Lung Cancer
What are the other Names for this Condition? (Also known as/Synonyms)
- Pulmonary Cancer
- Cancer of the Lung
What is Lung Cancer? (Definition/Background Information)
- Lung Cancer is a type of cancer that affects the lungs. It has one of the highest mortality rates among men and women with cancer
- Any individual can develop Lung Cancer, although individuals who smoke cigarettes remain at the highest risk for the condition
- If Cancer of the Lung is detected and diagnosed early, the prognosis is usually good. However, at this time, there are no appropriate screening methods present for Lung Cancer, which can adequately improve an individual’s survival rate or precisely identify this disease
- The type of normal lung cells that transform to malignancy can determine the type of Lung Cancer. The type of Lung Cancer one is diagnosed with determines an appropriate treatment method for the same
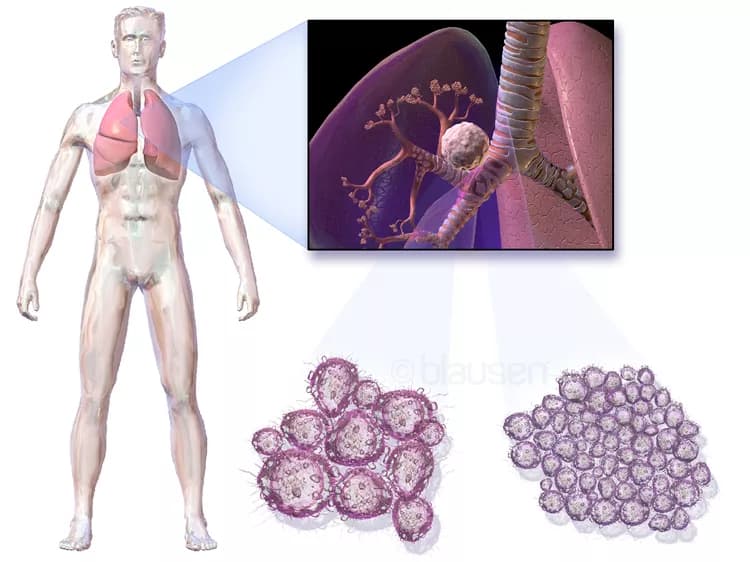
Lung Cancer is categorized into two types - Non-Small Cell Lung Cancer (NSCLC) and Small-Cell Lung Cancer (SCLC). It is difficult to diagnose NSCLC, because the cancer cells are underdeveloped when a pathologist looks under a microscope. Types of Non-Small Cell Lung Cancer include:
- Adenocarcinoma of the lung
- Squamous cell carcinoma
- Large cell carcinoma of the lungs
Small-Cell Lung Cancer is a fast-growing type of Lung Cancer that metastasizes faster than non-small cell types. This type comprises about 15% of all Lung Cancer cases. The types of SCLC include:
- Small cell carcinoma (SCC)
- Combined small cell lung carcinoma (c-SCLC)
Who gets Lung Cancer? (Age and Sex Distribution)
- Individuals under the age of 40 years are rarely diagnosed with Lung Cancer. The majority of Lung Cancer cases are detected and diagnosed in adults over the age of 65 years
- Men have a higher rate of incidence than women, although the gap is narrowing
- African Americans have an increased risk of the condition over any other race or ethnic group
What are the Risk Factors for Lung Cancer? (Predisposing Factors)
The underlying cause of Lung Cancer is unknown at this time, although physicians believe that certain factors may increase an individual’s risk for the condition. These risk factors include:
- Advancing age: The risk increases with age and most cases occur in individuals over the age of 65 years
- Smoking: Smoking cigarettes, cigars, or pipes, increase the risk due to damaging chemicals being inhaled into the lungs. When people inhale cigarette smoke, the harmful chemicals travel through the bronchi (breathing tube) and into the lungs. This result in the lung tissue cells being exposed to cancer-causing substances (carcinogens) contained in the smoke. The cilia’s (a small hair-like structure located in the cell lining) function is to clear contaminants out of the bronchi. Prolonged smoking damages the cilia, resulting in reduced clearance of the carcinogens. This can lead to an increased risk for developing Lung Cancer
- Exposure to secondhand smoke: Individuals who do not smoke, but live with smokers, also have an increased risk. This may also come about through a workplace exposure to tobacco smoke
- Exposure to asbestos and other harmful chemicals: Prolonged exposure to asbestos may increase an individual’s risk of Lung Cancer. Other harmful chemicals include arsenic, chromium, nickel, and tar
