What are the other Names for this Condition? (Also known as/Synonyms)
- Acute Tracheitis
- Bacterial Infection of the Trachea
- Tracheitis
What is Bacterial Tracheitis? (Definition/Background Information)
- Tracheitis is a rare bacterial infection of the trachea (windpipe/ breathing tube). It usually follows a recent upper respiratory tract viral infection, such a common cold
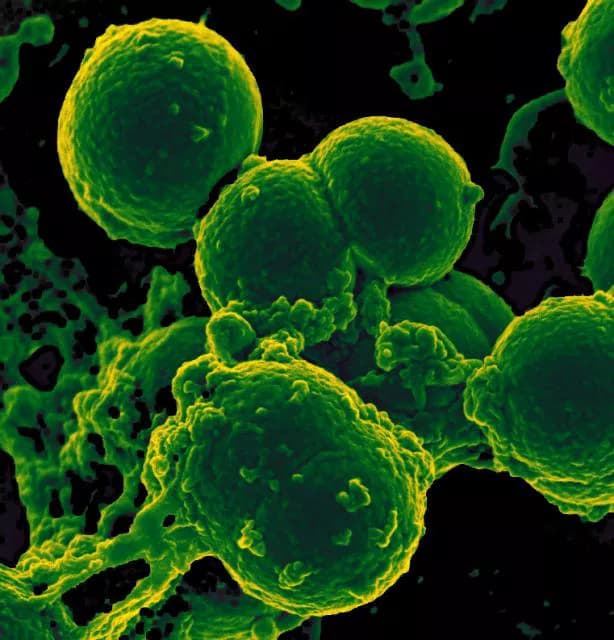
- Bacterial Tracheitis may cause severe airway obstruction that may result in a life-threatening situation. The most common organism responsible for the infection is Staphylococcus aureus
- The major site of the disease is at the narrowest part of the trachea. The infection leads to a collection of pus with membrane formation in the trachea, which interferes with breathing
- Bacterial Tracheitis usually affects pre-school and early school-aged children. It is very serious in young children, possibly because of their small trachea that is easily blocked by swelling
- The classic signs and symptoms of Bacterial Tracheitis include deep cough, high-grade fever, stridor (high-pitched abnormal sound while breathing), and difficulty in breathing. The condition is diagnosed by history, physical examination, along with a few tests that include tracheal culture, x-ray of the trachea, and laryngobronchoscopy
- This Bacterial Infection of the Trachea is treated with antibiotics. A majority of the children recover with no long-term complications; the most dangerous complication of Tracheitis is obstruction of the airways, which may even result in death
- Vaccination is the most effective way to prevent Bacterial Tracheitis
Who gets Bacterial Tracheitis? (Age and Sex Distribution)
- Bacterial Tracheitis usually affects pre-school and early school-aged children, but it may affect children of any age group (from 3 weeks to 15 years)
- Males are affected more often than females, in a 2:1 ratio
What are the Risk Factors for Bacterial Tracheitis? (Predisposing Factors)
- Bacterial Tracheitis usually follows an upper respiratory tract viral infection that is most often caused by influenza or para-influenza virus
It is important to note that having a risk factor does not mean that one will get the condition. A risk factor increases ones chances of getting a condition compared to an individual without the risk factors. Some risk factors are more important than others.
Also, not having a risk factor does not mean that an individual will not get the condition. It is always important to discuss the effect of risk factors with your healthcare provider.
What are the Causes of Bacterial Tracheitis? (Etiology)
Bacterial Tracheitis may be caused by a variety of bacteria. The common organisms responsible for this infection include:
- Staphylococcus aureus
- Streptococcus pyogenes
- Streptococcus pnuemoniae
- Moraxella catarrhalis
- Hemophilus influenza type b
What are the Signs and Symptoms of Bacterial Tracheitis?
