What are the other Names for this Condition? (Also known as/Synonyms)
- Carcinoma of Endometrium
- Carcinoma of Uterus
- Endometrial Carcinoma
What is Endometrial Cancer? (Definition/Background Information)
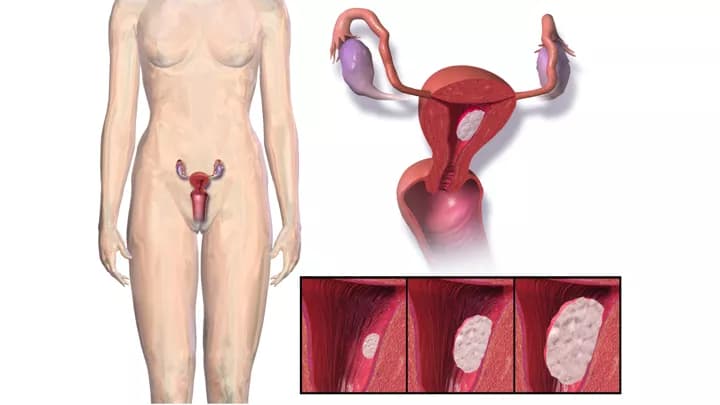
- Cancers of the uterus can arise from various structures of the uterus. Broadly, they may be categorized as the following:
- Carcinoma of the endometrium (arising from the lining of the endometrium)
- Carcinoma arising in the wall of the uterus (called sarcomas)
- Carcinoma arising from the outside covering of the uterus (serosal surface of the uterus): Such cancers arising from the serosal surface are very rare and are called sarcomas
- Endometrial Cancer is a type of cancer that begins in the lining of the uterus (the endometrium). The majority of Endometrial Cancer cases are detected and diagnosed in women aged 50 years and older (80% of the tumors are observed in postmenopausal women)
- According to the World Cancer Research Fund International (WCRF International), Endometrial Cancer is the 6th most commonly diagnosed cancer in women. Also, each year, approximately around 350,000 new cases are diagnosed in women worldwide
- A variety of factors are known to influence the development of the cancer including endometrial hyperplasia, poorly-controlled diabetes, positive family history, and polycystic ovarian syndrome. Obese women have an elevated risk of developing Endometrial Cancer. The exact cause of the cancer is unknown, but it may be due to certain genetic abnormalities
- The majority of Endometrial Cancer cases are detected and diagnosed at an early stage due to frequent abnormal vaginal bleeding, which is a major indicative sign. Additional signs and symptoms may include pelvic pain, pain during sex, and urination difficulties
- If Endometrial Cancer is diagnosed early, then a surgical removal of the uterus (where possible) usually eliminates the cancer. The earlier the stage of cancer at detection and the lower the grade of the cancer, the better is the prognosis
There are many different types of Endometrial Cancer. The type of normal uterus cells that transform to malignancy can help identify the subtype of Endometrial Cancer, which in turn can help determine the appropriate treatment to be provided. Some of the different types include:
- Endometrioid Carcinoma of Endometrium
- Mucinous Carcinoma of Endometrium
- Serous Carcinoma of Endometrium
- Clear Cell Carcinoma of Endometrium
- Neuroendocrine Tumors of Endometrium
- Mixed Carcinomas of Endometrium
- Undifferentiated and Dedifferentiated Carcinomas of the Endometrium
Based on the FIGO grading system, Endometrial Cancer types are histologically graded as the following:
- FIGO 1: Low-grade
- FIGO 2: Low-grade
- FIGO 3: High-grade
[FIGO - International Federation of Gynecology and Obstetrics]
Based on the grading, whether the tumor is influenced by excess estrogen, the type of genetic mutations noted, and other prognostic factors, Endometrial Cancer types are categorized as the following:
- Type 1 Endometrial Cancers:
- Includes endometrioid carcinoma and mucinous carcinoma
- The tumors are low-grade (FIGO 1 and 2)
- These categories of tumors are influenced by excessive estrogen stimulation, tamoxifen use, obesity, polycystic ovary syndrome, and other factors
- The presence of endometrial intraepithelial neoplasm (EIN) or atypical endometrioid hyperplasia is a significant risk factor
- Type 1 tumors are found to have mutations in PTEN, KRAS, and PAX2 genes
- Type 2 Endometrial Cancers:
- Includes serous carcinoma, clear cell carcinoma, carcinosarcoma, and undifferentiated carcinoma
- These are high-grade tumors (FIGO 3) that are aggressive in nature. In most cases at the time of diagnosis, the tumors are found to be in advanced (metastatic) stages
- Unopposed estrogen exposure is less of a risk factor, when compared to type 1 cancers
Who gets Endometrial Cancer? (Age and Sex Distribution)
- Endometrial Cancer is a type of cancer that affects the lining of the uterus (endometrium) in women
- Most of the cases are observed in postmenopausal women aged 50 years and older; over 50% of them are diagnosed between the ages of 50 and 70 years
- Women under the age of 40 years are rarely diagnosed with Endometrial Cancers