- Radon: Radon, a colorless, odorless, and tasteless radioactive gas is produced by the natural breakdown of uranium in soil and rocks. In certain parts of the United States, hazardous levels of radon gas can develop inside buildings or households. Individuals exposed to excessive amounts of radon gas are vulnerable to Lung Cancer
- Race: African Americans are at an elevated risk than individuals of any other race
- Family history: Individuals with one or more immediate family members or relatives with a history of Lung Cancer
- Personal history: Patients, who have previously had Lung Cancer, have an increased risk of its reoccurrence
- Certain lung diseases: Lung diseases, such as tuberculosis, bronchitis, or chronic obstructive pulmonary disease, over a prolonged period of time, may increase an individual’s risk
- Radiation therapy to the chest: Individuals, who had radiation therapy to the chest for another cancer, are increasingly prone to Lung Cancer
- Air pollution: Exposure to polluted air may increase any individual’s risk. This is true, especially in the case of smokers, who are exposed to air pollution, than the non-smokers
It is important to note that having a risk factor does not mean that one will get the condition. A risk factor increases one's chances of getting a condition compared to an individual without the risk factors. Some risk factors are more important than others.
Also, not having a risk factor does not mean that an individual will not get the condition. It is always important to discuss the effect of risk factors with your healthcare provider.
What are the Causes of Lung Cancer? (Etiology)
The direct cause of Lung Cancer is not entirely known at this time; although, physicians believe certain factors may be responsible for the disease, which include:
- Smoking cigarettes, cigars, or pipes, increase an individuals’ risk for Lung Cancer due to the damaging chemicals being inhaled into the lungs. When cigarette smoke is inhaled, the harmful chemicals travel through the bronchi (breathing tube) and into the lungs. This result in the lung tissue cells being exposed to carcinogens present in the smoke. Cilia, located in cells lining the bronchi, remove contaminants out of the bronchi. Smoking (over many years) damages the cilia, resulting in reduced clearance of carcinogens from lung. This factor may contribute to the development of Lung Cancer
- Radon, a colorless, odorless, and tasteless, radioactive gas is produced by the natural breakdown of uranium in soil and rocks. In certain parts of the United States, hazardous levels of radon gas can develop in building or households. Individuals exposed to excessive amounts of radon gas may have an increased risk of Lung Cancer
- Prolonged exposure to asbestos and other harmful chemicals such as arsenic, chromium, nickel, and tar
What are the Signs and Symptoms of Lung Cancer?
Early-stage Lung Cancer rarely causes any signs and symptoms, and may initially make for a difficult diagnosis. Besides, several of the primary symptoms may result from non-malignant conditions too. The overlapping signs and symptoms may result in a delayed diagnosis of Lung Cancer in some cases.
Lung Cancer usually begins to show some signs or symptoms during the later stages of the disease, which may include:
- Shortness of breath (dyspnea)
- Abnormal, persistent pain in the chest
- Abnormal pain in bones
- Fatigue
- Weight loss
- Coughing up blood (hemoptysis)
- Headache (cephalgia)
- Anorexia (loss of appetite)
How is Lung Cancer Diagnosed?
