What are the other Names for this Condition? (Also known as/Synonyms)
- Blue Mole
- Common Blue Naevus
- Dermal Melanocytoma
What is Blue Nevus? (Definition/Background Information)
- A nevus (plural nevi) is a mole on the skin that can occur on any part of the body
- A Blue Nevus is a benign proliferation of melanocytes (which makes melanin pigment) in the dermis or skin. It is typically an acquired condition
- The mole can be present anywhere on the body, though half of them are seen on the hands and feet. They appear as papules or nodules and are normally pigmented in blue shades
- Normally, these moles are present during childhood and adolescence. Blue Nevi are generally asymptomatic in nature, but may present cosmetic concerns in some individuals
- Sun exposure may be a risk factor for acquiring the condition. Blue Nevus is observed to occur in a random manner and the cause is unknown
- Treatment is generally not required for a Blue Nevus unless it presents cosmetic issues. The prognosis is generally excellent with or without treatment, since these moles are generally benign
Who gets Blue Nevus? (Age and Sex Distribution)
- Blue Nevus is a skin condition that may be present at birth or form at any age in an individual. However, mainly children and adolescents are generally noted to have this type of nevus. It is uncommon in older age
- Both males and females are affected and there is no gender bias observed
- All racial and ethnic groups are at risk, but this nevus type is more frequent in fair-skinned individuals (Caucasians)
What are the Risk Factors for Blue Nevus? (Predisposing Factors)
The risk factors identified for Blue Nevus include:
- Sun exposure
- Generally, lighter-skinned races or individuals (such as Caucasians of America and Europe) are at a higher risk compared to other darker-skinned racial groups (such as Africans and Asians)
It is important to note that having a risk factor does not mean that one will get the condition. A risk factor increases ones chances of getting a condition compared to an individual without the risk factors. Some risk factors are more important than others.
Also, not having a risk factor does not mean that an individual will not get the condition. It is always important to discuss the effect of risk factors with your healthcare provider.
What are the Causes of Blue Nevus? (Etiology)
- The cause of Blue Nevus formation is unknown
- It is believed to be acquired due to certain unknown factors. The cause may be probably genetic
What are the Signs and Symptoms of Blue Nevus?
Blue Nevus may not present any signs and symptoms in most cases. The general features of the condition include:
- It is a benign tumor of melanocytic cells on the skin. They may be single or many in numbers
- It is usually well-defined and less than 10 mm in size (along the larger dimension). These moles/nevi are usually round or oval in shape; although they can be of any shape
- They can be present as a papule or nodule (a raised mass). A papule is an area of abnormal skin tissue that is less than 1 centimeter around. Usually a papule has distinct borders, and it can appear in a variety of shapes
- The benign nevus is usually slow-growing and pigmented. The color may vary from blue to blue black
- The pigment color over the mole is usually uniform, although sometimes irregular pigmentation is observed. This can cause concerns of a melanoma and may need to be investigated by a healthcare provider. However, usually a Blue Nevus does not transform into a melanoma (a malignant skin cancer)
- Blue Nevi can occur anywhere on the body. However, 50% of them are seen to arise on the dorsal aspect of the hands and feet. Other common sites include the head and neck area (and face)
They usually occur early in life and grow in size, as the child becomes an adult. As one age, these moles may become smaller and in many cases, they can disappear.
How is Blue Nevus Diagnosed?
A Blue Mole/Nevus is diagnosed through the following tools:
- Complete physical examination with evaluation of medical history
- Dermoscopy: It is a diagnostic tool where a dermatologist examines the skin using a special magnified lens
- Wood’s lamp examination: In this procedure, the healthcare provider examines the skin using ultraviolet light. It is performed to examine the change in skin pigmentation
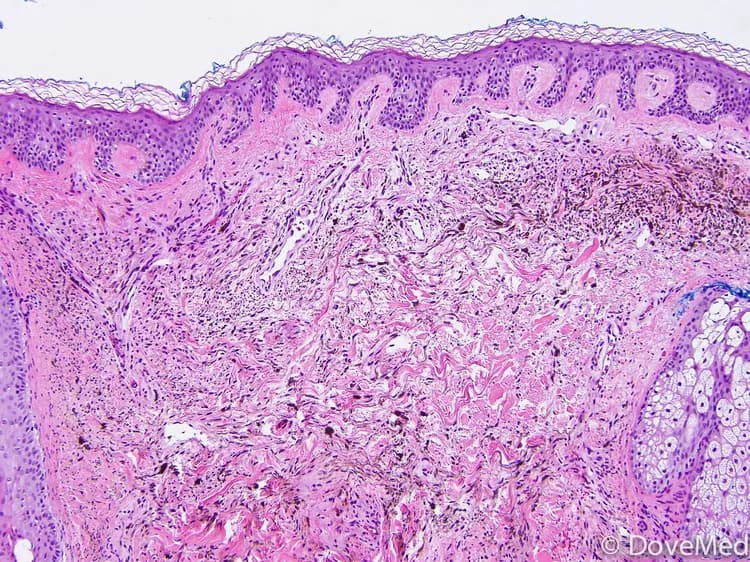
- Skin biopsy: A skin biopsy is performed and sent to a laboratory for a pathological examination. The pathologist examines the biopsy under a microscope. After putting together clinical findings, special studies on tissues (if needed) and with microscope findings, the pathologist arrives at a definitive diagnosis
Note: In majority of the cases, no biopsy is necessary. But they may be performed to rule out other conditions presenting similar signs and symptoms.
Many clinical conditions may have similar signs and symptoms. Your healthcare provider may perform additional tests to rule out other clinical conditions to arrive at a definitive diagnosis.
What are the possible Complications of Blue Nevus?
There are frequently no complications that arise from a Blue Nevus.
- Nevertheless, in some individuals, it may give rise to cosmetic concerns
- Scratching or itching of the moles may lead to bleeding and ulceration. This can cause secondary bacterial or fungal infections to develop
How is Blue Nevus Treated?
The treatment measures for Blue Nevus include:
- The healthcare provider may chose to regularly observe the benign mole; a “wait and watch” approach may be followed
- Surgical excision and removal of the mole, if necessary for cosmetic reasons
- Blue Nevus can also be excised through electrocautery surgical procedure
How can Blue Nevus be Prevented?
Current medical research has not established a way of preventing the occurrence of Blue Nevi. However the following measures can help these moles from becoming either a dysplastic mole or a melanoma:
- Minimize direct exposure to the sun’s ultraviolet (UV) rays
- Avoid tanning beds and sun lamps
- Perform self-examination of your skin, from head to toe, once a month (especially if you are at risk)
- Get a professional skin exam from a healthcare provider, once a year
- Do not pick or scratch the moles, which can cause it to ulcerate and bleed
What is the Prognosis of Blue Nevus? (Outcomes/Resolutions)
- The prognosis of Blue Nevus is excellent on its complete excision and removal
- Since, these are benign conditions, the prognosis is excellent even if no treatment is provided and only periodic observation maintained
Additional and Relevant Useful Information for Blue Nevus:
The following DoveMed website link is a useful resource for additional information:
Related Articles
Test Your Knowledge
Asked by users
Related Centers
Related Specialties
Related Physicians
Related Procedures
Related Resources
Join DoveHubs
and connect with fellow professionals

0 Comments
Please log in to post a comment.