What are the other Names for this Condition? (Also known as/Synonyms)
- OCCA (Ovarian Clear Cell Adenocarcinoma)
- Ovarian Clear Cell Adenocarcinoma (OCCA)
What is Clear Cell Adenocarcinoma of Ovary? (Definition/Background Information)
- Clear Cell Adenocarcinoma of Ovary is a rare malignant ovarian tumor that generally affects middle-aged women. The causal factors for Clear Cell Adenocarcinoma of Ovary are unknown
- Tumors of the ovaries can be benign, borderline or low malignant potential (LMP), or malignant tumors. Thus, not all ovarian tumors are cancers
- Benign tumors are not cancerous and do not spread or metastasize. Borderline or low malignant potential (LMP) tumors are usually benign, but some of them can behave like cancers. Malignant tumors are cancers that spread and metastasize
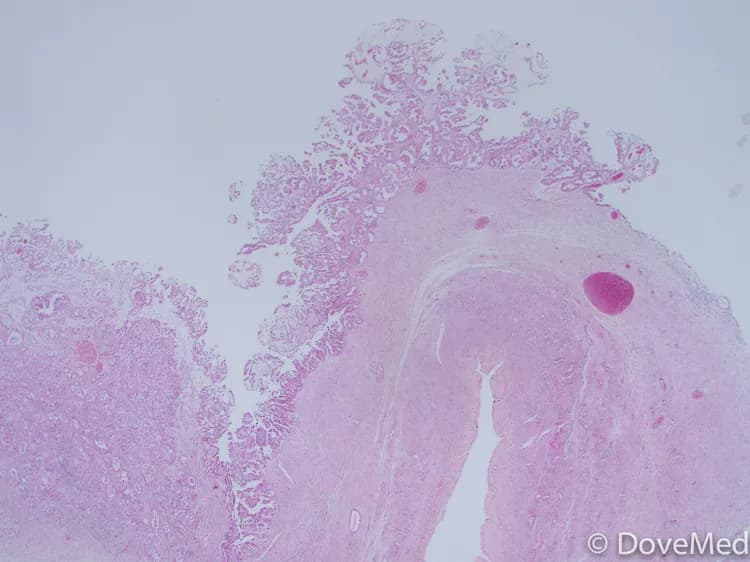
- Clear Cell Adenocarcinoma of Ovary is a rapidly-growing tumor that arises from the epithelial cells in the ovary and occurs as a combination of cyst and solid mass within the ovary
- In a majority of the cases, the tumor presents as a single mass within the ovary. These tumors are associated with endometriosis of ovary and pelvis
- Ovarian Clear Cell Adenocarcinomas (OCCAs) are usually present with signs and symptoms, such as abdominal pain with movement, vaginal bleeding, and increased abdominal girth
- The treatment for Clear Cell Adenocarcinoma of Ovary may involve chemotherapy, surgery, radiation therapy, or a combination of these procedures. The prognosis depends on many factors that include the stage of the tumor
- The prognosis of Ovarian Clear Cell Adenocarcinoma is typically poor despite the provision of appropriate treatment, especially if it has spread to other parts of the body (termed metastatic clear cell adenocarcinoma)
Who gets Clear Cell Adenocarcinoma of Ovary? (Age and Sex Distribution)
- Ovarian Clear Cell Adenocarcinoma is generally observed in middle-aged women with the average age of individual affected being 57 years. Infants and young children are commonly not affected
- Though such ovarian tumors do not usually run within families, rare cases have been reported of such instances
- Worldwide, women of any race and ethnicity may be affected by Clear Cell Adenocarcinoma of Ovary
What are the Risk Factors for Clear Cell Adenocarcinoma of Ovary? (Predisposing Factors)
In general, the risks for ovarian cancers include the following factors. Some individuals may have multiple risk factors, which increases the threat for Clear Cell Adenocarcinoma of Ovary.
