What are the other Names for this Condition? (Also known as/Synonyms)
- MC (Molluscum Contagiosum)
- Molluscum Contagiosum Infection
- Molluscum Verrucosum
What is Molluscum Contagiosum? (Definition/Background Information)
- Molluscum Contagiosum (MC) is a common viral infection of the skin, caused by the Molluscum Contagiosum virus
- It is characterized by small, painless, and pearl-like papules (bumps) on the skin that are typically white, pink, or flesh-colored
- The condition spreads by direct skin-to-skin contact, through touching objects contaminated with the virus, sexual contact, and touching other parts of the body after scratching molluscum bumps
- Generally, Molluscum Contagiosum is a mild condition causing no harm, and most often seen in young and very young children, including teenagers. However, adults may also be affected by the condition
- In many, the skin bumps resolve from the response of the immune system. Since it may take over a year for the symptoms to resolve and for Molluscum Contagiosum to completely disappear, treatment is generally recommended
- The treatment also helps minimize spread within a family or social groups. The treatment for Molluscum Contagiosum could include creams, medications, and surgical removal of the skin papules
Who gets Molluscum Contagiosum? (Age and Sex Distribution)
- Molluscum Contagiosum often affects children between the ages of 1 and 12 years, but it can occur at any age
- Both males and females may be affected
- Molluscum Contagiosum occurs worldwide and individuals of all races and ethnic groups are affected
What are the Risk Factors for Molluscum Contagiosum? (Predisposing Factors)
The risk factors for Molluscum Contagiosum are as follows:
- Having a weakened immune system, such as due to HIV/AIDS, or due to treatment for cancer
- Children having atopic dermatitis, the most common form of eczema, have an increased risk for developing Molluscum Contagiosum
- Living in a tropical location, as the Molluscum Contagiosum virus spreads well in warm and humid environments. Hence, the infection is more frequently seen in tropical countries
- In some, no clearly identifiable risk factors are noted
It is important to note that having a risk factor does not mean that one will get the condition. A risk factor increases ones chances of getting a condition compared to an individual without the risk factors. Some risk factors are more important than others.
Also, not having a risk factor does not mean that an individual will not get the condition. It is always important to discuss the effect of risk factors with your healthcare provider.
What are the Causes of Molluscum Contagiosum? (Etiology)
- The Molluscum Contagiosum Infection is caused by Molluscum Contagiosum virus, which is a part of the poxvirus family. The virus enters the body through any break in the skin
- It spreads through direct skin-to-skin contact, which occurs when the molluscum bumps on the infected person are touched
- The infection also spreads by touching objects contaminated with the virus, such as towels, toys, clothing, and bedding
- Sexual contact with an infected individual can also spread the Molluscum Contagiosum virus
- Spread of the skin bumps in an individual may occur by scratching or rubbing the bumps, and then touching another area of the body. This causes the virus to spread to other parts of the body
- However, most individuals are relatively resistant to an infection from Molluscum Contagiosum. This indicates that they are not likely to develop molluscum if they come into contact with the virus
What are the Signs and Symptoms of Molluscum Contagiosum?
The signs and symptoms of Molluscum Contagiosum are as follows:
- Round and raised papules (spots) on the skin that are often:
- Small; about 1-3 millimeters in diameter
- Spots that grow over time to become about the size of a pencil eraser
- White, pink, or flesh-colored with a “pearly” appearance
- Filled with a waxy or cheesy substance in the central core, which contains the contagious virus
- Characterized by a small indentation, or dimple, at the top
- Painless, but can become red, itchy, inflamed, or infected, particularly if the bumps are scratched
- Molluscum can appear as a single lesion, or as clusters, groups, or even in rows. Approximately between 1 and 20 lesions are observed. At times, hundreds of lesions are seen
- Spreading of the virus to other areas of the skin can occur from scratching the bumps and then touching another part of the body
- In children, the molluscum lesions are usually located on the face, neck, hands, arms, armpits, chest, stomach, legs, or genital area
- In adults, the bumps are typically found on the inner thighs, abdomen, or genitalia
How is Molluscum Contagiosum Diagnosed?
Molluscum Contagiosum is diagnosed as follows:
- A complete physical examination and a thorough medical history: A physician is usually able to identify Molluscum Contagiosum by examining the bumps on the skin
- The doctor may refer the affected individual to a dermatologist or a doctor, who specializes in diseases of the skin
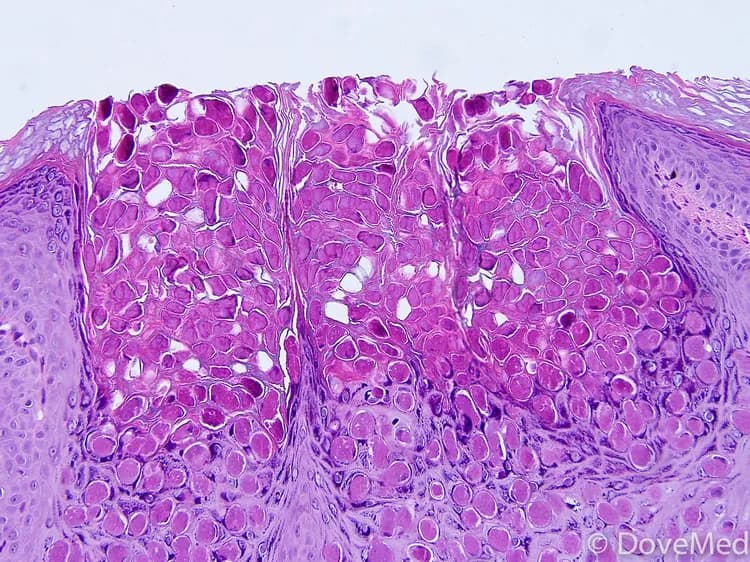
- In some cases, the doctor may scrape skin from the infected area to obtain a sample. The skin scrapping is then examined under a microscope by a pathologist, to arrive at a definitive diagnosis
- A skin biopsy may also be performed occasionally
Many clinical conditions may have similar signs and symptoms. Your healthcare provider may perform additional tests to rule out other clinical conditions to arrive at a definitive diagnosis.
