What are the other Names for this Condition? (Also known as/Synonyms)
- Amazonic Pseudolephromatous Blastomycosis
- Jorge Lobo’s Disease
- Lacaziosis
What is Lobomycosis? (Definition/Background Information)
- Lobomycosis is a skin infection caused by the fungus Lacazia loboi. This fungus is found almost exclusively in South America and some Central American regions
- Lacazia loboi is generally found in dense forest areas with large water bodies/rivers and high humidity levels (relative humidity at about 75%). The pathogen is naturally found only in dolphins and humans, giving rise to an unsubstantiated speculation that the infection spreads from dolphins to humans
- Although the human disease is predominantly reported in South and Central America, the infection in dolphins is spreading and has been reported in the coasts of south Brazil, Indian Ocean, Western Pacific, Africa, Europe, and North Carolina (in the USA)
- Individuals who work with dolphins, forest workers, those who live in the forests of South and Central America, and scientists doing fieldwork in such forests, are at an increased risk of contracting Lobomycosis
- The fungus establishes itself when there is a break in the skin due to an injury, such as through cuts, scratches, insect or animal bites. After this event occurs, it can take a long time (up to 2 years) before the signs and symptoms of Lobomycosis are manifested in the individual
- The symptoms of the infection appear predominantly on exposed skin, such as on the ears, arms, and legs. Other body surfaces, such as the chest and face, may also be affected. Superficial or deep nodules and plaques (raised, smooth-surfaced, and hard lesions) may appear on the skin; these may be unpigmented or have different shades of pigmentation
- Lobomycosis can lead to complications, such as ulceration of the skin lesions and the development of recurrent lesions. In rare cases, the infection may result in squamous cell carcinomas
- Lobomycosis is diagnosed based on the presenting symptoms, travel or work history of the affected individual to the endemic regions, and microscopic examination of a lesion sample using specific stains, which is performed in a laboratory
- Removal of lesions and surrounding skin by surgery is considered the most effective method of treating this infection. The use of anti-fungal agents for treatment of Lobomycosis has not yielded satisfactory results
- The prognosis of Lobomycosis depends on the severity of the signs and symptoms, and response to surgery. Although there is a likelihood of a chronic infection, Lobomycosis is limited to the skin in most cases
Who gets Lobomycosis? (Age and Sex Distribution)
- From the cases reported thus far, individuals of all ages are susceptible to Lobomycosis
- Both male and female genders are at risk
- The exact prevalence of this infection is not known, although it is predominantly reported in some South and Central American countries including:
- South America: Brazil, Venezuela, Suriname, Ecuador, Bolivia, Peru, Guyana, French Guyana
- Central America: Mexico, Panama, and Costa Rica
- “Imported cases” of the infection, when an individual contracts the fungus in one of the countries (mentioned-above) and develops the symptoms after a lapse of time, have been reported from Canada, France, Germany, Greece, Netherlands, South Africa and the USA
What are the Risk Factors for Lobomycosis? (Predisposing Factors)
The following are some known risk factors for developing Lobomycosis:
- Living in or around the forests of South or Central America (the endemic regions)
- Occupations involving dense forest areas where the fungus is endemic including:
- Collecting resin from rubber trees
- Farming
- Fishing
- Scientific research
- Hunting
- Individuals, who come into contact with infected dolphins or dolphin tissues, including:
- Marine biologists
- Veterinarians
- Aquarium workers
- Workers involved in animal rescue operations
- Those involved in rehabilitation of injured dolphins
- Coming into contact with infected tissue from humans, who are:
- Physicians or healthcare providers
- Other medical personnel involved in the care of infected individual
- Laboratory technicians
It is important to note that having a risk factor does not mean that one will get the condition. A risk factor increases ones chances of getting a condition compared to an individual without the risk factors. Some risk factors are more important than others.
Also, not having a risk factor does not mean that an individual will not get the condition. It is always important to discuss the effect of risk factors with your healthcare provider.
What are the Causes of Lobomycosis? (Etiology)
- Lobomycosis is caused by the fungus Lacazia loboi. This fungus is present in the soil, vegetation, and water, in the forests of certain Central and South American regions
- The fungus gains entry into the skin through a break/cut on the skin. This may be from nicks, scratches, insect bites, animal bites, and even through punctures from accidental stingray stings
- Once established, the infection sets in gradually, with a long latent period (several months to even 2 years) before the symptoms are manifested
- The infection can occur while dealing with contaminated tissue from a dolphin, or while working with an infected mammal
- Infection in humans can also occur from tissue samples that are being processed for diagnosis, or during procedures involving the lesions
What are the Signs and Symptoms of Lobomycosis?
