What are the other Names for this Condition? (Also known as/Synonyms)
- Anus Cancer
- Cancer of Anal Canal
- Cancer of the Anus
What is Anal Cancer? (Definition/Background Information)
- The anus is a part of the body that is connected to the rectum of the large intestine and is the passageway, through which stool leaves the body
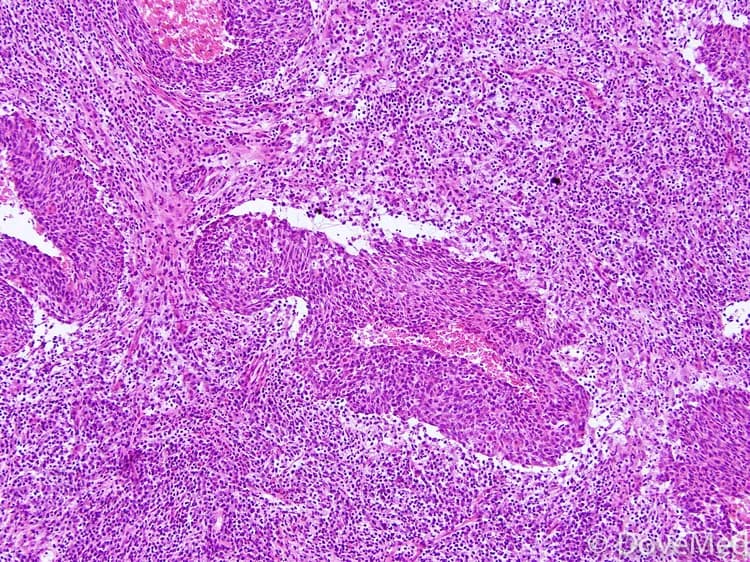
- Anal Cancer is a form of cancer that affects the anus or anal canal. It arises after genetic mutations transform healthy cells into abnormal cells following uncontrollable growth
- Abnormal cancer cells can form new cancer cells that subsequently invade other tissues in the body. Additionally, these abnormal cells do not die as healthy cells typically do, resulting in the formation of an abnormal mass or tumor
- Many different types of cells are located in the anal canal meaning that various types of tumors can form in the anus. However, some tumors are benign (non-cancerous), while others are malignant (cancerous)
- The two most common type of Anal Cancers include adenocarcinoma of the anal canal and squamous cell carcinoma of anal canal. The squamous cell carcinoma type is known to be associated with human papillomavirus infection (HPV), which is a sexually transmitted disease
- The signs and symptoms of Anal Cancer include rectal bleeding, constipation, and the presence of lumps in the anal canal. It is typically diagnosed through a rectal examination
- Anal Cancer is treated using radiation therapy, chemotherapy, and/or surgery. The earlier the detection, the better are the treatment outcomes
Who gets Anal Cancer? (Age and Sex Distribution)
- Anal Cancer is relatively rare, comprising about 1-2% of all gastrointestinal cancers. It is typically diagnosed in individuals aged 50 years or older
- Both males and females can develop Anal Cancer
- Individuals of all race/ethnic background may be affected
What are the Risk Factors for Anal Cancer? (Predisposing Factors)
Multiple risk factors have been associated with Anal Cancer that include:
- Age: Most individuals with Anal Cancer are typically over the age of 50
- Anal sex is a significant risk factor
- Smoking: Smoking can increase the risk for various cancers including Anal Cancer
- Human papillomavirus (HPV): Infection with HPV increases the risk for several cancer forms, including Anal Cancer. HPV is a sexually transmitted infection that can cause genital warts
- Immunosuppression: Individuals being treated with immunosuppressive drugs (organ transplant patients), or those with human immunodeficiency virus (HIV) infection have an increased risk
- Chronic local inflammation: Individuals with anal fistulas or open anal wounds have a higher risk
It is important to note that having a risk factor does not mean that one will get the condition. A risk factor increases one's chances of getting a condition compared to an individual without the risk factors. Some risk factors are more important than others.
Also, not having a risk factor does not mean that an individual will not get the condition. It is always important to discuss the effect of risk factors with your healthcare provider.
What are the Causes of Anal Cancer? (Etiology)
Anal Cancer is caused by genetic changes that turn healthy cells into cancer cells. These cancer cells have lost the ability to control their growth leading to the formation of tumors.