There are a variety of tests the healthcare providers may use to detect, locate, and diagnose Lung Cancer, and whether it has potentially spread to other regions. A surgical procedure called a biopsy (usually performed by a radiologist or a cardiothoracic surgeon) is the only test a physician uses in order to make a definitive diagnosis of Lung Cancer. However, if a physician is unable to perform a lung biopsy due to the risk of damaging vital organs, additional tests will be recommended that may include:
- Physical examination: During a physical exam, a physician will check the individual’s overall health status, listen to their breathing, and check for possible fluid buildup in the lungs (auscultation)
- Chest X-ray: Two-dimensional pictures using tiny amounts of radiation are taken in order to detect any tumors, or other medical issues associated with the lungs such as pneumonia. Tumors inside the lungs can be detected with a chest X-ray, although sometimes these tumors may be too small to be visualized
- Computerized tomography (CT) scan: Also known as CAT scan, this radiological procedure creates detailed three-dimensional images of structures inside the body. CT scans are not a tool of preference to detect Lung Cancer; although, CT scans may be helpful in detecting recurrences, or if the cancer has metastasized to the surrounding lymph nodes of the lungs
- Positron emission tomography (PET): A PET scan is a nuclear medicine imaging technique that uses three-dimensional images to show how tissue and organs are functioning. A small amount of radioactive material may be injected into a vein, inhaled, or swallowed. A PET scan is also helpful in detecting recurrences, or if any metastasis (to the surrounding lymph nodes of the lungs) has occurred
- Magnetic resonance imaging (MRI) scan: An MRI scan uses magnetic fields that create high-quality pictures of certain body parts, such as tissues, muscles, nerves, and bones. These high-quality images may indicate to a physician if any Lung Cancer is present
- Sputum cytology: Sputum cytology is test that involves the collection of mucus (sputum), coughed-up by a patient. After the mucus is collected, a pathologist examines them in an anatomic pathology laboratory for any cell abnormalities indicative of Lung Cancer
- Bone scan: A bone scan is a nuclear imaging test that involves injecting a radioactive tracer into an individual’s vein. Bone scans are primarily used to detect if the cancerous tumor in the lung has metastasized to the bones
- Bone marrow biopsy: Bone marrow is a soft tissue found within the bones. Occasionally with Lung Cancer, a bone marrow biopsy is used to detect blood abnormalities, or if a physician thinks that metastasis to the bone marrow may have occurred
A biopsy refers to a medical procedure that involves the removal of cells or tissues, which are then examined by a pathologist. Different biopsy procedures include:
- Bronchoscopy: During bronchoscopy, a special medical instrument, called a bronchoscope, is inserted through the nose and into the lungs to collect small tissue samples. These samples are then examined by a pathologist, after the tissues are processed in an anatomic pathology laboratory
- Thoracentesis: During thoracentesis, a special medical device, called a cannula, is used to remove the fluid between the lungs and the chest wall. A pathologist then examines the extracted cells from the fluid in an anatomic pathology laboratory to determine any signs of Lung Cancer
- Thoracoscopy: During thoracoscopy, a surgical scalpel is used to make very tiny incisions into the chest wall. A medical instrument, called a thoracoscope, is then inserted into the chest, in order to examine and remove tissue from the chest wall, which are then examined further
- Thoracotomy: Thoracotomy is a surgical invasive procedure with special medical instruments to open-up the chest. This allows a physician to remove tissue from the chest wall or the surrounding lymph nodes of the lungs. A pathologist will then examine these samples under a microscope after processing the tissue in a laboratory
- Mediastinoscopy: During mediastinoscopy, a surgical scalpel is used to make very tiny incisions above the breastbone. Then, a medical instrument called a mediastinoscope is inserted into the chest wall to examine and remove samples. These tissue samples are processed and then examined under a microscope for any abnormalities
- Fine needle aspiration biopsy (FNAB): During the fine needle aspiration biopsy, a device called a cannula is used to extract tissue or fluid from the lungs or surrounding lymph nodes. These are then examined in an anatomic pathology laboratory, in order to look for any signs of Lung Cancer
- Autofluorescence bronchoscopy: It is a bronchoscopic procedure in which a bronchoscope is inserted through the nose and into the lungs and measure light from abnormal precancerous tissue. Samples are collected for further examination by a pathologist
Many clinical conditions may have similar signs and symptoms. Your healthcare provider may perform additional tests to rule out other clinical conditions to arrive at a definitive diagnosis.