- All racial and ethnic groups are affected by this cancer type; the condition is observed worldwide in women. Nevertheless, Caucasians are found to have a higher risk than other races
What are the Risk Factors for Endometrial Cancer? (Predisposing Factors)
The underlying cause of Endometrial Cancer is unknown at this time, although healthcare experts believe that certain factors may increase an individual’s risk for the condition. The risk factors include:
- Advancing age: Endometrial Cancer may generally develop in females of all ages, but are seldom diagnosed in women younger than 40 years. The risk increases as one ages, although most cases occur between the ages 55 and 70 years
- Obesity: Obese women have an elevated risk for developing the condition. Studies indicate that about 40% of the cases are associated with obesity
- Endometrial hyperplasia (specifically endometrial intraepithelial neoplasm or atypical endometrioid hyperplasia): It is an abnormal overgrowth of the endometrium that is usually caused by hormonal effects. Hyperplasia is not a type of cancer; however women with atypical endometrioid hyperplasia have a 45 times greater risk for getting Endometrial Cancer in their lifetime. Atypical endometrioid hyperplasia is also called endometrial intraepithelial neoplasm (EIN), which is considered a premalignant condition
- Poor dietary choices: Individuals taking a diet that consists of foods high in animal fat may have an increased risk for developing this cancer type
- Nulliparous women: Women who have never been pregnant have an increased risk for Endometrial Cancer, than women who have had at least one or more pregnancies
- Tamoxifen therapy: Women, on the hormone therapy drug tamoxifen, to treat or prevent breast cancer may be at an increased risk. Nevertheless, women are advised to discuss the risk and benefits of the therapy with their physician. Many times, the benefits of tamoxifen therapy for breast cancer far outweigh the risk of Endometrial Cancer development
- Estrogen therapy for a long time duration
- Family history: Endometrial Cancer may be prevalent in families, since in 1 in 20 cancer cases, a family history is reported. Individuals with an associated history of colon cancer may be at a significantly higher risk. Individuals with one or more immediate family members or relatives with a history of colon cancer, non-polyposis colorectal cancer (HNPCC) or Lynch syndrome, may have an increased risk for Endometrial Cancer
- Diabetes: Endometrial Cancer is 4 times more likely to develop in women with diabetes. Researchers believe this may be linked to the high obesity rates found in individuals with type II diabetes
- Radiation therapy: Women who had had radiation therapy to the pelvis for other cancers are at an increased risk
- High blood pressure
- History of breast cancer or ovarian cancer
- Polycystic ovarian syndrome (PCOS): Polycystic ovarian syndrome is a condition in which women’s hormones are out of balance. It is one of the most common endocrine disorders in women
- Any other condition causing an hormonal imbalance in the body, such as use of birth-control pills or pregnancy
- Use of intrauterine contraceptive devices (IUDs)
- Menstrual cycle: Women who got their period before the age of 12 years, and those who reached menopause after age 55 years have an elevated risk. The longer the duration between menarche and menopause, the greater is the risk. This is due to hormonal influences during the reproductive period on the endometrial tissue
- Muir-Torre syndrome: A rare genetic disorder that is inherited in an autosomal dominant pattern
- Turner syndrome: A congenital genetic condition that exclusively occurs in females
It is important to note that having a risk factor does not mean that one will get the condition. A risk factor increases ones chances of getting a condition compared to an individual without the risk factors. Some risk factors are more important than others.
Also, not having a risk factor does not mean that an individual will not get the condition. It is always important to discuss the effect of risk factors with your healthcare provider.
What are the Causes of Endometrial Cancer? (Etiology)
The exact cause and mechanism of formation of Endometrial Cancer is unknown. Some researchers believe that the tumor occurs due to a genetic mutation within the cells in the endometrium (the lining of the uterus).