The signs and symptoms of Bacterial Tracheitis may include:
- Deep or barking cough
- Inspiratory stridor: A high pitched crowing sound that is heard, while the child breathes in
- Scratchy feeling in the throat, hoarse voice
- Fever
- Chest pain, difficulty breathing
- Ear ache
- Headache
- Dizziness - feeling lightheaded
- Tachypnea - increased respiratory rate
How is Bacterial Tracheitis Diagnosed?
In order to diagnose Bacterial Tracheitis, the physician will initially perform a physical examination with evaluation of medical history. Bacterial Tracheitis usually follows a viral infection of the upper respiratory tract. Hence, the initial symptoms of cough, runny nose, and low-grade fever, may be present.
During physical examination the physician will look for:
- High-grade fever
- Tachypnea - increased respiratory rate
- Stridor
- Intercostal retractions: The muscles between the ribs pull in, as the child tries to breathe
- Worsening respiratory distress: Breathing will be very difficult for the child as the disease progresses, because of increasing airway obstruction
- Cyanosis: Bluish or grey discoloration around the lips, due to decreasing oxygen levels in blood
- There is no specific position of the body in which the child feels relieved or comfortable
Diagnostic tests that may be required include:
- Pulse oximetry: A sensor is placed on a thin part of the body, such as a fingertip or earlobe, to measure the amount to oxygen in blood
- Tracheal culture: Tracheal secretions are taken and sent to the laboratory, where they are placed on a special dish to observe the growth of the bacteria
- Nasopharyngeal culture: Mucous secretions from the uppermost part of the throat are sent to the laboratory, to check for any bacterial growth
- X-ray of the trachea: To examine the extent of the narrowing of trachea
- X-ray of the chest is taken to detect infection in the lungs
- Blood test: A complete blood count is done that shows an increased white blood cell count
- A laryngobronchoscopy is the most effective way to diagnose Bacterial Tracheitis. It is a thin instrument that is used to directly visualize the larynx and trachea (airway)
What are the possible Complications of Bacterial Tracheitis?
Bacterial Tracheitis is a life-threatening emergency condition in children. The possible complications may include:
- Airway tracheal obstruction, which is an acute emergency that can lead to death
- Toxic shock syndrome: If Bacterial Tracheitis is caused by Staphylococcus aureus, then S. aureus can produce a toxin that causes fever, shock, and multiple organ failure
- Pneumonia (infection of the lungs)
- Pulmonary edema (presence of fluid in the lungs)
How is Bacterial Tracheitis Treated?
In Bacterial Tracheitis there is significant danger of tracheal obstruction, which may be fatal, so the main focus is to keep the trachea patent.
- Antibiotics are cornerstone of the treatment and are given through a vein (intravenous)
- Generally, an admission in the ICU is required with continuous monitoring of blood pressure, pulse, temperature, and oxygen levels
- Endotracheal intubation: It is a tube that is placed in the airways, to help with breathing, and which is connected to a ventilator (a machine that supports breathing)
How can Bacterial Tracheitis be Prevented?
- The most effective way to prevent Bacterial Tracheitis is vaccination
- Vaccination against influenza, measles, and streptococcus pneumoniae, is essential for all children to prevent development of the infection
What is the Prognosis of Bacterial Tracheitis? (Outcomes/Resolutions)
- The prognosis of Bacterial Tracheitis is excellent with early recognition of the condition and effective treatment
- With early and prompt treatment, a majority of children affected by Tracheitis recover, having no long-term complications
Additional and Relevant Useful Information for Bacterial Tracheitis:
Bacterial Tracheitis is potentially a life-threatening emergency. An urgent medical attention should be immediately sought, if a child has had a recent upper respiratory tract infection and suddenly develops high-grade fever, with worsening cough and breathing difficulties.
Related Articles
Test Your Knowledge
Asked by users
Related Centers
Related Specialties
Related Physicians
Related Procedures
Related Resources
Join DoveHubs
and connect with fellow professionals

0 Comments
Please log in to post a comment.