What are the other Names for this Condition? (Also known as/Synonyms)
- Benign Bone Neoplasm - Osteochondroma
- Multiple Osteochondroma (occurring in Diaphyseal Aclasis)
- Neoplasm of Bone - Osteochondroma
What is Osteochondroma of Bone? (Definition/Background Information)
- Bone Tumor - Osteochondroma is a fairly common benign outgrowth of the bone. They account for about 30% of all benign bone tumors
- This benign outgrowth of bone, affects both the medullary and cortical portion of the bone
- Osteochondromas include a cartilaginous cap that projects from the bone surface. It is this “cap”, which causes the tumor to grow bigger
- The Osteochondroma is actually a misplaced epiphyseal growth plate on the bone surface, and not really a true neoplasm
- They can occur, either as random solitary lesions, or as multiple lesions. Multiple lesions are seen in the autosomal dominant disorder - hereditary multiple exostosis
- The most common sites of occurrence are the distal femur, proximal humerus, or the proximal tibia
- Not all Osteochondromas require to be treated. Surgical removalof the lesion is performed, when some of them cause symptoms
Who gets Osteochondroma of Bone? (Age and Sex Distribution)
- Osteochondromas commonly occur in children and young adults, under the age of 20 years
- Both male and females are prone to get the tumor
- No ethnic or racial preference is noted
What are the Risk Factors for Osteochondroma of Bone? (Predisposing Factors)
Risk factors for Bone Tumor - Osteochondroma include:
- Osteochondromas can occur as random solitary/multiple lesions
- Multiple lesions are seen with the autosomal dominant disorder - hereditary multiple exostosis, and in the contiguous gene deletion syndromes Langer-Giedion syndrome and Potocki-Shaffer syndrome
It is important to note that having a risk factor does not mean that one will get the condition. A risk factor increases ones chances of getting a condition compared to an individual without the risk factors. Some risk factors are more important than others.
Also, not having a risk factor does not mean that an individual will not get the condition. It is always important to discuss the effect of risk factors with your healthcare provider.
What are the Causes of Osteochondroma of Bone? (Etiology)
- The cause of development of Osteochondromas is unknown
- Some scientists believe that Osteochondromas are caused by defects in bone development
What are the Signs and Symptoms of Osteochondroma of Bone?
The signs and symptoms of Osteochondroma include:
- Mass-like growth on the affected bone; this palpable mass can cause symptoms due to pressure on adjacent structures, such as nerves
- Blockage of blood vessels due to pressure from the mass can cause damage to surrounding tissues
- Pressure from an Osteochondroma may result in venous thrombosis or arterial pseudo-aneurysms
- Pain at the site of the mass; pain can occur due to fractures in the stalk of Osteochondroma
The tumor most commonly occurs around the knee joint, other locations include:
- Distal part of femur (above kneecap) in 1/3rd of the cases, proximal tibia (below kneecap) in 1/5th cases
- Less commonly the tumor can occur in bones of feet, scapula, humerus bone, bones of hand, and pelvic bones; very rarely, such tumors can occur in bones of the spine
How is Osteochondroma of Bone Diagnosed?
The diagnosis of Osteochondroma is made as follows:
- A thorough medical history and a complete physical examination is necessary
- X-rays of the affected bone
- MRI of the affected bone
- Biopsy of the mass, which is then examined by a pathologist under a microscope, for a definitive diagnosis
Many clinical conditions may have similar signs and symptoms. Your healthcare provider may perform additional tests to rule out other clinical conditions to arrive at a definitive diagnosis.
What are the possible Complications of Osteochondroma of Bone?
The complications of Osteochondromas include:
- The tumor mass can cause pressure on adjacent structures, such as the nerves. In severe cases, nerve damage may occur
- Osteochondroma pressure may result in venous thrombosis or arterial pseudo-aneurysms. Such venous thrombus can cause thromboembolism
- In less than 1% individuals, Osteochondroma can turn malignant; into a tumor called malignant osteosarcoma. Greater the number of Osteochondromas, greater are the chances that some of them may turn malignant
How is Osteochondroma of Bone Treated?
- Not all Osteochondromas need treatment
- Surgery to remove the lesion is indicated, when the lesions cause symptoms. In such cases, removal of the entire cartilaginous cap is necessary during the surgery, to prevent their recurrence
How can Osteochondroma of Bone be Prevented?
