What are the other Names for this Condition? (Also known as/Synonyms)
- Broken Neck
- Cervical Spine Fracture
- Hangman's Fracture
What is Cervical Fracture? (Definition/Background Information)
- A Cervical Fracture is a break or crack that occurs in one of the three vertebral columns of the spine, called the cervical vertebrae. The other two vertebral columns of the spine are the lumber (lower back) and thoracic (mid-back)
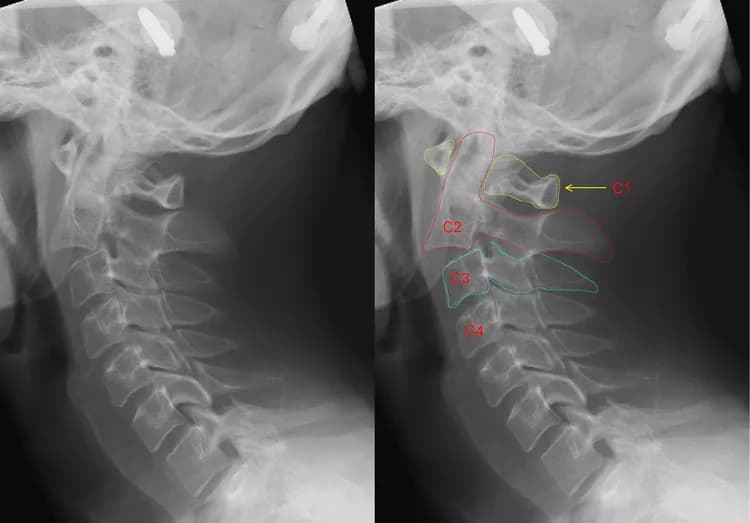
- There are seven bones (C1-C7) within the cervical vertebrae that support the head and neck. A Cervical Fracture is also known as a Neck Fracture
- Cervical Fractures are usually caused by any high-energy impact such as an automobile accident or a fall. Individuals, who participate in athletic sports, such as football or hockey, also have an increased risk of such fracture types
- Treatment for a Cervical Fracture depends on the location of the injury and the type of fracture sustained
There are different types of Cervical Fractures. Physicians categorize Cervical Fractures based on the injury pattern and if a spinal cord injury has occurred. Classifying the fracture patterns may help determine the appropriate treatment. The most common types of Cervical Fractures include:
- Odontoid Fracture: An Odontoid Fracture is a fracture of the pars interarticularis (also called the axis) on the pedicle of the C2 vertebrae. A fracture to the odontoid makes it difficult for individuals to have a full range of motion of their neck. This type of fracture is common in children
- Hangman’s Fracture: A Hangman’s Fracture is another type of fracture that occurs to the C2 vertebrae
- Jefferson Fracture: Jefferson Fracture is a fracture through the anterior and posterior arches of the C1 vertebra. When these fracture types occur, the C1 vertebra may also fracture
- Teardrop Fracture: A Teardrop Fracture is an injury that occurs when one or more of the vertebrae within the lower neck fracture. A Teardrop Fracture is a flexion compression injury that may affect the surrounding ligaments and discs
Who gets Cervical Fracture? (Age and Sex Distribution)
- Approximately 80% of all Cervical Fractures occur in individuals between the ages of 18 to 25 years old
- Such fractures occur in both males and females. However, it is more commonly seen in males than females (in a 4:1 ratio)
- No ethnic or racial preference is seen
What are the Risk Factors for Cervical Fracture? (Predisposing Factors)
Common risk factors for Cervical Fractures include:
- Participation in any rough or high-impact sport such as football or hockey
- An advanced age
- Degenerative joint disease (osteoarthritis)
- Osteoporosis, which is a disease that weakens the bones
It is important to note that having a risk factor does not mean that one will get the condition. A risk factor increases ones chances of getting a condition compared to an individual without the risk factors. Some risk factors are more important than others.
Also, not having a risk factor does not mean that an individual will not get the condition. It is always important to discuss the effect of risk factors with your healthcare provider.
What are the Causes of Cervical Fracture? (Etiology)
Some common causes of Cervical Fractures include:
- A high-energy impact traumatic event such as an automobile accident
- A fall from a significant height
- Participation in any rough or high-impact sport
- Domestic violence, street fights
Location of fracture in the cervical region statistic:
- Fracture of the C1 vertebra accounts for around 10% of all Cervical Fractures and 2% of all spinal cord injuries
- C2 fractures represent 33% of all Cervical Fractures and 15% of all spine injuries
- Fractures of the C6 or C7 vertebra account for 50% of all Cervical Fractures
What are the Signs and Symptoms of Cervical Fracture?
The signs and symptoms of a Cervical Fracture include
- Pain, tenderness, and swelling in the neck
- Difficulty swallowing
- Limited range of motion in the neck
- Tingling sensation, weakness, and noticeable numbness of the neck
- Blurred vision
- Loss of consciousness due to injury to the brain
- Paralysis of the arms or legs
Cervical Fractures are very serious injuries that can lead to paralysis or the possibility of death. Individuals with serious neck injuries should not be moved (from their position) and requires immediate medical treatment by a trained healthcare professional.