- In general, it is known that cancers form when normal, healthy cells begin transforming into abnormal cells - these cancer cells grow and divide uncontrollably (and lose their ability to die), resulting in the formation of a mass or a tumor
- The transformation of normally healthy cells into cancerous cells may be the result of genetic mutations. Mutations allow the cancer cells to grow and multiply uncontrollably to form new cancer cells
- These tumors can invade nearby tissues and adjoining body organs, and even metastasize and spread to other regions of the body
Currently, medical research is being conducted to determine the exact cause of Endometrial Cancer.
What are the Signs and Symptoms of Endometrial Cancer?
Due to the presence of significant signs and symptoms in the initial periods, Endometrial Cancer is generally diagnosed at an early stage. However, if there are associated underlying conditions presenting overlapping signs and symptoms, there could be a delay in diagnosis.
The signs and symptoms that are typically observed early in Endometrial Cancer include:
- Postmenopausal abnormal vaginal bleeding, spotting, or discharge
- Abnormal bleeding is noted in 65% of the cases
- Vaginal bleeding after menopause occurs in 9 out of 10 women
- Painful and difficulty during urination
- Pain during sexual intercourse
- Abdominal pain (the pain is usually a pelvic pain)
In more advanced cases, the following signs and symptoms may be observed:
- Abdominal swelling due to the mass or due to fluid accumulation in the belly (called ascites)
- Persistent feeling of abdominal bloating with nausea or vomiting
- Changes in bowel movements, such as constipation
- Feeling full soon, after eating less
- Loss of appetite with weight loss
- Fatigue, feeling tired easily
- Frequent urination (polyuria)
How is Endometrial Cancer Diagnosed?
There is a variety of tests healthcare providers may use to detect, locate, and diagnose Endometrial Cancer, and assess if it has potentially spread to other regions. A surgical procedure called a biopsy (usually performed by an obstetrician-gynecologist) is the main test a healthcare provider relies on to make a definitive diagnosis of Endometrial Cancer.
The diagnostic tools may include:
- A thorough physical examination and a complete medical history evaluation is very vital to the diagnosis
- Pelvic examination: During a pelvic examination, a physician exams the uterus, vagina, ovaries, fallopian tubes, bladder, and rectum to check for any abnormal changes in these organs
- Complete blood count (CBC) with differential of white blood cells
- Liver function test (LFT)
- Blood tests called serum tumor markers that include:
- CA-125 test
- Human chorionic gonadotropin (hCG)
- Alpha-fetoprotein (AFP)
- Lactate dehydrogenase (LDH)
- Inhibin (hormone)
- Estrogen and testosterone levels
- Hysteroscopy: During hysteroscopy, a physician inserts a tiny telescope through the cervix into the uterus. This procedure is used to remove small amounts of the endometrium for pathological examination
- Cystoscopy: During cystoscopy, a physician inserts a narrow tube called cystoscope, to look directly into the bladder to see if cancer from endometrium has spread to the bladder. To make an individual more comfortable during this test, a local anesthetic is usually administered
- Proctoscopy: During proctoscopy, a physician inserts a narrow tube called proctoscope, to look directly into the rectum to see if cancer from endometrium has spread to the rectum. To make an individual more comfortable during this test, a general anesthetic is usually administered
- Dilation and curettage (D&C) of the uterus: If the biopsy was inadequate in procuring enough tissue samples, or a physician is unsure whether cancer exists, a procedure called dilation and curettage may be necessary. A D&C of the uterus procedure involves opening the cervix and surgically removing the inner lining and tissue present in the uterus. To make an individual more comfortable during this procedure, a general anesthetic is usually administered
- X-ray of the abdomen and pelvic region
- Chest X-ray: Chest X-rays are used to detect if the cancer has spread to the lung
- Barium enema X-ray
- Computerized tomography (CT) scan of the abdomen and pelvic region: Also known as CAT scan, this radiological procedure creates detailed three-dimensional images of structures inside the body. CT scans are not tools of preference to detect Endometrial Cancer. Although CT scans may be helpful in detecting recurrences, or if the cancer has metastasized to other organs
- MRI scan of abdomen and pelvic region
- Transvaginal ultrasound: Transvaginal ultrasound inserts an ultrasound probe into the vagina designed to take pictures of the insides of the uterus
- Vascular radiological studies of abdomen and pelvic region
- Positron emission tomography (PET scan): A PET scan is a nuclear medicine imaging technique that uses three-dimensional images to show how tissue and organs are functioning. A small amount of radioactive material is required with this test. The radioactive material may be injected into a vein, inhaled, or swallowed. It may be performed to see if the cancer has metastasized/spread to other regions
- Exploratory laparoscopy (diagnostic laparoscopy): This is a procedure wherein the abdomen is examined using a minimally invasive technique. During this procedure, a tissue biopsy and tissue for culture are performed. A minimally invasive approach helps decrease the complications and length of stay at the hospital. A diagnostic laparoscopy is also helpful in establishing the staging of the tumor
- Colonoscopy: A colonoscopy may be performed to assess the extent of tumor spread
- Whole body bone scan
- Endometrial biopsy: A biopsy refers to a medical procedure that involves the removal of cells or tissues, which are then examined by a pathologist under a microscope. After putting together the clinical findings, special studies on tissues (if needed), and the microscope findings, the pathologist arrives at a definitive diagnosis. Sometimes, the pathologist may perform special studies that may include immunohistochemical stains, histochemical stains, molecular testing, and very rarely, electron microscopic studies. Examination of the biopsy under a microscope by a pathologist is considered to be the gold standard in arriving at a conclusive diagnosis
Note: Pap smear is not a good screening tool for Endometrial Cancer. Approximately 50% of women with Endometrial Cancer have normal Pap smear.
