Malignant Pilomatricoma
What are the other Names for this Condition? (Also known as/Synonyms)
- Calcifying Epitheliocarcinoma
- Malignant Pilomatrixoma
- Pilomatrical Carcinoma
What is Malignant Pilomatricoma? (Definition/Background Information)
- Pilomatricoma is a benign and generally slow-growing skin tumor of the hair follicle. It is common and occurs on the skin as a cystic nodule, usually in the head and neck region
- Malignant Pilomatricoma is an extremely rare tumor that may develop spontaneously, when there is no history of benign Pilomatricoma. In many cases, malignancy may also occur from benign Pilomatricomas
- Generally, there are two kinds of Pilomatricomas:
- Sporadic type of Pilomatricoma, in which a single tumor is observed
- Familial type of Pilomatricoma, in which multiple tumors are observed. It often occurs in association with certain genetic conditions
- The cause of Malignant Pilomatricoma may be related to genetic factors for both types (familial and sporadic). The condition is mostly observed in elderly men
- This cancerous tumor type may infiltrate local tissues, but only rarely metastasizes. Recurrence after removal of Malignant Pilomatricoma can also be noted
- In majority of cases, a complete surgical excision is the preferred mode of treatment for this malignant tumor. In rare cases of metastasis, a combination of chemotherapy, radiation therapy, and surgical procedures may be used
- The outcome for an individual with Malignant Pilomatricoma depends upon various factors, but is usually good with appropriate treatment
Who gets Malignant Pilomatricoma? (Age and Sex Distribution)
- Malignant Pilomatricoma is a very rare type of tumor that usually occurs in elderly adults. Occasionally, it can occur in children and young adults
- Both males and females may be affected, though males are affected more than females
- Individuals of all racial and ethnic background may be affected. Worldwide, only 50 cases of Malignant Pilomatricoma have been reported
What are the Risk Factors for Malignant Pilomatricoma? (Predisposing Factors)
- Currently, no risk factors have been identified for Malignant Pilomatricoma in a majority of the cases
- In some cases, the presence of a benign Pilomatricoma is a risk factor
- Furthermore, the incidence of benign Pilomatricoma is increased in individuals with a family history of genetic disorders such as:
- Steinert syndrome
- Turner syndrome
- Gardner syndrome
- Sotos syndrome
It is important to note that having a risk factor does not mean that one will get the condition. A risk factor increases ones chances of getting a condition compared to an individual without the risk factors. Some risk factors are more important than others.
Also, not having a risk factor does not mean that an individual will not get the condition. It is always important to discuss the effect of risk factors with your healthcare provider.
What are the Causes of Malignant Pilomatricoma? (Etiology)
The cause of development of Malignant Pilomatricoma is presently unknown.
- In some rare cases, a benign Pilomatricoma may transform into a cancerous form
- In many cases, a random development of the tumor seems to take place, when there is no presence of a benign Pilomatricoma
What are the Signs and Symptoms of Malignant Pilomatricoma?
The signs and symptoms of Malignant Pilomatricoma include:
- It usually occurs as a single, raised cystic nodule on the skin
- Multiple tumors are noted in association with other syndromes (underlying conditions)
- It is typically a slow-growing tumor that occurs deep in the skin. Due to this, it is sometimes mistaken for a lymph node
- It can range in size from 0.5 to 10 cm and can infiltrate local tissues
- The skin over the nodule may ulcerate and bleed
- These nodules can occur at any location in the body, but they are commonly observed in the head and neck region
- The tumors may also calcify
In case Malignant Pilomatricoma is associated with underlying genetic disorders, the signs and symptoms of the disorder will be present.
How is Malignant Pilomatricoma Diagnosed?