How is Cervical Fracture Diagnosed?
Individuals are likely to be taken to the emergency room where a healthcare professional will inquire about symptoms, any previous physical activities, and how the injury occurred. If a neck injury is suspected, the physician may refrain from performing a thorough physical examination, until after any spinal X-rays are completed.
Cervical Fracture diagnostic tests may include:
- Neurological tests: The physician will assess an individual’s neurological status. This includes testing sensory neurons, motor responses, and reflexes, which can determine if the nervous system is damaged. In addition, the physician will test the individual’s reflexes that can help determine where an injury to the spinal cord has occurred
- X-ray of the spine: X-rays are commonly used in evaluating a fracture. An x-ray image can show if bones have been displaced. This diagnostic imaging test helps provide a clear image of the bone, identify the exact location of the injury, and determine the extent of the fracture
- Computerized tomography (CT) scan of the spine: A CT scan takes a series of x-ray images from several different angles. These images are then merged to create cross-sectional images of bones and soft tissues of the body, which then allows the physician to examine the spine and surrounding structures to confirm a diagnosis
- Magnetic resonance imaging (MRI) of the spine: An MRI is a detailed scan that uses a magnetic field to generate thorough images of the interior bones and soft tissues of the neck. This also helps to confirm the diagnosis
Many clinical conditions may have similar signs and symptoms. Your healthcare provider may perform additional tests to rule out other clinical conditions to arrive at a definitive diagnosis.
What are the possible Complications of Cervical Fracture?
The complications of a Cervical Fracture may include:
- Paraplegia (paralysis of the legs)
- Quadriplegia (paralysis of both the arms and legs)
- Damage to the nerves or blood vessels within the spine
How is Cervical Fracture Treated?
Treatments for Cervical Fractures (or Neck Fractures) depend on the location of the injury and the type of fracture that occurred, and include both surgical and nonsurgical methods.
Nonsurgical treatment measures for a Cervical Fracture may include:
- For minor compression fractures, complete immobilization of the neck with a cervical brace may be required for 6 to 8 weeks. This is required to restrict an individual’s movement until the bone heals
- Non-steroidal anti-inflammatory oral medications, such as ibuprofen and naproxen, can help reduce the pain and swelling in the neck
- Skeletal traction is an orthopedic mechanism to hold pieces of the broken bones together
- A physical therapist and an occupational therapist may help with rehabilitation exercises. These exercises may also help individuals retrain themselves in new ways of performing regular activities
- Speech therapy can help with any speech or swallowing difficulties
Surgical treatment measures for a Cervical Fracture may include:
- Open reduction and internal fixation (ORIF) of Cervical Fracture: Open reduction and internal fixation is a surgical intervention procedure to realign the fractured bone into its original position. An internal fixation device is used to hold the bone together until it is fully healed. Different internal fixation devices, such as plates, screws, and rods, may be used to hold the bone together
- Anterior cervical discectomy and fusion (ACDF): This surgical procedure is performed through an incision within the front of the neck and involves removing the damaged cervical vertebra to relieve pressure on the spinal cord and/or nerves
How can Cervical Fracture be Prevented?
It is always recommended to be careful and consciously aware while performing any physical activities, such as sports, or even some normal daily activities that could lead to situations involving accidents. Children must be provided a safe environment to work, study, or play. Any probable dangers involved should also be anticipated, and safety measures adopted
A few ways to further help prevent unwanted injuries or a Cervical Spine Fracture include:
- Always wear a seat belt while driving or traveling as a passenger in an automobile vehicle
- Avoid jumping head first into shallow water spots
- Individuals who participate in any high-risk sports, such as football or hockey, should wear appropriate safety equipment to help prevent the possibility of any injury or bone fracture
What is the Prognosis of Cervical Fracture? (Outcomes/Resolutions)
- The long-term prognosis of Cervical Fractures depends on the severity of the injury, which can range from complete recovery to total paralysis (quadriplegia)
- The prognosis is usually good in individuals whose Cervical Fractures have been stabilized. However, the range of motion of the head and neck may still be at least 50% restricted after stabilization of the upper part of the neck
- Treatment of a Cervical Fracture that exclusively involves internal fixation is frequently ineffective. Internal fixation followed by a cervical fusion usually improves the prognosis
- Overall, due to the improvement in surgical techniques and healthcare over the last 40 years, the outcomes have improved significantly for individuals with spinal cord injuries
Additional and Relevant Useful Information for Cervical Fracture:
Hangman’s Fracture results from a forced hyperextension of the neck; the term was first introduced in 1965 by Schneider et al.
Related Articles
Test Your Knowledge
Asked by users
Related Centers
Related Specialties
Related Physicians
Related Procedures
Related Resources
Join DoveHubs
and connect with fellow professionals

0 Comments
Please log in to post a comment.