Many clinical conditions may have similar signs and symptoms. Your healthcare provider may perform additional tests to rule out other clinical conditions to arrive at a definitive diagnosis.
What are the possible Complications of Endometrial Cancer?
The complications of Endometrial Cancer include:
- Emotional distress due to the presence of uterine cancer
- Poorly-differentiated carcinomas may be associated with paraneoplastic syndrome, which may affect the functioning of the eye. In this condition, an individual may have significant vision changes including blindness due to bilateral melanocytic growth of the uvea of the eye
- If detected late, Endometrial Cancer can spread into the surrounding organs, making it difficult to successfully treat using surgical interventions
- The cancer can metastasize (spread) to the fallopian tube, ovary, cervix, bone, liver, lung, and brain. If metastasis to the lymph nodes are noted, then usually it is to the pelvic and para-aortic lymph nodes
- Perforation in the uterus, which may occur during a diagnostic D&C or endometrial biopsy procedure
- Sexual dysfunction can take place as a side effect of surgery, chemotherapy, or radiation therapy
- Recurrence of the cancer following incomplete surgical removal
How is Endometrial Cancer Treated?
The treatment of Endometrial Cancer may depend upon a consideration of the following set of factors:
- The histological subtype of the cancer
- Stage of the cancer: Once a diagnosis of cancer of the endometrium has been made, the extent to which the tumor has spread is assessed. This is called staging
- Size and location of the tumor
- Severity of the signs and symptoms
- Age of the individual
- Overall health status of the individual
- The treatment preferences of the individual
Following is the staging protocol for Endometrial Cancer, according to the American Joint Committee on Cancer (AJCC), updated July 2016:
Stage I Endometrial Cancer: The cancer is found in the uterus only. Stage I is divided into stages IA and IB, based on how far the cancer has spread.
- Stage IA: The cancer is in the endometrium only or less than halfway through the myometrium (muscle layer of the uterus)
- Stage IB: The cancer has spread halfway or more into the myometrium
Stage II Endometrial Cancer: The cancer has spread into connective tissue of the cervix, but has not spread outside the uterus.
Stage III Endometrial Cancer: The cancer has spread beyond the uterus and cervix, but has not spread beyond the pelvis. Stage III is divided into stages IIIA, IIIB, and IIIC, based on how far the cancer has spread within the pelvis.
- Stage IIIA: The cancer has spread to the outer layer of the uterus and/or to the fallopian tubes, ovaries, and ligaments of the uterus
- Stage IIIB: The cancer has spread to the vagina and/or to the parametrium (connective tissue and fat around the uterus)
- Stage IIIC: The cancer has spread to lymph nodes in the pelvis and/or around the aorta (largest artery in the body, which carries blood away from the heart)
Stage IV Endometrial Cancer: The cancer has spread beyond the pelvis. Stage IV is divided into stages IVA and IVB, based on how far the cancer has spread.
- Stage IVA: The cancer has spread to the bladder and/or bowel wall
- Stage IVB: The cancer has spread to other parts of the body beyond the pelvis, including the abdomen and/or lymph nodes in the groin
(Source: Stages of Endometrial Cancer, July 2016, provided by the National Cancer Institute at the National Institutes of Health; U.S. Department of Health and Human Services)
In most cases, a combination of chemotherapy (drugs), radiation therapy, and surgical procedures is employed by the healthcare provider to treat the condition.