- Increasing age: A majority of women who are diagnosed with ovarian cancer are over the age of 55 years
- Body weight: Women who are overweight have an increased risk of developing ovarian cancer
- Genetic mutations: Women with BRCA-1 and BRCA-2 genetic mutations are at increased risk
Note: Studies have found that currently two mutations in the BRCA-1 and BRCA-2 genes can increase the risk. Breast cancer gene 1 (BRCA-1) and breast cancer gene 2 (BRCA-2) are inherited types of mutations. Women with BRCA-1 mutation have a 50% higher risk and women with BRCA-2 mutation have a 20% higher risk of ovarian cancer. However, it is important to note that a majority of women who get Clear Cell Adenocarcinoma of Ovary do not have either the BRCA-1 or the BRCA-2 gene mutations. Also, the presence of these mutations does not mean that the individual will develop the condition.
- Hormone replacement therapy (HRT) in post-menopausal women increases the risk for ovarian cancer
- Family history: Women with a family history of ovarian cancer may have an increased risk
- Past history of breast cancer, colorectal cancer, or endometrial cancer: Having a past diagnosis of these cancers increase the risk of developing ovarian cancer
- Smoking: Some studies have shown that long-standing smoking can increase the risk
- A weakened immune system (immunocompromised) increases the risk of Clear Cell Adenocarcinoma of Ovary
- High fat diet may increase the risk, though this factor has not been conclusively proven
- Childbearing status: Studies have found that women who have had at least one child before the age of 30, have a lowered risk of ovarian cancer
- Breastfeeding status: It has been found that women who breastfeed are at a reduced risk
It is important to note that having a risk factor does not mean that one will get the condition. A risk factor increases ones chances of getting a condition compared to an individual without the risk factors. Some risk factors are more important than others.
Also, not having a risk factor does not mean that an individual will not get the condition. It is always important to discuss the effect of risk factors with your healthcare provider.
What are the Causes of Clear Cell Adenocarcinoma of Ovary? (Etiology)
The cause of Clear Cell Adenocarcinoma of Ovary is unknown in many cases. In some cases, genetic defects may play a role.
What are the Signs and Symptoms of Clear Cell Adenocarcinoma of Ovary?
The signs and symptoms of Clear Cell Adenocarcinoma of Ovary depend on a number of factors such as:
- Size of the tumor
- Histological type of the tumor
- Whether a single ovary or both the ovaries are involved
- The tumor is a cyst or a solid mass
- Whether the tumor produces hormones
- Local spread of the tumor
- Rupture of the cystic mass
- Extent of bleeding within the tumor
- Whether the tumor is present as part of a syndrome, in which case, the signs and symptoms associated with the accompanying syndrome may exist
The presentations are based on the stage of the tumor. Many of the following symptoms can be seen in benign ovarian tumors too. Hence, additional test are always needed before confirming a diagnosis of ovarian cancer.
- Abdominal pain (the pain is usually a pelvic pain)
- Abdominal swelling due to the mass or due to fluid accumulation in the belly (called ascites)
- Increased abdominal girth due to fluid accumulation (ascites)
- Persistent feeling of abdominal bloating with nausea or vomiting
- Changes in bowel movements, such as constipation
- Feeling full soon after eating less (having a feeling of satiety after eating less)
- Loss of appetite with weight loss
- Fatigue, feeling tired easily
- Frequent urination (polyuria) and difficulty while urinating
- Frequent pain during sex (dyspareunia)
- Abnormal menstrual bleeding
Some of the other features of Ovarian Clear Cell Adenocarcinomas include:
- Clear Cell Adenocarcinoma usually presents as a single mass in the ovary, though rarely it can occur as multiple nodules within the same ovary too
- Sometimes, the tumors have been observed to be present at birth
- The ovarian mass is usually not painful and is poorly defined
- These tumors can cause para-endocrine hypercalcemia (a disorder occurring due to ovarian mass)
- The nodule is typically less than 15 cm in size (along the larger dimension); however, some may grow to greater sizes
- Large tumors may occasionally rupture spilling cyst contents into the belly
- These tumors can be locally aggressive, meaning that the tumor may spread to local areas
The Clear Cell Adenocarcinoma of Ovary may occur as a new growth that develops over weeks and months.
How is Clear Cell Adenocarcinoma of Ovary Diagnosed?
