What are the other Names for this Condition? (Also known as/Synonyms)
- BP (Bullous Pemphigoid)
- Pemphigoid
What is Bullous Pemphigoid? (Definition/Background Information)
- Bullous Pemphigoid is an uncommon skin disease mainly affecting the elderly population, characterized by the formation of blisters on the skin. Occasionally, blisters also form on moist, mucous membrane lined surfaces of the body (Mucous Membrane Pemphigoid)
- The blisters are formed when the immune system attacks the ‘basement membrane’ layer of the skin with antibodies (proteins). Sometimes, medications can trigger the immune system
- The antibodies cause an abnormal inflammatory reaction, which leads to large, fluid-filled blister formations on the skin. The armpits, lower abdomen, and upper thighs (areas that flex) are frequently involved
- Bullous Pemphigoid is treated with medications that suppress the immune system, which include corticosteroids and prednisone. If left untreated, spontaneous remissions and exacerbations occur over many months or years
- In elderly people with a poor health condition, Bullous Pemphigoid can even be fatal
Who gets Bullous Pemphigoid? (Age and Sex Distribution)
- Bullous Pemphigoid is usually observed in the elderly population, with a majority of those affected being over the age of 60 years
- Childhood and infant-onset Bullous Pemphigoid has been reported in rare cases
- Members of both sexes (males and females) are affected equally
- The condition is observed worldwide; there is no racial or ethnic predilection
What are the Risk Factors for Bullous Pemphigoid? (Predisposing Factors)
There are no well-defined risk factors associated with Bullous Pemphigoid; though, certain factors can trigger the development of the condition. These may include:
- The triggers may be prescription drugs such as penicillin, etanercept, furosemide, and sulfasalazine
- Sunburn, ultraviolet light therapy, and radiation therapy
- A genetic predisposition to develop Pemphigoid may cause activation of the immune system in certain aging individuals
- Individuals with certain neurological diseases, such as stroke, dementia, and Parkinson’s disease, may be at a higher risk for Bullous Pemphigoid
It is important to note that having a risk factor does not mean that one will get the condition. A risk factor increases ones chances of getting a condition compared to an individual without the risk factors. Some risk factors are more important than others.
Also, not having a risk factor does not mean that an individual will not get the condition. It is always important to discuss the effect of risk factors with your healthcare provider.
What are the Causes of Bullous Pemphigoid? (Etiology)
While the exact cause of Bullous Pemphigoid is not known, it is considered to be an autoimmune disease.
- In an autoimmune disease, the immune system starts attacking one’s own body. The immune system attacks the skin’s basement membrane [the basement membrane is a thin layer connecting the skin’s outer layer (epidermis) to the inner layer (dermis) with antibodies (proteins)
- The antibodies cause an abnormal inflammatory reaction, which leads to large, fluid-filled blisters forming on the skin
- The antibodies are ‘IgG immunoglobulins’ and the specific targets in the skin are proteins (BP180, BP230), which are associated with a basement component known as ‘hemidesmosomes’
What are the Signs and Symptoms of Bullous Pemphigoid?
Signs and symptoms associated with Bullous Pemphigoid include:
- A rash is often the first symptom that may be seen weeks before any other symptom develops. The rash, which is usually ring-shaped or round, can disappear on its own
- Blisters appear later, commonly on creases and body folds or on the abdomen. The armpits, lower abdomen, and upper thighs (areas that flex) are often involved
- Blisters are large and filled with clear or blood-stained fluid surrounded by reddish or normal appearing skin. They do not rupture readily, are itchy, and can get quite large; when they burst, though, they can heal without scarring
- In severe cases, blisters appear over the entire surface of the skin and on mucous membrane lined areas (such as the mouth and inner nose)
- Mouth involvement can cause pain, difficulty in eating, and coughing. Inner nose involvement can cause nosebleeds
- The disease worsens and improves over time (exacerbations and remissions)
How is Bullous Pemphigoid Diagnosed?
The diagnosis of Bullous Pemphigoid may include:
- Usually the physician is able to diagnose Bullous Pemphigoid by examining the skin condition
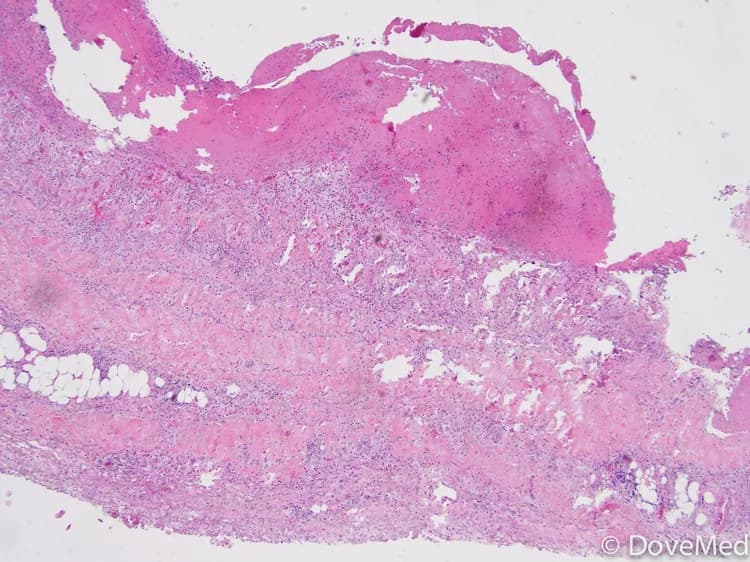
- Skin biopsy: A small sample of the blister (biopsy) may be taken to confirm the diagnosis. The tissue sample is then sent to the laboratory to be examined by a pathologist under the microscope
- Antibodies can also be shown to be circulating in blood (by indirect immunofluorescence method)
Many clinical conditions may have similar signs and symptoms. Your healthcare provider may perform additional tests to rule out other clinical conditions to arrive at a definitive diagnosis.