What are the possible Complications of Lung Cancer?
The complications of Lung Cancer may include:
- Dyspnea (or shortness of breath): Individuals with Lung Cancer may have an increased risk of exhibiting signs of dyspnea, if the cancerous tumor expands to block important large or small airways of the chest or lung
- Hemoptysis (coughing-up blood): Individuals may cough-up blood due to excessive amounts of blood in the airways
- Pain: Advanced stages of Lung Cancer that has metastasized to the pleural cavity (lining surrounding the lungs) or other areas of the body may cause excessive pain and agony
- Pleural effusion (fluid in the chest): Excessive fluid accumulation resulting from a cancerous tumor spreading inside or outside of the lungs
- Lung Cancer that spreads to other parts of the body: There is an increased risk of the cancer metastasizing (or spreading) to other parts of the body such as the adrenal gland, liver, bones, and to the other lung
How is Lung Cancer Treated?
Treatment for Lung Cancer depends on a number of factors, including the histological type of Lung Cancer, the stage of the cancer, the overall health, and treatment preferences of the patient.
Surgery for Lung Cancer:
The recommended treatment for individuals with Lung Cancer is to remove the part of the lung that contains the cancerous growth. Thoracotomy is the surgical removal of all or part of the lungs and is usually performed by a cardiothoracic surgeon. There are many different approaches a cardiothoracic surgeon may use to combat Lung Cancer. These include:
- Wedge resection: Wedge resection is a partial removal of the wedge-shape portion of the lung that contains cancerous cells (along with any surrounding healthy tissue)
- Segmentectomy: Segmentectomy is also the partial removal of the cancerous lung and any surrounding healthy tissue
- Lobectomy (pulmonary lobectomy): Lobectomy is the most common type of surgical procedure performed for Lung Cancer, to partially remove a portion of a lung
- Sleeve lobectomy: Sleeve lobectomy is also a surgical procedure to partially remove a portion of the lung and a part of the airway (bronchus)
- Pneumonectomy: It is the surgical removal of the entire lung
During surgery, the surgeon will also examine the surrounding areas of the lung, looking for any signs of cancer metastasis.
Chemotherapy:
- Chemotherapy is a treatment using drugs to kill cancer cells. In this treatment for Lung Cancer, generally a combination of two or more chemotherapy drugs are used
- These drugs may be administered intravenously (through a vein in your arm) or orally (in a pill-form). Drugs inserted directly into the bloodstream, travel through the body and kill the cancer cells
- Such drugs may be recommended for patients with advanced Lung Cancer that has spread to other body parts
Radiation therapy:
- Radiation therapy attempts to destroy cancer cells by aiming high-energy beams at the cancer cells
- Radiation therapy can either be administered by a machine outside the body (external beam radiation) or administered internally, by a device positioned directly at or close to the malignant tumor, inside the lungs (brachytherapy)
- Radiation therapy may be used before surgery to decrease the size of a tumor, thus allowing for its easier removal; or after surgery, to kill any remaining cancer cells
- Radiation therapy and chemotherapy are sometimes used as a combination tool
Targeted drug therapy:
Targeted drug therapy is a relatively new medical treatment used to target abnormal cancer cells and reduce the chance of cancer spreading to other parts of the body. There are currently two types of targeted drug therapy treatments used for Lung Cancer that include:
- Bevacizumab (Avastin): Bevacizumab is a target therapeutic drug used together with chemotherapy, and designed to disrupt or obstruct the formation of new blood vessels in the tumor. However, individuals who take Bevacizumab, have an increased risk of bleeding, blood clots, and high blood pressure
- Erlotinib (Tarceva): Epidermal growth factor receptor (EGFR) is a protein located on the exterior of a cell. Erlotinib is another targeted therapeutic drug, designed to disrupt the protein on cancerous cells from expanding and dividing. The drug is administered to patients orally (in pill-form) and it is usually taken in combination with chemotherapy
How can Lung Cancer be Prevented?
