Granulomatosis with Polyangiitis (formerly Wegener Granulomatosis)
What are the other Names for this Condition? (Also known as/Synonyms)
- Granulomatosis with Polyangiitis (GPA)
- Midline Granulomatosis
- Wegener's Granulomatosis (formerly)
What is Granulomatosis with Polyangiitis? (Definition/Background Information)
- Granulomatosis with Polyangiitis (GPA; formerly known as Wegener's Granulomatosis) is a rare autoimmune disorder typically affecting the airways of the lungs, including the sinuses and parts of upper respiratory tract, the kidneys, and the small blood vessels of middle-aged adults
- GPA may be described as a syndrome (combination of signs and syndrome) caused by the formation of small areas of inflammation, called granulomas, in the lungs and kidney tissues, and inflammation in the small blood vessels, termed as vasculitis
- Different individuals may present different sets of signs and symptoms. The abnormal inflammation causes lung-related and kidney-related symptoms, thereby damaging the organs. In the lungs, it can result in the presence of a lung mass, which can sometimes be mistaken for lung cancer on radiological studies
- Granulomatosis with Polyangiitis is caused by an abnormal inflammation of the tissues and small blood vessels. However, the exact cause of such inflammation is unknown. The condition cannot be transmitted from individual to another. GPA is also not inherited from one’s parents (i.e., it cannot be transmitted to one’s children)
- The management of Granulomatosis with Polyangiitis involves an early diagnosis and prompt treatment that may involve immunosuppressive medication and/or surgical procedures. The outcomes of individuals with GPA depend on the severity of the condition and it varies from good to extremely poor
Who gets Granulomatosis with Polyangiitis? (Age and Sex Distribution)
- Granulomatosis with Polyangiitis is a very rare condition, predominantly affecting Caucasians. The incidence of the disorder is 1 in 33,000 in the Caucasian population
- It occurs in both males and females usually between the ages of 40 and 65 years
- All races are affected but the incidence is higher among Caucasians in comparison to African Americans. No other ethnic or geographical predisposition is seen
What are the Risk Factors for Granulomatosis with Polyangiitis? (Predisposing Factors)
The risk factors for Granulomatosis with Polyangiitis may include:
- Middle-age individuals have a higher risk, even though the condition may affect individuals of any age group
- All races can be affected, but the incidence is higher among the Caucasian population
Some studies have proposed a genetic predisposition in some individuals, but the studies are not yet conclusive.
It is important to note that having a risk factor does not mean that one will get the condition. A risk factor increases one's chances of getting a condition compared to an individual without the risk factors. Some risk factors are more important than others.
Also, not having a risk factor does not mean that an individual will not get the condition. It is always important to discuss the effect of risk factors with your healthcare provider.
What are the Causes of Granulomatosis with Polyangiitis? (Etiology)
According to current medical knowledge, the exact cause of Granulomatosis with Polyangiitis (GPA) disorder is not known.
- GPA is described as an autoimmune disorder that is caused by an abnormal inflammation of the tissues at several body regions. However, the exact cause of such inflammation is unknown
- Currently, active research is being performed to determine the cause. Some scientists believe that it is caused by an abnormal immune system response following a bacterial or a viral infection
Note: Granulomatosis with Polyangiitis can be confused with a disorder called polyarteritis nodosa with which it shares some similarities. However, both GPA and polyarteritis nodosa are two different conditions.
What are the Signs and Symptoms of Granulomatosis with Polyangiitis?
The signs and symptoms of Granulomatosis with Polyangiitis may vary greatly from one individual to another. Some may have mild symptoms, while others may have severe symptoms. The signs and symptoms may include:
- Upper respiratory tract symptoms such as sinusitis and middle ear infections. Frequent middle ear infections can cause hearing loss
- Chronic sinus inflammation causing congestion and pain around the sinuses of the face
- Constantly running nose with cold-like symptoms
- Drying of nasal mucous membranes can cause frequent nosebleeds
- Shortness of breath, cough, chest congestion can occur frequently
- Fever, fatigue, body aches, joint swelling with joint pains, and muscle weaknesses
- Eye symptoms including itching of eyes, conjunctivitis, eye pain, watering of eyes, and vision problems
- Skin symptoms with formation of skin ulcers, skin rashes and nodules that are often painful
- Presence of blood and protein in urine on urine analysis
- Nerve symptoms causing tingling and weakness affecting either a single nerve (mononeuropathy) or multiple nerves (polyneuropathy). The term mononeuropathy indicates that a single nerve is damaged, whereas polyneuropathy means that more than one nerve is damaged
How is Granulomatosis with Polyangiitis Diagnosed?