The following are the diagnostic tools for Clear Cell Adenocarcinoma of Ovary:
- A thorough physical examination and a complete medical history evaluation is very vital
- Pelvic examination
- Complete blood count (CBC) with differential of white blood cells
- Liver function test (LFT)
- Since these tumors can cause para-endocrine hypercalcemia, a blood analysis would show increased calcium levels
- Blood tests called serum tumor markers that include:
- CA-125 test
- Human chorionic gonadotropin (HCG)
- Alpha-fetoprotein (AFP)
- Lactate dehydrogenase (LDH)
- Inhibin (hormone)
- Estrogen levels
- Testosterone levels
- Exploratory laparoscopy (diagnostic laparoscopy): This is a procedure wherein the abdomen is examined using a minimally invasive technique. During this procedure, a tissue biopsy and tissue for culture are performed. A minimally invasive approach helps decrease the complications and length of stay at the hospital. A diagnostic laparoscopy is also helpful in the staging of the tumor
- Colonoscopy: A colonoscopy may be performed to assess the extent of tumor spread
- A tissue biopsy of the tumor: A tissue biopsy is performed and sent to a laboratory for a pathological examination
A pathologist examines the biopsy under a microscope. After putting together the clinical findings, special studies on tissues (if needed), and the microscope findings, the pathologist arrives at a definitive diagnosis. Sometimes, the pathologist may perform special studies that may include immunohistochemical stains, histochemical stains, molecular testing, and very rarely, electron microscopic studies. Examination of the biopsy under a microscope by a pathologist is considered to be the gold standard in arriving at a conclusive diagnosis.
A differential diagnosis is often undertaken to eliminate other tumor types, before arriving at a definitive diagnosis.
Radiological imaging studies may include:
- X-ray of the abdomen and pelvic region
- Barium enema x-ray
- CT scan of the abdomen and pelvic region
- MRI scan of abdomen and pelvic region
- Ultrasound scans of the pelvic region; usually transvaginal ultrasonography (TVS) and abdominal ultrasound scans are performed
- Vascular radiological studies of abdomen and pelvic region
If the tumor has metastasized to other regions, then radiological examination to determine the extent of metastasis may be performed. These may include:
- X-ray of the affected region
- Barium enema X-ray
- CT scan of the affected region
- MRI scan of the affected region
- Ultrasound scans of the affected region
- Vascular radiological studies of the affected region
- Whole body bone scan
- Positron emission tomography (PET) scan or PET/CT scan
Many clinical conditions may have similar signs and symptoms. Your healthcare provider may perform additional tests to rule out other clinical conditions to arrive at a definitive diagnosis.
What are the possible Complications of Clear Cell Adenocarcinoma of Ovary?
The complications due to Clear Cell Adenocarcinoma of Ovary may include:
- There may be a rapid growth of the tumor which may invade into the surrounding tissues causing tissue damage. A distance metastasis of the tumor from its primary site has been frequently reported
- Recurrence of the ovarian tumor after surgery
- There may be side effects from the chemotherapy (such as toxicity) and radiation therapy administered
A Clear Cell Adenocarcinoma of Ovary can metastasize to other regions of the body. Extensive metastasis may result in fatalities.
How is Clear Cell Adenocarcinoma of Ovary Treated?
The treatment for Clear Cell Adenocarcinoma of Ovary may include any of the following - chemotherapy, surgery, or radiation therapy. In most cases, a combination of chemotherapy (drugs), radiation therapy, and surgical procedures is employed by the healthcare provider to treat the condition.
- The surgery may involve a total abdominal hysterectomy (complete removal of the uterus), removal of both the ovaries and fallopian tubes (called bilateral salpingo-oophorectomy, omentectomy (removal of fat around the intestines), biopsy of lymph nodes within the abdomen, or the removal of other tissues in the pelvis and abdomen as needed
- If the tumor is present in only one ovary, then the surgeon may perform a procedure called unilateral salpingo-oophorectomy. In this procedure only the affected ovary and fallopian tube are removed; the uterus is not removed (there is no hysterectomy performed). The unaffected ovary and fallopian tube is also not removed
- Post-operative care is important: A minimal physical activity is advised, until the surgical wound heals
- A debulking surgery to reduce the tumor mass, followed by a combination of chemotherapy and radiation therapy may be employed in some instances. The debulking procedure helps the chemotherapy treatment in being more effective, because there is lesser tumor mass left for the drugs to act on
- Chemotherapy may be administered before debulking or after debulking procedure, depending on each individual’s circumstances
- Follow-up care with regular screening and check-ups are important (to monitor the status of the tumor)
The healthcare provider will determine and plan the best course of treatment on a case-by-case basis.