- There are no known methods to prevent Osteochondromas
- Once they occur, surgical removal of the entire cartilaginous cap is necessary, to prevent any recurrence
What is the Prognosis of Osteochondroma of Bone? (Outcomes/Resolutions)
- In a majority of individuals, Osteochondromas do not cause any symptoms
- In those who have symptoms, surgical excision results in cure. The prognosis is usually excellent
It is estimated that very small fraction of individuals may have recurrence after surgery (2% recurrence - according to Mayo Clinic).
Additional and Relevant Useful Information for Osteochondroma of Bone:
When a pathologist examines Osteochondroma grossly and microscopically, the following features are noted:
Macroscopic (gross) findings:
Sessile Osteochondromas are semicircular tumors and have a thin cartilage cap. The periosteum from the affected bone forms a thin membrane around the tumor. Irregular calcification lines differentiate cartilage from cancellous bone. The tumor contains fatty and hematopoietic marrow that reflects the condition of the affected bone. With a pedunculated Osteochondroma, the lesion has the appearance of a mushroom with a bony stalk and a cap or cartilaginous tissue. To appreciate the full thickness of the cartilaginous cap, it is important to cut the lesion perpendicular to the stalk.
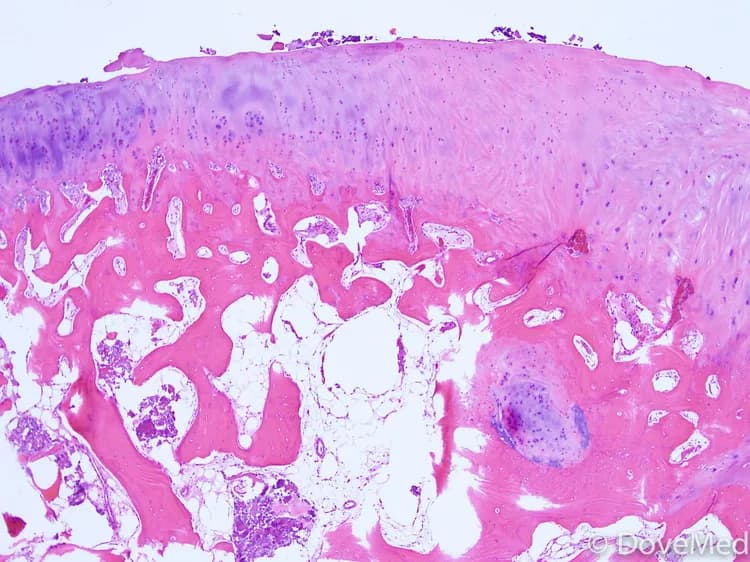
Microscopic (histopathology) findings:
A thin pink membrane surrounds the outermost portion of the cap, representing the periosteum that has been lifted-off the bone. Both bone and cartilage should be seen in a single section, otherwise a chondrosarcoma should be considered, due to the extensive amount of cartilage. Clusters ofchondrocytes in lacunae make up the cartilaginous cap, and abundant chondroid matrices are present between the clusters. As seen in epiphyseal plates, the chondrocytes towards the base are arranged in columns, and bony trabeculae arise from the cartilage plate.
Differential diagnosis:
Subungual exostosis, bizarre parosteal osteochondromatous proliferation, and secondary chondrosarcoma are included in the differential diagnosis. The distal phalanx is involved in subungual exostosis and presents as a rapidly-growing mass. However, Osteochondromas are rarely seen in subungual locations, and the bone has a mature appearance not seen in subungual exostosis. Bizarre parosteal osteochondromatous proliferation usually involves the small bones of the hand and has a blue pattern of calcification not seen in Osteochondromas. If an Osteochondroma becomes malignant, it is typically an osteosarcoma. Secondary sarcoma should be suspected, if there is a soft tissue mass showing irregular mineralization.
On a radiologist examinationof the X-rays, the following features may be seen:
Findings include a pedunculated or sessile projection from the bone surface. The cortex and the medullary cavity are continuous with the involved bone. At the site of the Osteochondroma, the affected bone is typically (unusually) wide, and if the tumor is pedunculated, it will normally point away from the nearest joint.
Related Articles
Test Your Knowledge
Asked by users
Related Centers
Related Specialties
Related Physicians
Related Procedures
Related Resources
Join DoveHubs
and connect with fellow professionals

0 Comments
Please log in to post a comment.