Congenital Hydrocephalus
What are the other Names for this Condition? (Also known as/Synonyms)
- Fetal Cerebral Ventriculomegaly
- Fetal Hydrocephalus
- Primary Hydrocephalus
What is Congenital Hydrocephalus? (Definition/Background Information)
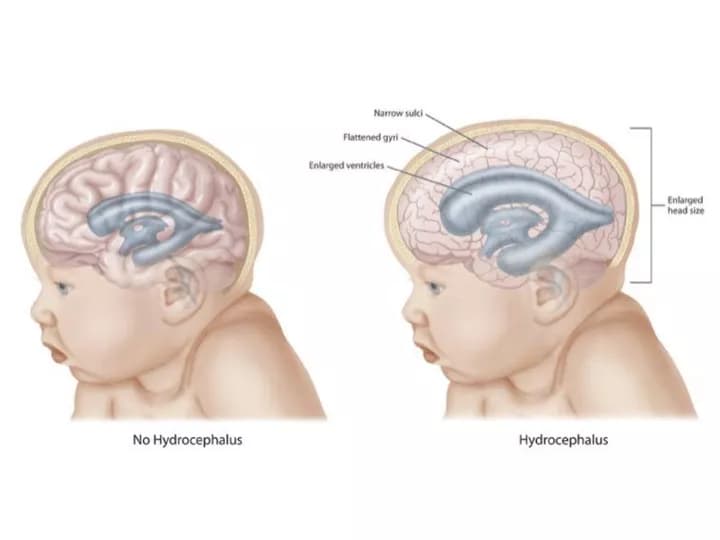
- Hydrocephalus is a buildup of excess fluid in the brain. There are 2 types of hydrocephalus:
- Acquired Hydrocephalous
- Congenital Hydrocephalous
- Congenital Hydrocephalus is a birth defect, caused either by genetic defects, or fetal growth and development anomalies
- The uncharacteristic buildup of cerebrospinal fluid (CSF) in the brain may injure the organ, resulting in physical and mental abnormalities. Early detection and treatment is vital to prevent adverse effects of this abnormality
- The prognosis is dependent on a variety of factors; however, one of the key factor that determines the outcome is the cause of Congenital Hydrocephalus
Who gets Congenital Hydrocephalus? (Age and Sex Distribution)
- Newborn babies are present with Congenital Hydrocephalus that is distinctly visible as an enlarged head. The incident rate of this disorder is about 1 in 1000 live births
- Generally, both male and female sexes are equally prone to the condition, with the exception of Bickers-Adam syndrome (where only male babies are affected by this congenital syndrome)
- Information on racial or ethnic preference (if any) is unavailable
What are the Risk Factors for Congenital Hydrocephalus? (Predisposing Factors)
Risk factors of Congenital Hydrocephalus include:
- Excess production of cerebrospinal fluid (CSF), or inability of the brain to absorb sufficient CSF
- Any obstruction to the free flow of CSF within the central spinal cord
- Brain hemorrhages, brain tumors or cysts
- Any infection that affects the brain, neural tube disorders (spina bifida), brain malformations (such as Arnold-Chiari malformation Type II, Dandy-Walker syndrome)
- A neurological defect, called aqueduct atresia and stenosis, is one of the most common causative factor for Congenital Hydrocephalus
- Infections, such as syphilis and toxoplasmosis, borne by the mother
- Genetic defects due to chromosomal aberrations, like Trisomy syndromes
- Preterm delivery
It is important to note that having a risk factor does not mean that one will get the condition. A risk factor increases ones chances of getting a condition compared to an individual without the risk factors. Some risk factors are more important than others.
Also, not having a risk factor does not mean that an individual will not get the condition. It is always important to discuss the effect of risk factors with your healthcare provider.
What are the Causes of Congenital Hydrocephalus? (Etiology)
- The cerebrospinal fluid has an important role to play in effective functioning of the brain. It regulates the flow of blood within the brain and also acts as a protective buffer around the brain, by absorbing any external force or shock, and by providing an immunological barrier against disease or any infection
- Hydrocephalus occurs, when there is an excess of CSF in the brain cavities, which cannot be drained or absorbed. This builds up pressure in the head to disproportionate levels, and has a potential of causing serious long-term harm, including death
- Any trauma, disease, or infection, affecting the brain can bring about Congenital Hydrocephalus. A congenital manifestation of Hydrocephalus indicates that the causal factor has an origin in the womb, or it followed immediately upon the baby’s birth
- Hydrocephalus in Newborns could be a result of a blocked cerebral aqueduct (a long, narrow midbrain canal), due to a tumor or cyst formation, a hemorrhage, or an infection
- It could also be due to medical disorders, such as craniosynostosis, malformations of brain (Arnold-Chiari malformation Type II, Dandy-Walker syndrome), neural tube defects, and hydranencephaly, among others
What are the Signs and Symptoms of Congenital Hydrocephalus?
The signs and symptoms of Congenital Hydrocephalus differ for infants and older children. The skull is not yet completely hardened at infancy, and the disorder may be in its initial phase of progression.