How can Clear Cell Adenocarcinoma of Ovary be Prevented?
The cause of Ovarian Clear Cell Adenocarcinoma is unknown. Hence, there are no known methods to prevent the tumor occurrence.
- Early diagnosis with close monitoring and treatment of the tumor is important. A timely tumor recognition and prompt treatment will help in having optimal outcomes
- Due to its metastasizing potential and chances of recurrence, regular medical screening at periodic intervals with blood tests, radiological scans, and physical examinations are often needed
- The US Preventive Services Task Force (USPSTF) currently does not have any recommendation for screening against ovarian cancer for the general population. Tests such as blood serum CA125 level or trans-vaginal ultrasonography are not really helpful as screening tools
- The National Cancer Institute (NCI) recommends that women who are at high risk for ovarian cancer take regular (annual) examinations. The healthcare provider may perform studies such as ultrasonography examinations and CA125 testing as part of one’s annual physical examination
What is the Prognosis of Clear Cell Adenocarcinoma of Ovary? (Outcomes/Resolutions)
The prognosis of Clear Cell Adenocarcinoma of Ovary depends upon the following factors:
- The stage of the tumor
- Overall health of the individual
- Tumor stage at detection
- Presence of metastasis and the organs involved with metastasis
- The patient’s response to treatment such as chemotherapy and radiotherapy
At the time of diagnosis, women with Clear Cell Adenocarcinoma of Ovary have shown different stages of the tumor. Statistics reveal that 33% are diagnosed at Stage I, 19% at Stage II, 29% at Stage III, and 9% at Stage IV. The 5-year survival rate depends on the tumor stage at the time of diagnosis. After 5 years, it is 69% for Stage I tumors, 55% for Stage II, 14% for Stage III, and 4% for Stage IV tumors.
The ovarian cancer is staged as follows:
Stage I ovarian cancer: In Stage I ovarian cancer, the cancer is limited to one or both ovaries. Stage I is broken into three separate subcategories:
- IA: Cancer is confined to one ovary; no cancer cells are present on the surface of the ovary, or in the pelvis or abdomen
- IB: Cancer is present in both ovaries, but no cancer cells are present on the surface of the ovaries, or in the pelvis or abdomen
- IC: Cancer is present in one or both the ovaries. Additionally, the cancer cells are present on the surfaces of one or both ovaries, one tumor has ruptured, or the cancer cells are found in fluid samples from the abdomen
Stage II ovarian cancer: A Stage II ovarian cancer indicates that the disease has spread from the ovary to the pelvic organs, such as the fallopian tubes, uterus, or rectum. Stage II has the following three subcategories:
- IIA: Cancer is present in one or both of the ovaries and has spread into the uterus or fallopian tube(s). No cancer cells are present in the abdomen
- IIB: Cancer is present in one or both of the ovaries and has spread to other pelvic organs, such as the bladder, colon, or rectum
- IIC: Cancer is present in one or both ovaries, and it has spread to the pelvic organs. It is also found in fluid samples from the abdomen
Stage III ovarian cancer: In stage III ovarian cancer, the cancer has spread from the ovary and beyond the pelvis, to the abdomen or nearby lymph nodes. This stage has the following three subcategories:
- IIIA: Cancer is present in one or both of the ovaries; the cancer cells are also present in microscopic amounts in the abdominal fluid
- IIIV: Cancer is present in one or both of the ovaries; the cancer cells are also present in tumors (smaller than 2 cm in size) in the abdominal lining
- IIIC: Cancer is present in one or both of the ovaries; the cancer cells are also present in tumors (larger than 2 cm in size) in the abdominal lining, or in the nearby lymph nodes
Stage IV ovarian cancer: A Stage IV ovarian cancer indicates that the disease has spread from the ovary to distant sites within the body, such as the liver or lungs.
Additional and Relevant Useful Information for Clear Cell Adenocarcinoma of Ovary:
The following DoveMed website link is a useful resource for additional information:
Related Articles
Test Your Knowledge
Asked by users
Related Centers
Related Specialties
Related Physicians
Related Procedures
Related Resources
Join DoveHubs
and connect with fellow professionals

0 Comments
Please log in to post a comment.