A diagnosis of Malignant Pilomatricoma may involve the following:
- A thorough medical history and physical examination
- Dermoscopy: It is a diagnostic tool where a dermatologist examines the skin using a special magnified lens
- Blood tests may indicate increased levels of calcium (hypercalcemia) and parathyroid hormone (PTH)
- A fine needle aspiration may be performed, if the nodule is mistaken for a lymph node. This can lead to a misdiagnosis of metastatic squamous cell carcinoma
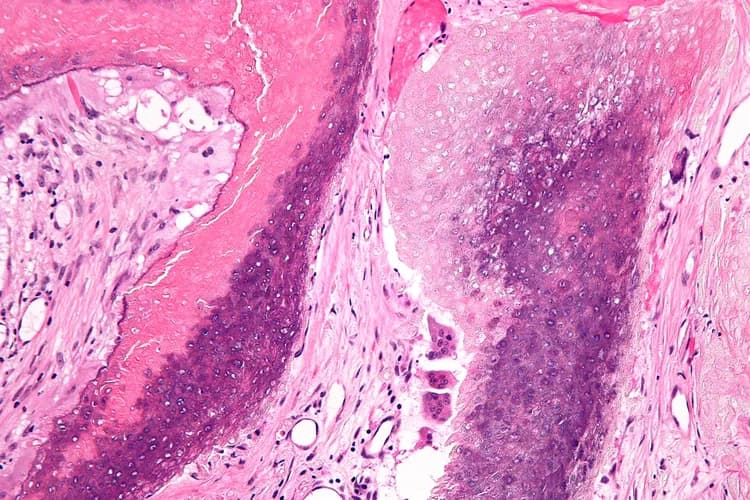
- Skin biopsy: A skin biopsy is performed and sent to a laboratory for a pathological examination. The pathologist examines the biopsy under a microscope. After putting together clinical findings, special studies on tissues (if needed) and with microscope findings, the pathologist arrives at a definitive diagnosis
- Specific tests may be undertaken based on the underlying conditions that are associated with Malignant Pilomatricoma (if any)
Many clinical conditions may have similar signs and symptoms. Your healthcare provider may perform additional tests to rule out other clinical conditions to arrive at a definitive diagnosis.
What are the possible Complications of Malignant Pilomatricoma?
The complications from Malignant Pilomatricoma may include the following:
- Even though metastasis of the tumor is rare, it can take place. In such cases, the cancer may spread to the local lymph nodes and lungs
- The tumors often occur in the head and neck region and may present cosmetic issues in some individuals
- Ulceration and bleeding of the tumors may cause an infection (bacteria or fungi), leading to scarring
- Sometimes, recurrence of the tumor after its surgical removal may be observed
- Complications may arise from any inherited genetic disorder that is associated with the presence of multiple tumors
How is Malignant Pilomatricoma Treated?
The treatment of Malignant Pilomatricoma may be undertaken as follows:
- In most cases, a wide surgical excision and removal of the entire tumor is the preferred treatment option. This may be followed by radiation therapy and/or chemotherapy
- If the tumor has metastasized (in rare cases), then a combination of chemotherapy, radiation therapy, and invasive procedures may be used to treat the tumor
- Post-operative care is important: One must maintain minimum activity levels, until the surgical wound heals
- Follow-up care with regular screening and check-ups are important and encouraged
How can Malignant Pilomatricoma be Prevented?
- Current medical research has not established a method of preventing Malignant Pilomatricoma
- Regular medical screening at periodic intervals with blood tests, scans, and physical examinations are mandatory due to its metastasizing potential and possibility of recurrence. Often several years of active vigilance is necessary
What is the Prognosis of Malignant Pilomatricoma? (Outcomes/Resolutions)
- The prognosis of Malignant Pilomatricoma depends upon the stage of the tumor, the location of the tumor, and the age and health of the individual
- Early diagnosis and treatment of the tumor generally yields a better outcome and is important
- The prognosis also depends upon the presence of any underlying genetic condition the tumor is associated with
Additional and Relevant Useful Information for Malignant Pilomatricoma:
- There is no evidence to prove that certain foods contribute to Pilomatricoma development
- Cleaning the skin too hard with strong chemicals or soaps may aggravate the skin condition. Care must be taken avoid strong soaps and chemicals that could potentially worsen the condition
- The presence of dirt on the body is not a causative factor for the condition. However, it helps to be clean and hygienic, which may help the condition from getting worse
Related Articles
Test Your Knowledge
Asked by users
Related Centers
Related Specialties
Related Physicians
Related Procedures
Related Resources
Join DoveHubs
and connect with fellow professionals


0 Comments
Please log in to post a comment.