In infants, the signs and symptoms of Congenital Hydrocephalus include:
- Lethargy, sleepiness
- Irritability
- Seizures
- Drooping, downward deviating eyes, termed as ‘sunsetting’
- Feeding troubles, frequent vomiting
- Developmental delays
- Infants usually have a large head (considering the body proportion)
In children, the signs and symptoms of Congenital Hydrocephalus include:
- Lethargy, sleepiness, drowsiness
- Irritability, headaches
- Blurred vision, swollen optic nerve, ‘sunsetting’ of the eyes
- Vomiting and nausea
- Unsteady walking posture, loss of balance
- Dementia, memory loss, cognition and coordination problems, speech impairment
- Seizures
- Urinary incontinence
How is Congenital Hydrocephalus Diagnosed?
Both prenatal and postnatal tests are available to diagnose Congenital Hydrocephalus. The main diagnostic tools include:
- Amniocentesis - performed at around the 5th month of pregnancy
- Ultrasound scans - to check for any abnormal fluid levels in the brain, while baby is in the womb
- After birth of the child, the imaging studies performed could include: MRI scan of central nervous system (brain and spine), CT scan of the head and neck, pressure tests to detect pressure of CSF in the brain
Since treatment of the condition can commence only after birth of the child; the above test results are correlated with a comprehensive physical (neurological) and family medical history evaluation.
Many clinical conditions may have similar signs and symptoms. Your healthcare provider may perform additional tests to rule out other clinical conditions to arrive at a definitive diagnosis.
What are the possible Complications of Congenital Hydrocephalus?
Complications due to Congenital Hydrocephalus may include the following:
- Severe types of Congenital Hydrocephalus can pose a serious threat to normal physical and mental growth of the baby
- Many diseases and conditions could cause fluid pressure buildup in the brain. The presence of these conditions could create additional medical complications
- In treating hydrocephalus, a shunt system is surgically inserted into the skull. This may cause infection, bleeding, obstruction, over-drainage, or the device itself may fail. In many cases, multiple shunt systems may be required to treat the condition, due to repeat malfunctions
How is Congenital Hydrocephalus Treated?
Following are the treatment measures for Congenital Hydrocephalus:
Very mild cases of fluid in the head may be treated with medications. However, surgical interventions are required to drain excess fluid, relieve the pressure buildup, and treat Congenital Hydrocephalus in most cases. In moderate to severe cases of hydrocephalus, the surgery is performed as early as the baby is ‘medically fit’ to undergo the procedure.
There are two main invasive procedures - the shunt system placement and the endoscopic third ventriculostomy (ETV) procedure.
Shunt system placement:
- A mechanical device consisting of a valve and two catheters (small, flexible tubes), known as a shunt, is normally used to treat hydrocephalus. This is the standard and most preferred option used
- One tube is surgically inserted into the head, the valve is placed around the ear, and any excess CSF is drained from the brain, by directing the other tube beneath the skin, usually into the stomach (sometimes into the lung or heart)
- The shunt is left in place, until the condition has improved and the baby is discharged
- Instructions are provided to the parents, on how to take care of the child at home
Endoscopic third ventriculostomy (ETV) placement:
- A tiny hole is surgically made in the wall of the brain cavity. Using endoscopes, the CSF is routed to another location of the body, for it to be reabsorbed
- The rerouting bypasses the obstruction causing the fluid buildup in the brain (such as a tumor, hemorrhage, or cyst)
- ETV helps in normalizing the pressure by avoiding a shunt system - it is an alternative treatment choice, but this method has to be compatible with the child’s medical condition
How can Congenital Hydrocephalus be Prevented?
- There are many causes for Congenital Hydrocephalus; however, the condition is not preventable
- Genetic counseling with genetic testing should be considered by individuals having a family history of the condition, and planning for a child
What is the Prognosis of Congenital Hydrocephalus? (Outcomes/Resolutions)
The prognosis for a child with Congenital Hydrocephalus is based on a combination of many factors. These include:
- Degree of severity of hydrocephalus
- Causative factor of the condition
- Age of the infant or child
- Health and medical history of the individual
- Tolerance level of the child, when subjected to various procedures and medications
- Success of the surgical procedures performed
- Complications that may develop, if any, due to Congenital Hydrocephalus
In some cases, life-long management of the condition is necessary, since the brain and other vital organs may be permanently affected; abnormal developments (both physical and mental) could also occur. An early detection and aggressive treatment of hydrocephalus, with regular follow-up health checkups is essential, in all cases.
Additional and Relevant Useful Information for Congenital Hydrocephalus:
- Acquired Hydrocephalus is the abnormal buildup of cerebrospinal fluid (CSF) inside several cavities of the brain. This is caused either by certain developmental irregularities and disorders, or due to injuries to the head or brain
- The success rate of a first time shunt is around 1 in 3. Most patients would require multiple shunts to manage their condition
- Those living in geographical locations with limited access to healthcare, due to economic hardships cannot afford the high cost of a shunt system placement procedure. As a result, hydrocephalus mortality rates in such regions are significantly much higher
Related Articles
Test Your Knowledge
Asked by users
Related Centers
Related Specialties
Related Physicians
Related Procedures
Related Resources
Join DoveHubs
and connect with fellow professionals

0 Comments
Please log in to post a comment.