What are the possible Complications of Molluscum Contagiosum?
Possible complications of Molluscum Contagiosum are as follows:
- Molluscum Contagiosum could become a highly contagious chronic infection, in which the skin bumps can persist for months or even years. In these cases, the infection easily spreads to different parts of the body
- Sometimes, secondary bacterial infections may arise
- Inflammation at and around the molluscum, which is an indication of the immune system’s response to the infection, can cause redness, itching, and discomfort
- Scarring may occur after Molluscum Contagiosum has healed; scarring is more likely to occur on areas of the skin where there is more fatty tissue, such as the thighs. Such scarring can result in social and emotional issues
- Conjunctivitis, or pink eye, may occur in individuals with Molluscum Contagiosum, if the bumps are close to the eyes or on the lash margins
- Individuals with compromised immune systems (patients with HIV/AIDS, or patients receiving cancer treatment) typically have more numbers of and larger molluscum bumps; these are usually harder to treat
How is Molluscum Contagiosum Treated?
Treatment is often advised to avoid spreading of the contagious molluscum papules. The following factors are considered during treatment of Molluscum Contagiosum:
- Children may not need treatment, as the bumps often go away on their own. Treating Molluscum Contagiosum may be painful for young children, and it can also rarely leave scars
- Individuals with weak immune systems require treatment. The molluscum in such individuals will not subside or disappear spontaneously without proper treatment
- At a given treatment session, only the visible lesions can be treated. Over time, new lesions will arise. Prompt treatment is advisable, because the new lesions will shed virus and inoculate more skin sites. Prolonged molluscum infection can become a troublesome experience
Surgery for Molluscum Contagiosum may include:
- Removing molluscum lesions by using a dull curette to painlessly flick the molluscum bodies from the skin
- Removing molluscum lesions by freezing them with liquid nitrogen
- Pulsed dye laser to destroy molluscum lesions has been reported to be successful
Medications:
- The dermatologist may recommend office applications of medications, such as cantharidin, extracted from blister beetles. This is applied directly on the lesions, to be washed off at home. A pinpoint painless blister forms, lifting off the molluscum lesions treated. As new lesions form, repeat visits are needed
- At home treatments include tretinoin, used for acne and skin rejuvenation. This dries and irritates the local skin, initiating an immune response. Imiquimod is a chemical immune signal cream, initially approved for genital warts. Applied to Molluscum Contagiosum lesions, it signals immune cells to attack the virus-infected skin cells
Molluscum Contagiosum can be left to subside and go away on its own; individual lesions may disappear within 2-3 months. Nevertheless, it is normal for new ones to grow, as older ones fade. Thus, it may take anywhere between 6-18 months for the lesions to completely disappear. Thus, a treatment of Molluscum Contagiosum is usually advised.
How can Molluscum Contagiosum be Prevented?
The following measures may be taken to help prevent the spread of Molluscum Contagiosum:
- Avoid touching, scratching, or rubbing the bumps
- Wash hands regularly and often
- Try to cover the molluscum bumps with clothing or bandages, to prevent others from touching the bumps and becoming infected. Also be sure to change bandages daily, and keep these skin areas clean
- Do not share personal items, such as towels, clothing, or hairbrushes, with others
- Avoid sexual contact, especially if you have Molluscum Contagiosum on or in close proximity to the genital area, until the bumps have completely healed
- Avoid participating in contact sports, including wrestling or football, unless all molluscum bumps can be covered by clothing or bandages
- Do not shave over skin that has molluscum bumps
- When swimming in public pools, it is recommended to cover bumps with watertight bandages and to avoid sharing kickboards, water toys, or towels
What is the Prognosis of Molluscum Contagiosum? (Outcomes/Resolutions)
The prognosis for Molluscum Contagiosum is as follows:
- Molluscum lesions usually go away on their own, without leaving any scars. The lesions are contagious until they disappear completely
- Individual lesions disappear within 2-3 months, but the complete disappearance of all lesions may take anywhere between 6-18 months
- Individuals with weak immune systems may have a more serious form of Molluscum Contagiosum, where the lesions are larger, more numerous, and more challenging to treat
Additional and Relevant Useful Information for Molluscum Contagiosum:
The following DoveMed website link is a useful resource for additional information:
https://www.dovemed.com/diseases-conditions/infection-center/
Related Articles
Test Your Knowledge
Asked by users
Related Centers
Related Specialties
Related Physicians
Related Procedures
Related Resources
Join DoveHubs
and connect with fellow professionals


0 Comments
Please log in to post a comment.