Granulomatosis with Polyangiitis (GPA) can cause several non-specific symptoms and signs, which may make it difficult for the healthcare provider to arrive at a definitive diagnosis. In general, GPA is diagnosed through the following tests and medical exams:
- A thorough physical examination and evaluation of one’s complete medical history
- Chest X rays and CT scan of chest and sinuses, which may show cavitations and mass formation
- Blood tests such as complete blood counts (CBC), erythrocyte sedimentation rate (ESR), and kidney function tests
- Urine analysis to detect the presence of blood and proteins in urine
- c-ANCA blood test for the detection of antibodies:
- 95% of cases of Granulomatosis with Polyangiitis are associated with antineutrophil cytoplasmic antibodies (ANCA), which are expressed in a cytoplasmic (c-ANCA) pattern on microscopic examination
- Having a positive blood test for ANCA autoantibodies that are expressed in this specific pattern helps the healthcare providers arrive at an appropriate diagnosis. Having a positive blood test is very helpful in establishing a diagnosis
- A negative blood test for these specific autoantibodies may not indicate that the individual does not have GPA. In such cases, the healthcare provider usually relies on other tests and procedures to arrive at a diagnosis
- Since c-ANCA blood test is positive for 95% of the individuals with Granulomatosis with Polyangiitis, this test is considered to be a sensitive test. c-ANCA blood test is also considered to be a highly specific test for GPA, since reportedly, no other disease yields a positive result with this test
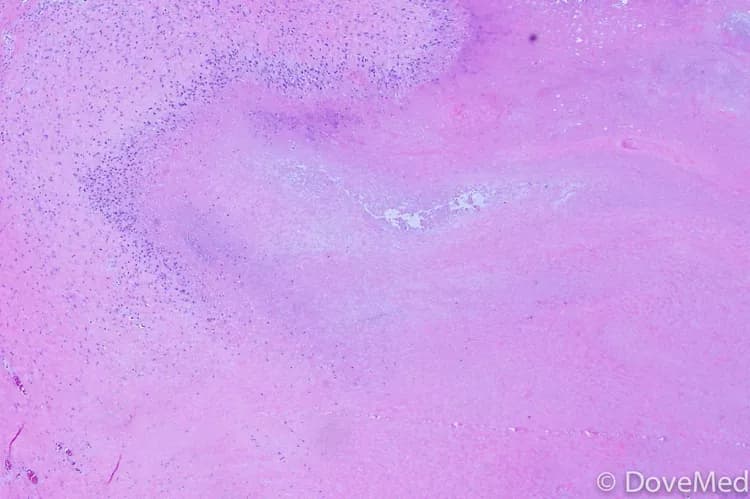
- Biopsy of tissue of the affected region: A tissue biopsy involves the removal of a sample of tissue, such as from the sinuses, skin, lung, or kidney, to check for Granulomatosis with Polyangiitis. The biopsy of the tissue is sent to a laboratory where the pathologist examines the nodule under a microscope to arrive at a definitive diagnosis. The pathologist examination of the tissue biopsy would show characteristic findings of granulomas and abnormal inflammations
Many clinical conditions may have similar signs and symptoms. Your healthcare provider may perform additional tests to rule out other clinical conditions to arrive at a definitive diagnosis.
What are the possible Complications of Granulomatosis with Polyangiitis?
The possible complications of Granulomatosis with Polyangiitis could include:
- Perforation of nasal septum
- Hearing loss due to constant ear infections
- Chronic conjunctivitis
- Kidney failure
- Lung failure
How is Granulomatosis with Polyangiitis Treated?
The treatment of Granulomatosis with Polyangiitis consists of medical and surgical care.
Medical care primarily involves suppressing the immune system using steroids and immunosuppressive medications.
- Bisphosphonate (Fosamax) is given to treat osteoporosis caused by chronic steroid treatment
- Treatment with methotrexate can cause folic acid deficiency, and hence, replacement with folic acid or folinic acid is often considered
- Antibiotics for lung infections and ear infections, as needed
Surgical treatment depends on the signs, symptoms, and complications caused by Granulomatosis with Polyangiitis and may include:
- Nasal septal surgery to correct nasal deformity
- Opening of the tear ducts caused by obstruction of the lacrimal (tear) ducts
- Dilatation of the bronchial airways caused by bronchial stenoses
- Insertion of PE tubes to treat frequent middle ear infections causing eustachian tube dysfunction
- Kidney transplant in cases where inflammation causes severe damage to kidney function
How can Granulomatosis with Polyangiitis be Prevented?
Currently there are no methods to prevent Granulomatosis with Polyangiitis. An early diagnosis and prompt treatment can help decrease the burden of the disease.
What is the Prognosis of Granulomatosis with Polyangiitis? (Outcomes/Resolutions)
The prognosis of Granulomatosis with Polyangiitis depends on the severity of signs and symptoms and the organs affected. It varies from one individual to another.
- The prognosis is good in individuals with mild symptoms and those who respond readily to immunosuppressive treatment
- In individuals with severe symptoms causing damage to the lungs and kidneys, the prognosis can be poor, especially if such individuals do not respond well to immunosuppressive treatment
- Constant monitoring of disease activity with frequent medical follow-up can also help improve the prognosis
- Nevertheless, the prognosis is poor in individuals with untreated disease
Additional and Relevant Useful Information for Granulomatosis with Polyangiitis:
Granulomatosis with Polyangiitis (GPA) was earlier referred to as Wegener's Granulomatosis (WG). The disorder was named after Friedrich Wegener, who in 1936 described the disease. This scientist was associated with the Nazis, and hence, several world academic and professional bodies discourage the usage of his name; instead, it was proposed to replace his name with the more descriptive title “Granulomatosis with Polyangiitis”.
Related Articles
Test Your Knowledge
Asked by users
Related Centers
Related Specialties
Related Physicians
Related Procedures
Related Resources
Join DoveHubs
and connect with fellow professionals

0 Comments
Please log in to post a comment.