Surgery for Endometrial Cancer: The recommended treatment for women with the cancer is to have the uterus surgically removed. The surgical treatment options a healthcare provider may recommend include:
- Hysterectomy: In this procedure, the uterus and cervix are removed. This is done by making an incision on the abdomen (termed abdominal hysterectomy), or through the vagina (termed vaginal hysterectomy), or by using a laparoscope (termed laparoscopic hysterectomy). Surgery is performed under general or epidural anesthesia, though the ability to have children is lost. Complications, such as bleeding, infection, or damage to the urinary tract, or the intestinal system, may occur in rare cases
- Radical hysterectomy: The uterus, cervix, the upper part of the vagina and tissues, next to the uterus are removed. Additionally, some pelvic lymph nodes may also be surgically taken out. The surgery is performed under anesthesia and may be carried out, via an incision made on the abdomen or by using laparoscopy. With this invasive procedure, the ability to have children is lost. Rarely, complications such as bleeding, infection, or damage to the urinary tract or the intestinal system, may occur. Removal of lymph nodes may lead to swelling of legs (lymphedema)
- Hysterectomy (abdominal) with salpingo-oophorectomy: It is a surgical procedure involving the removal of the uterus, and of the fallopian tube and ovary (salpingo-oophorectomy)
- Pelvic exenteration: The uterus, tissues surrounding the uterus, cervix, pelvic lymph nodes, and the upper part of the vagina, are removed. In addition, depending on the tumor spread, the remainder of the vagina, the bladder, rectum, and a part of the colon, may also be removed. Recovery from this surgery may take a long period of time
- A debulking surgery to reduce the tumor mass, followed by a combination of chemotherapy and radiation therapy may be employed in some instances. The debulking procedure helps the chemotherapy treatment in being more effective, because there is lesser tumor mass left for the drugs to act on. Chemotherapy may be administered before debulking or after debulking procedure, depending on each individual’s specific circumstances
During surgery, the surgeon will also examine the surrounding areas of the uterus looking for signs to see if the cancer has metastasized (spread) locally. After surgical treatment, the attending healthcare provider will discuss the details of the cancer with the individual.
Chemotherapy for Endometrial Cancer:
- Chemotherapy is a treatment that uses drugs to kill cancer cells. In this treatment, combinations of two or more chemotherapy drugs are usually used
- These drugs may be administered intravenously (through a vein in the arm), or orally (in a pill-form). Drugs inserted into the bloodstream traveling through the body and kill cancer cells
- Such drugs may be recommended for individuals with advanced Endometrial Cancer that has spread to other body parts
Radiation therapy for Endometrial Cancer:
- Radiation therapy attempts to destroy cancer cells by aiming high-energy beams at the cancer cells
- Radiation therapy can either be administered by a machine outside the body (external beam radiation) or administered internally, by a device positioned directly at, or close to the malignant tumor, inside the vagina (a procedure known as brachytherapy)
- Radiation therapy may be used before surgery to decrease the size of a tumor, thus allowing for easy removal, or after surgery to kill any remaining cancer cells
Radiation therapy and chemotherapy are sometimes used as a combination tool.
Hormone therapy: Hormonal therapy is a medical treatment used for women with advanced Endometrial Cancer that has metastasized beyond the uterus. The treatment options include taking medications that affect the hormone levels in the body:
- Synthetic progestin: Synthetic progestin, a type of hormone progesterone, may help prevent the development and progression of Endometrial Cancer cells
- Luteinizing hormone (LH): Also called lutropin, this hormone therapy drug helps lower an individual’s estrogen level in the body, or decrease the body’s ability to use the available estrogen. Endometrial Cancer cells rely on estrogen (the primary female sex hormone) to proliferate, and thus, administering LH drugs may cause the cancer cells to die out
How can Endometrial Cancer be Prevented?
