Merkel Cell Carcinoma of Skin
What are the other Names for this Condition? (Also known as/Synonyms)
- Cutaneous Neuroendocrine Carcinoma
- Primary Small Cell Carcinoma of Skin
- Trabecular Skin Carcinoma
What is Merkel Cell Carcinoma? (Definition/Background Information)
- Merkel Cell Carcinoma (MCC) is a rare cancer of the skin, which usually occurs in elderly individuals (in their late 60s). Sun exposure and immunodeficiency are key risk factors for the condition
- Merkel Cell Carcinoma develops in the sun-exposed areas of the body. The most common area of occurrence being the head and neck region. MCC manifests as a skin tumor (nodule) that can grow rapidly in size
- Mohs Micrographic Surgery followed by chemotherapy and radiation therapy may be necessary to treat the malignancy. Merkel Cell Carcinoma can be fatal, if it is not treated promptly or even following optimal care
Who gets Merkel Cell Carcinoma? (Age and Sex Distribution)
- Merkel Cell Carcinoma usually occurs in elderly individuals; an increased incidence being associated with adults who are in their 60s
- Both males and females are affected by the tumor, though it is more common in men than women (in a 2:1 ratio)
- A majority of the tumors occur among Caucasians. The tumor is very rare among individuals with dark-colored skin
- Merkel Cell Carcinoma is seen all over the world; there is no particular geographical restriction noted
What are the Risk Factors for Merkel Cell Carcinoma? (Predisposing Factors)
The risk factors for Merkel Cell Carcinoma include:
- Sun exposure
- HIV infection and AIDS affected individuals
- Solid organ (such as kidney, heart, lung, and liver) transplant patients
- Individuals who remain immunodeficient for long periods; such as those undergoing chronic steroidal therapy, those with autoimmune disorders, among others
It is important to note that having a risk factor does not mean that one will get the condition. A risk factor increases one’s chances of getting a condition compared to an individual without the risk factors. Some risk factors are more important than others.
Also, not having a risk factor does not mean that an individual will not get the condition. It is always important to discuss the effect of risk factors with your healthcare provider.
What are the Causes of Merkel Cell Carcinoma? (Etiology)
The exact cause for Merkel Cell Carcinoma (MCC) is presently unknown. Research is being currently conducted to determine the exact cause of the condition.
- Some cases of MCC have shown chromosomal abnormalities in chromosome 1 (in the short arm of chromosome 1). Such chromosomal abnormalities have been noted in cancers such as neuroblastoma and melanoma. Some researchers believe that these tumor groups may be related to each other
- Besides, over half of all MCCs have a specific type of chromosomal abnormality, called trisomy of chromosome 6
- The gene responsible for the development of the carcinoma is currently unknown
What are the Signs and Symptoms of Merkel Cell Carcinoma?
The following are the clinical signs and symptoms of Merkel Cell Carcinoma (MCC):
- A single painless dome-shaped nodule, or occasionally the nodule may be present as a plaque, which is reddish in color. The skin over the plaques may ulcerate
- The mass/nodule and the reddish discolored area (plaque), is not itchy
- The mass grows rapidly. In just a matter of few weeks or months, the tumor can become large and readily noticeable
- The most common areas of skin that are involved with MCC include the head and neck region, arms, and legs
- In a majority of the cases the tumor size measures 0.5 cm to 2 cm
How is Merkel Cell Carcinoma Diagnosed?