Although there are no preventable measures for Lung Cancer, various steps can be taken to help decrease the risk of its formation. These measures include:
- Smoking cessation: When an individual quits smoking even after smoking for several years, they reduce their risk for Lung Cancer by 30-50% after 10 years. Individuals under the age of 50 years, who quit smoking, may ultimately have the same reduced risk as a non-smoker. Nevertheless, approximately 10-15% of all Lung Cancer related deaths are seen in non-smokers
- Physical activity: Obesity increases the risk for Lung Cancer due to increased levels of inflammation in the body, which reduces the body immunity. Individuals, who participate in a modest amount of physical activity, may decrease their risk
- Adequate consumption of fruits and vegetables: A healthy diet, low in saturated fats and rich in many fruits and vegetables, may help decrease one’s risk for Lung Cancer. Regular consumption of soy-based foods incorporated into a diet also decreases one’s risk
- Avoiding exposure to certain chemicals: Individuals who work with certain harmful chemicals can lessen their exposure to the chemicals, by following proper usage principles and occupational safety instructions. Prolonged exposure to asbestos and other harmful chemicals (arsenic, chromium, nickel, and tar), may increase the risk of Lung Cancer. This risk is multiplied in smokers who are exposed to these harmful chemicals.
- Avoid exposure to secondhand smoke: Individuals, who are exposed to secondhand tobacco smoke, such as caused by living with a smoker or from workplace exposure, also have an increased risk for developing Lung Cancer
- Avoid exposure to radioactive gas: Radon, a radioactive gas, produced by the natural breakdown of uranium in soil and rocks may develop to hazardous levels inside building spaces. Individuals exposed to excessive amounts of radon gas are vulnerable to Lung Cancer
- Limit alcohol consumption: Alcoholic beverages have been linked to increasing an individuals’ risk for certain types of cancers, such as those affecting the lungs, mouth, throat, esophagus, breast, colon, and liver. Scientists are not entirely certain at this time, but alcohol may release certain harmful chemicals or generate toxic substances, after it is digested and metabolized in the body. Increased estrogen levels, identified as increasing one’s risk of certain cancers, such as breast cancer, ovary cancer, and endometrial cancer, may be associated with excessive alcohol consumption. Certain food nutrients that help prevent cancer may diminish due to excessive amounts of alcohol consumption, thereby increasing Lung Cancer risk
What is the Prognosis of Lung Cancer? (Outcomes/Resolutions)
- The prognosis for Lung Cancer depends on the individual’s age, physical health, location of the tumor, and the stage and grade of cancer. The lower the stage and grade of cancer, the better is the prognosis
- Unfortunately, a high-mortality rate of Lung Cancer is due to the relative ineffectiveness of treatments associated with the many forms of Lung Cancer and its subtle signs and symptoms resulting in a late diagnosis
- Lung Cancer has one of the highest mortality rates in the world. A majority of the diagnosed individuals do not survive beyond 5 years
Additional and Relevant Useful Information for Lung Cancer:
According to the American Cancer Society 2011 estimates in the United States, each year approximately 221,130 new cases of Lung Cancer (combining Non-Small Cell and Small-Cell Lung Cancer) will be diagnosed, and around 156,940 people will die from this condition.
Related Articles
Test Your Knowledge
Asked by users
Related Centers
Related Specialties
Related Physicians
Related Procedures
Related Resources
Join DoveHubs
and connect with fellow professionals

0 Comments
Please log in to post a comment.