What are the other Names for this Condition? (Also known as/Synonyms)
- Cavernoma of Liver
- Cavernous Hemangioma of Liver
- Hepatic Hemangioma
What is Liver Hemangioma? (Definition/Background Information)
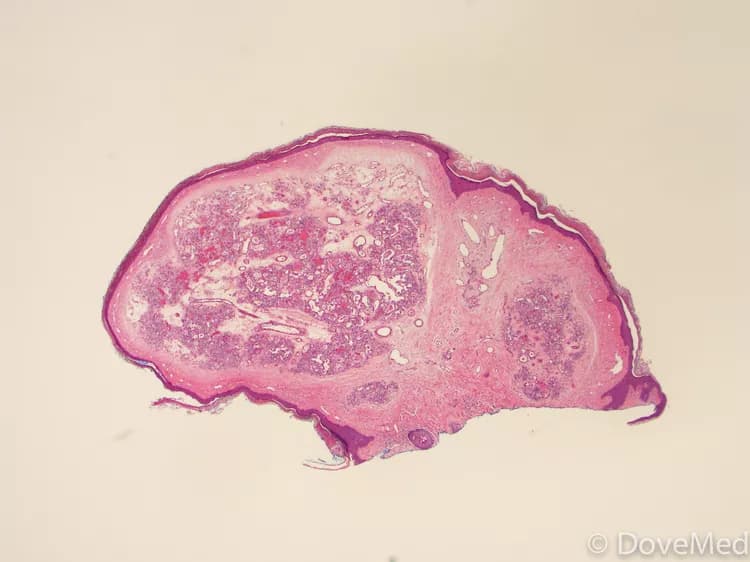
- Hemangiomas are benign malformations of blood vessels, which can occur in a variety of tissues, such as the brain, kidney, liver, lung, skin, and nasal cavity
- Liver Hemangiomas are non-cancerous, vascular tumors of the liver. It usually occurs as a single tumor, although multiple masses have been noted. These tumors are most often diagnosed in young and middle-aged individuals
- Women, who have been pregnant or are using hormone replacement therapies, are more likely to develop Liver Hemangiomas. The cause of formation of this benign tumor is not yet well understood; though some studies have shown that it can be congenital in nature (occurring at birth)
- Liver Hemangiomas are generally asymptomatic. In some individuals, signs and symptoms, such as pain in the upper right region of the abdomen, loss of appetite, nausea, and vomiting, may be noted. Pregnant women or women taking hormone-based medications may experience an increase in tumor size
- A majority of asymptomatic cases may require no treatment, but individuals with severe signs and symptoms may be treated through a surgical removal of the tumor, hepatic artery ligation, and radiation therapy
- The prognosis for Liver Hemangiomas is generally good. Smaller hemangiomas are not known to affect the liver’s ability to function; however, some tumors may grow large over time affecting liver function. In such cases, the prognosis is assessed on a case-by-case basis
Who gets Liver Hemangioma? (Age and Sex Distribution)
- Liver Hemangiomas most often occur in adult individuals between the ages of 30-50 years of age
- Women develop them more often than men; they also tend to frequently have larger tumors
- Liver Hemangiomas can affect individuals of all races and ethnicities
What are the Risk Factors for Liver Hemangioma? (Predisposing Factors)
Individuals with the following factors/conditions have a higher risk for developing Liver Hemangioma:
- Women, who have been pregnant are at an increased risk for developing Liver Hemangiomas than women who have never been pregnant
- Women, who have used hormone replacement therapy to treat menopausal symptoms are also more likely to be diagnosed with this tumor than women who did not receive such a therapy
It is important to note that having a risk factor does not mean that one will get the condition. A risk factor increases ones chances of getting a condition compared to an individual without the risk factors. Some risk factors are more important than others.
Also, not having a risk factor does not mean that an individual will not get the condition. It is always important to discuss the effect of risk factors with your healthcare provider.
What are the Causes of Liver Hemangioma? (Etiology)
The cause of Liver Hemangiomas is not yet well understood.
- However, some studies have shown that this condition is congenital (present from birth)
- Some researchers believe that Liver Hemangiomas are a type of birth defect (or birth malformations)
What are the Signs and Symptoms of Liver Hemangioma?
The majority of Liver Hemangiomas is generally asymptomatic and presents no signs and symptoms. In some individuals, the signs and symptoms may include:
- Pain in the upper right region of the abdomen
- Bleeding of the Liver Hemangioma
- Sense of fullness after eating only a small amount of food
- Loss of appetite
- Nausea and vomiting
The signs of a growing tumor include pain in the upper right region of the abdomen, nausea, and vomiting.
How is Liver Hemangioma Diagnosed?
A diagnosis of Liver Hemangioma may include the use of the following tests and procedures:
- Complete evaluation of medical history along with a thorough physical exam
- The following imaging techniques are generally used to diagnose Liver Hemangiomas:
- Ultrasound of the abdomen
- CT scan of the abdomen
- MRI scan of the abdomen
- SPECT scan of the abdomen
- Hepatic angiogram
- Liver function test
Many clinical conditions may have similar signs and symptoms. Your healthcare provider may perform additional tests to rule out other clinical conditions to arrive at a definitive diagnosis.
What are the possible Complications of Liver Hemangioma?
A few possible complications associated with Liver Hemangioma include:
- Pregnant women with Liver Hemangiomas may see an increase in the size of their tumors due to an increase in the hormone estrogen levels
- Liver Hemangiomas are known to rupture, causing severe bleeding
- Large tumor sizes may severely affect liver function
How is Liver Hemangioma Treated?
Liver Hemangiomas are generally asymptomatic and therefore, do not require any treatment, in a majority of cases.
- If a Liver Hemangioma causes significant pain or compresses on nearby structures in the abdomen, treatment may be considered
- Treatment options for Liver Hemangiomas depend on the tumor’s size, location, number (single or multiple tumors), patient's health, and preference
The treatment methods employed for Liver Hemangiomas may include:
- Surgical removal of the tumor
- Hepatic artery ligation
- Arterial embolization
- Radiation therapy
- Liver transplants may be considered for individuals with severe complications
How can Liver Hemangioma be Prevented?
- Currently, there is no effective prevention for the formation of Liver Hemangiomas
- Once diagnosed, close monitoring of the tumor may help prevent major complications from developing
- Pregnant women with the tumor may also need to be closely monitored to observe for any change in tumor size
What is the Prognosis of Liver Hemangioma? (Outcomes/Resolutions)
- Liver Hemangiomas are generally noncancerous and asymptomatic in nature. Also, smaller hemangiomas usually do not affect the liver’s functional ability. In such cases, the prognosis is generally excellent
- Liver Hemangiomas may grow larger over time. The prognosis of large hemangiomas that affect the liver function is assessed on an individual basis
Additional and Relevant Useful Information for Liver Hemangioma:
Please visit our Digestive Health Center for more physician-approved health information:
Related Articles
Test Your Knowledge
Asked by users
Related Centers
Related Specialties
Related Physicians
Related Procedures
Related Resources
Join DoveHubs
and connect with fellow professionals

0 Comments
Please log in to post a comment.