The diagnosis of Merkel Cell Carcinoma is as follows:
- Medical history assessment with a thorough physical examination
- Chest X-ray
- CT scan of chest and abdomen region
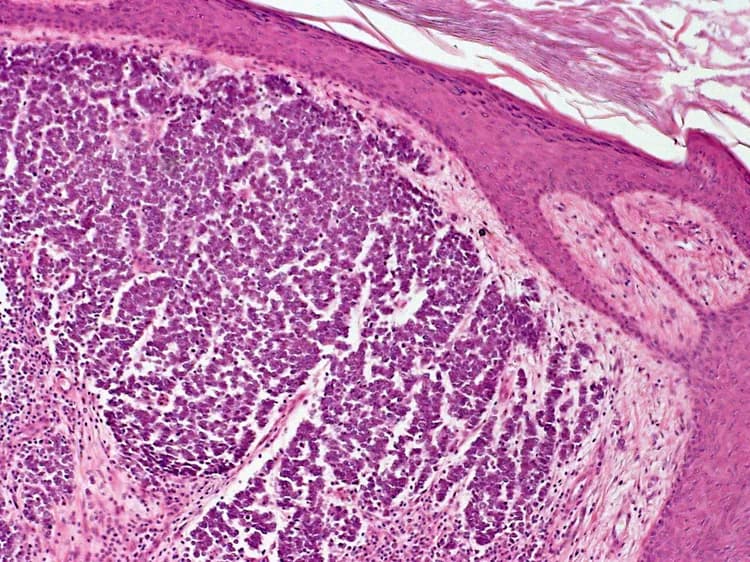
- Skin biopsy of the lesion (mass); the skin biopsy is examined by a pathologist under the microscope, to arrive at a definitive diagnosis
Many clinical conditions may have similar signs and symptoms. Your healthcare provider may perform additional tests to rule out other clinical conditions to arrive at a definitive diagnosis.
What are the possible Complications of Merkel Cell Carcinoma?
The complications of Merkel Cell Carcinoma (MCC) include:
- Emotional stress
- Metastasis (spreading of the cancer) to distant organs
- Recurrence of MCC at the original tumor site after initial surgery to treat the condition
How is Merkel Cell Carcinoma Treated?
Treatment measures for Merkel Cell Carcinoma:
- After the initial biopsy (to aid in diagnosis), the mass is completely excised through surgical resection. Occasionally, a dissection of the lymph nodes in the neck region, may also have to be performed
- Mohs Micrographic Surgery is the preferred initial surgical choice
- Sentinel lymph node biopsy can determine the presence of lymph node metastases
- Radiographic imaging to determine distant metastases may be performed
- In case of metastatic Merkel Cell Carcinoma, chemotherapy and radiation therapy, may have to be additionally administered
How can Merkel Cell Carcinoma be Prevented?
Currently there are no known methods to prevent the formation of Merkel Cell Carcinoma.
What is the Prognosis of Merkel Cell Carcinoma? (Outcomes/Resolutions)
- The prognosis of Merkel Cell Carcinoma depends upon the stage of the tumor. If the tumor is localized to the skin, then complete excision of the tumor through surgery can be curative
- If the tumor is of a higher stage (if tumor has spread to other parts of the body), then the prognosis is guarded
- The prognosis is worse if the tumor is diagnosed in an older adult, is located in the head and neck region, has a size greater than 2 cm, and the individual is immunocompromised
- If the tumor has a fast growth rate, as determined during a microscopic examination by the pathologist, then the tumor outcome may be worse
- If the tumor has spread into the blood vessels, termed angiolymphatic invasion (as established upon a microscopic examination by the pathologist); then, this factor also makes for a poor prognosis
Additional and Relevant Useful Information for Merkel Cell Carcinoma:
- Approximately 500 new cases of Merkel Cell Carcinomas are diagnosed in the United States each year
- The pathologist may perform additional testing to help with the diagnosis. Such tests may include immunostains, such as cytokeratins, epithelial membrane antigen, cytokeratin 20, thyroid transcription factor I (TTF-1), chromogranin, synaptophysin, neuron specific enolase, Bombesin, somatostatin, calcitonin, gastrin, CD117, and CD 99. The tumor is usually positive for the above mentioned immunochemical stains
- The tumor is negative for immunostains, such as leukocyte common antigen and S100 protein. The staining pattern helps a pathologist arrive at a correct diagnosis
Related Articles
Test Your Knowledge
Asked by users
Related Centers
Related Specialties
Related Physicians
Related Procedures
Related Resources
Join DoveHubs
and connect with fellow professionals


0 Comments
Please log in to post a comment.