinical conditions in order to arrive at a definitive diagnosis.
What are the possible Complications of Non-Alcoholic Steatohepatitis?
Complications associated with Non-Alcoholic Steatohepatitis depend upon the severity of the disorder:
- Liver failure may arise due to continued damage to the liver as a result of fat deposits and liver inflammation
- When liver cirrhosis occurs:
- Blood protein synthesis is compromised and clotting does not effectively occur and this can result in massive bleeding
- Individuals are often unable to filter blood effectively, which can lead to the accumulation of toxins in the body. These toxins can travel through the body and have negative effects on the brain, leading to encephalopathy
- The liver cannot properly process broken down and damaged red blood cells. As a result, bilirubin can accumulate in the body and cause jaundice
- Ascites, fluid accumulation in the peritoneal cavity, may develop
- Portal hypertension: Cirrhosis slows down the normal flow of blood through the liver. This increases blood pressure in the vein that brings blood from the intestines to the liver
- Hepatocellular carcinoma (a type of liver cancer) can occur if the condition is left untreated, or if it progresses
How is Non-Alcoholic Steatohepatitis Treated?
Treatment for Non-Alcoholic Steatohepatitis (NASH) depends on the severity of the condition. A typical treatment plan for an individual with NASH may include:
- Weight loss programs to control obesity through diet, exercise, and medication. A low glycemic index diet has been shown to be effective in lowering one’s BMI
- Control of diabetes, hypercholesterolemia, and hypertriglyceridemia using medications and lifestyle changes
- Commonly used medications in the treatment of NASH and its associated conditions include thiazolidinediones, vitamin E, pentoxifylline, ursodeoxycholic acid, and others
- Liver transplant may be required, if NASH progresses to cirrhosis of liver
Regardless of what treatment is received, follow-up care and regular screening are important to ensure that Non-Alcoholic Steatohepatitis does not progress and cause further complications.
How can Non-Alcoholic Steatohepatitis be Prevented?
- The risk of developing Non-Alcoholic Steatohepatitis can be reduced by losing weight (if you are obese or overweight) and exercise
- Use of medications to control blood sugar levels (diabetes), treating hypertension, hypercholesterolemia, and hypertriglyceridemia can help in the prevention of NASH
It is not always possible to follow these preventative measures. It is important to attend regular medical screenings so that NASH can be detected early and treated properly.
What is the Prognosis of Non-Alcoholic Steatohepatitis? (Outcomes/Resolutions)
- The prognosis of Non-Alcoholic Steatohepatitis depends on the severity of the liver injury
- In most cases, where the liver injury is not extensive, the prognosis is good with timely diagnosis and appropriate treatment
- If, however, severe liver injury and cirrhosis is present, there is a chance of development of liver cancer and other complications. Individuals with severe NASH may not always have a favorable prognosis
Additional and Relevant Useful Information for Non-Alcoholic Steatohepatitis:
- Non-alcoholic fatty liver disease (NAFLD) affects 20 - 45% of Americans, whereas NASH affects 3-5 % of Americans
- Liver needle biopsy is a minimally-invasive procedure. During this procedure, a biopsy of the liver tissue is performed to evaluate liver abnormalities
The following article link will help you understand liver needle biopsy:
http://www.dovemed.com/common-procedures/procedures-surgical/liver-needle-biopsy/
Related Articles
Test Your Knowledge
Asked by users
Related Centers
Related Specialties
Related Physicians
Related Procedures
Related Resources
Join DoveHubs
and connect with fellow professionals

0 Comments
Please log in to post a comment.