Currently, there are no known and available methods to prevent Endometrial Cancer. However, various steps may be taken to help decrease the incidence risk:
- Physical activity: Obesity increases the risk for cancer due to additional related risk factors, such as increased estrogen level, polycystic ovary syndrome, reduced physical activity, and a diet high in saturated fats. Therefore, individuals with higher physical activity levels have a decreased risk of developing Endometrial Cancer
- Pregnancy and breastfeeding: During pregnancy and while breastfeeding, the estrogen levels are lowered. Being pregnant and/or breastfeeding may lower a woman’s risk for Endometrial Cancer. Women, who have multiple pregnancies in their lifetime, and who breastfeed for a period greater than 18 months, may have a decreased risk
- Combination of oral contraceptives: Taking a combination of oral contraceptives, such as estrogen and progestin, decrease the risk for Endometrial Cancer. The protective effect of a combination of oral contraceptives increases, the longer they are taken; it may even last several years after usage is stopped
- Adequate consumption of fruits and vegetables: A healthy diet, low in saturated fats and rich in many fruits and vegetables, may help decrease one’s risk for Endometrial Cancer. Regular consumption of soy-based foods, incorporated into a diet, also decreases one’s risk
- Individuals with Lynch syndrome should have regular/annual check-ups (as recommended by the healthcare provider)
- The US Preventive Services Task Force (USPSTF) currently does not have any recommendation for screening against Endometrial Cancer for the general population. Tests, such as trans-vaginal ultrasonography and Pap smears, are not really useful as screening tools
- The US-based National Cancer Institute (NCI) recommends that women, who are at high risk for Cancers of the Endometrium, take regular (annual) examinations
- Early diagnosis with close monitoring and treatment of the tumor is important. A timely tumor recognition and prompt treatment will help in having optimal outcomes
Regular medical screening at periodic intervals with blood tests, radiological scans, and physical examinations are mandatory, due to risk of metastasis and recurrence of the tumor, for individuals who have already endured the cancer. Often several years of active vigilance is necessary.
What is the Prognosis of Endometrial Cancer? (Outcomes/Resolutions)
- The prognosis for Endometrial Cancer depends upon a set of several factors that include:
- The size of the tumor: Individuals with small-sized tumors fare better than those with large-sized tumors
- Stage of cancer: With lower-stage tumors, when the tumor is confined to site of origin, the prognosis is usually excellent with appropriate therapy. In higher-stage tumors, such as tumors with metastasis, the prognosis is poor
- Histological subtype of the tumor
- FIGO grade of the tumor: Tumors that are graded 1 and 2 have better prognoses than grade 3 tumors
- Hormone-receptor status of the cancer such as estrogen receptor (ER) and progesterone receptor (PR)
- Cell growth rate of the Endometrial Carcinoma
- Menopausal status of the women
- Overall health of the individual: Individuals with overall excellent health have better prognosis compared with those with poor health
- Age of the individual: Older individuals generally have poorer prognosis than younger individuals
- Individuals with bulky disease have a poorer prognosis
- Involvement of the regional lymph nodes, which can adversely affect the prognosis
- Involvement of vital organs may complicate the condition
- The surgical respectability of the tumor (meaning, if the tumor can be removed completely)
- Whether the tumor is occurring for the first time, or is a recurrent tumor. Recurring tumors have worse prognosis compared to tumors that do not recur
- Response to treatment: Tumors that respond to treatment have better prognosis compared to tumors that do not respond to treatment
- Progression of the condition makes the outcome worse
- Women with Endometrial Cancer have a survival rate of approximately 92% after 1 year, and 95% at 5 years, if the cancer has not spread. However, if the cancer has metastasized (spread), the survival rate at 5 years is only 23%
- In general, cancers included in type 1 group have better prognosis than those in type 2 group. Thus, endometrioid carcinoma and mucinous carcinoma have better outcomes than serous carcinoma, clear cell carcinoma, carcinosarcoma, and undifferentiated carcinoma; when the comparisons are made on a same stage basis
- An early diagnosis and prompt treatment of the tumor generally yields better outcomes than a late diagnosis and delayed treatment
- The combination chemotherapy drugs used, may have some severe side effects (like cardio-toxicity). This chiefly impacts the elderly adults, or those who are already affected by other medical conditions. Individuals, who tolerate chemotherapy sessions better, generally have better outcomes
Additional and Relevant Useful Information for Endometrial Cancer:
- Cervical cancer is a malignancy of the cervix, which is the lower part of the uterus/womb. It is the 2nd or 3rd most common cancer in women worldwide. A vast majority of cancers arising from the cervix (almost 70 %) are squamous cell carcinomas
The following link can help you understand squamous cell carcinoma of uterine cervix:
Related Articles
Test Your Knowledge
Asked by users
Related Centers
Related Specialties
Related Physicians
Related Procedures
Related Resources
Join DoveHubs
and connect with fellow professionals

0 Comments
Please log in to post a comment.