What are the possible Complications of Bullous Pemphigoid?
Complications associated with Bullous Pemphigoid are:
- Ruptured blisters can become infected and lead to sepsis (more likely in elderly people and those with poor health). Infection can also delay wound healing
- Scarring of the mouth and eye when these areas are involved
- Due to the prolonged use of steroids and immunosuppressants, adrenal gland insufficiency, osteoporosis, and bone fractures may also develop
How is Bullous Pemphigoid Treated?
There are several treatment options for Bullous Pemphigoid. These include:
- The goal is to use the lowest possible dose of medication to relieve itching, promote skin healing, and reduce blister formation
- Corticosteroids, such as prednisone, in pill form are used to reduce the inflammation. It may take a few weeks for blisters to stop appearing, following which the steroids have to be tapered (reduced in dosage)
- Corticosteroid ointments cause fewer side effects than the pills; hence, they can be tried even in severe forms of the disease before starting the pills. Clobetasol is a very effective steroid-based ointment
- The oral antibiotics doxycycline and minocycline have anti-inflammatory side effects that can sometimes control Bullous Pemphigoid without using corticosteroids like prednisone
- Even if these do not control, but improve the symptoms, the dose of prednisone needed may be lowered, decreasing side effects
- The chemotherapy agent methotrexate can also be used in small doses as a steroid dose sparing agent
- Stronger immunosuppressants, such as Azathioprine and Mycophenolate mofetil, are used to decrease the requirement of corticosteroids if the agents listed above are not effective
- It is not unusual for a patient with Bullous Pemphigoid to have a topical treatment routine and several oral medications, to control their disease. Close follow-up and frequent visits to the healthcare provider are required
- Rituximab is a genetically engineered antibody that targets the antibody producing lymphocytes, thus helping in immune suppression. It can be used in severe cases resistant to standard treatment
- When blistering is severe, hospital admission, antibiotics to prevent bacterial infection, and the application of sterile dressings over blisters and raw areas is necessary
- High dose intravenous immunoglobulins may be used in severe cases
Most individuals require treatment that range anywhere from 6 to 60 months. The treatment can be stopped when the desired response is seen. Monitoring the levels of the causative antibodies circulating in the serum can guide when tapering or discontinuing the medications.
How can Bullous Pemphigoid be Prevented?
There are no known measures to prevent Bullous Pemphigoid. Some of the known triggers that can be avoided are:
- Prescription drugs such as penicillin, etanercept, sulfasalazine, and furosemide
- Ultraviolet light therapy and radiation therapy
- Exposure to sun
What is the Prognosis of Bullous Pemphigoid? (Outcomes/Resolutions)
- Untreated Bullous Pemphigoid may have spontaneous remissions and relapses that may spread over months or years. The most severe form, when involving the airways, can be fatal, if left untreated
- The treatment administered aims to control rather than cure the condition. In most cases, long-term remissions are observed after 6 months or up to even 5 years of therapy. Once it clears up, treatment can be stopped
- Morbidity and risk of death is higher in those with widespread or aggressive disease, individuals on high dose corticosteroids and immunosuppressants, and those with other underlying medical conditions
- The high dose treatment with steroids and immunosuppressants may worsen underlying hypertension, diabetes mellitus, and heart diseases.
- Long-term steroid doses cause the adrenal glands to atrophy. Abrupt discontinuation can lead to numerous severe effects, including death
- Steroidal therapy may cause stomach ulcers, gastrointestinal bleeds, and agranulocytosis (when the bone marrow fails to produce enough white blood cells)
- Long-term oral steroid treatments can cause calcium to leave the bones, or cause a serious condition called avascular necrosis of the bone
- Patients on long-term corticosteroids should have a medical alerting device or other means to advise all healthcare workers of their status
Additional and Relevant Useful Information for Bullous Pemphigoid:
- Infant-Onset Bullous Pemphigoid is more commonly being observed now. Blisters usually appear over the palms, soles, and on the face
- A form of Bullous Pemphigus occurs in women during pregnancy. It is termed pemphigus gestationis
- Some other forms of Bullous Pemphigoid are generalized bullous form, vesicular form, vegetative form, generalized erythroderma form, urticarial form, nodular form, and acral form. They differ in the distribution, appearance, and severity of the blisters
Related Articles
Test Your Knowledge
Asked by users
Related Centers
Related Specialties
Related Physicians
Related Procedures
Related Resources
Join DoveHubs
and connect with fellow professionals


0 Comments
Please log in to post a comment.