The signs and symptoms of Lobomycosis may develop slowly, over a period of months or years. The site and severity of infection may vary between infected individuals.
Some common signs and symptoms include:
- Skin lesions that looks similar to a pimple, which may be superficial or deep
- The presence of nodules or plaques that are:
- Covered in shiny skin, which is smooth and unbroken
- Without any visible spider veins
- Flesh-colored, or light or dark pink
- Fibrous in appearance
- Similar in appearance to a scar
- Occasionally, the skin lesion may appear like a wart
- Disintegration of outer layers of affected skin (maceration) in very moist environment during rainy seasons, leading to ulceration
- Formation of blisters and discharge of thick, yellow liquid (observed in rare cases)
- Spreading of the primary infection to surrounding skin, causing an increasing in the surface area affected by the lesions
- Itching (seen in advanced cases)
- Dysesthesia or abnormal sensations on the skin (observed in individuals with advanced infection)
How is Lobomycosis Diagnosed?
The diagnosis of Lobomycosis is made on the basis of:
- A thorough physical examination and an assessment of one’s symptoms
- An evaluation of the affected individual’s medical, work, and travel history
- Microscopic observation of skin by scraping a lesion and mounting it for viewing
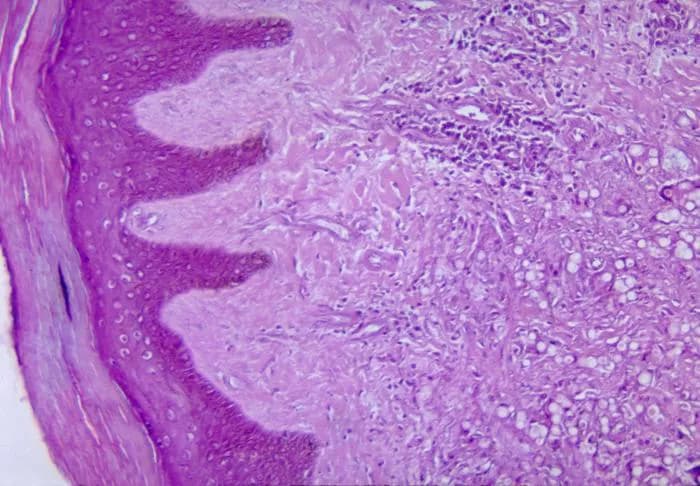
- Biopsy of lesions for
- Staining with Hematoxylin and Eosin (H&E) staining to check whether the infection is superficial or deep
- Staining with periodic acid-Schiff, Grocott methenamine silver, or calcofluor white stains to observe fungal cells
Many clinical conditions may have similar signs and symptoms. Your healthcare provider may perform additional tests to rule out other clinical conditions to arrive at a definitive diagnosis.
What are the possible Complications of Lobomycosis?
The potential complications that could arise in those with Lobomycosis include:
- The infection can become chronic
- Severe itching and abnormal sensations affecting the quality of life
- Spread of infection to other sites, such as to the lymph nodes
- The skin lesions spreading and causing disfigurement and distress
- Ulcerating lesions
- In rare cases, longstanding infection can result in the development of malignancy (squamous cell carcinoma) in the affected area
How is Lobomycosis Treated?
The type of treatment and follow-up for Lobomycosis is typically determined by a healthcare professional on a case-by-case basis. The most effective treatment for this fungal infection is surgery.
- The lesions and the surrounding tissue are removed and the wound dressed to allow proper healing
- Care is taken to remove and sanitize infected instruments to avoid re-infection of the surgical site
- Some antifungal medication may be recommended to prevent re-infection of surgical sites
How can Lobomycosis be Prevented?
Currently, there is no vaccine available to prevent the development of Lobomycosis. However, the following measures may be considered towards prevention:
- Wearing protective clothing to avoid exposing broken skin to contaminated surfaces and tissues
- Regular medical screening at periodic intervals with tests, and physical examinations are crucial, and highly recommended
Active research is currently being performed to explore the possibilities for treatment and prevention of Lobomycosis.
What is the Prognosis of Lobomycosis? (Outcomes/Resolutions)
- The prognosis of Lobomycosis is determined by the severity of infection and response to treatment
- There is a likelihood of chronic infection and spread of infection to different body parts. The quality of life may be affected owing to disfigurement
- In rare cases, longstanding infections can result in malignancy; such a complication can require further tests and suitable treatment
Additional and Relevant Useful Information for Lobomycosis:
The type of dolphins involved in the transmission of Lobomycosis is the bottle-nose dolphin.
Related Articles
Test Your Knowledge
Asked by users
Related Centers
Related Specialties
Related Physicians
Related Procedures
Related Resources
Join DoveHubs
and connect with fellow professionals

0 Comments
Please log in to post a comment.