The tumors found in the anal canal can be either benign (non-cancerous) or malignant (cancerous). Moreover, because there are various types of cells in the anus, each cell type can become cancerous to form a different kind of Anal Cancer.
The different types of Anal Cancer include:
- Squamous cell carcinoma: It is the most common subtype of Anal Cancer. The cancer develops in the squamous cells that line the lower region of the anus, as well as the majority of the anal canal
- Cloacogenic carcinoma: A subtype of squamous cell carcinoma, it affects a region of the anus called the cloaca. It accounts for about 25% of all Anal Cancers
- Adenocarcinoma: It forms in the cells that are part of the upper part of the anus (in the glands that produce mucus found under the anal lining)
- Basal cell carcinoma: A small proportion of Anal Cancers are basal cell carcinomas. These form in the skin surrounding the anus
- Melanomas: It forms in cells that produce the melanin pigment that are found in the skin or anal lining (mucosal melanoma)
It is known that human papillomavirus (HPV) is the most common cause of Anal Cancer. HPV is sexually transmitted and results in the formation of genital warts. HPV infection is commonly caused by anal sexual intercourse. Sexually-active individuals (both males and females) have a higher risk for HPV infection from unsafe sex and multiple partners. However, only a small percentage of individuals with HPV infection develop Anal Cancer.
What are the Signs and Symptoms of Anal Cancer?
The signs and symptoms associated with Anal Cancer may include:
- Bleeding in the anus or rectum
- Pain in the anal region
- A mass or lump in the anal canal
- Persistent anal itching
- Change in bowel movements or habits
- Discharge or mucus from the anus
Some of the above symptoms of Anal Cancer are also associated with more common conditions such as hemorrhoids. Therefore, it is important to consult a physician in case of any of the above being noted.
How is Anal Cancer Diagnosed?
The following procedures may be used to diagnose Anal Cancer:
- Physical exam: A physician may first conduct a physical exam, which can also help in gaining more information about a patient’s health history and past illnesses
- Digital rectal examination (DRE): During a DRE, the physician inserts a lubricated, gloved finger into the lower area of the rectum. This allows the detection of any lumps or abnormal growth in the region
- Anoscopy: Anoscopy is a procedure using a special medical device, called an anoscope (a lighted tube), to examine the anal canal and rectum
- Endo-anal or endo-rectal ultrasound study: An ultrasound transducer (or probe) is inserted into the anal canal and rectum. The probe emits high-energy sounds waves that bounce of internal organs and tissues, creating a visual picture of the anal canal
- Biopsy: A biopsy is the removal of samples of cells or affected tissues for further exam under the microscope by a pathologist for any signs of cancer
Following a confirmation of Anal Cancer, additional procedures are performed to determine the stage of cancer and whether it has spread (metastasized) to other parts of the body. This will help the physician in choosing the most appropriate treatment method.
- Imaging of the pelvic and abdomen region: Computerized tomography (CT), magnetic resonance imaging (MRI), and positron emission tomography (PET) may be used to scan the pelvis and abdomen
- Chest X-rays: The lungs may be examined to determine if the cancer has spread to the chest area
Many clinical conditions may have similar signs and symptoms. Your healthcare provider may perform additional tests to rule out other clinical conditions to arrive at a definitive diagnosis.
What are the possible Complications of Anal Cancer?
Anal Cancer rarely metastasizes to distant regions of the body; only a small percentage of anal tumors actually spread. If such a metastasis does take place, then it is typically to the lungs and liver.
How is Anal Cancer Treated?
As with most cancer types, early detection is associated with better survival results. The treatment method used is dependent on the location of the tumor, its histological subtype, and the stage of the cancer.
The following treatment options may be considered for Anal Cancer:
- Chemotherapy: Chemotherapy drugs are typically taken as pills or injected directly into a vein. These drugs travel through the body to kill any cancer cells. But, they can also kill healthy cells within the gastrointestinal tract and adjacent regions. The side effects include vomiting, nausea, and hair loss
- Radiation therapy: Radiation therapy involves using X-rays to kill cancerous cells. High-powered radiation beams are directed to particular body regions to target the cancer. In the process, healthy cells can also be damaged. The side effects include hardening and shrinking of the anal canal, reddening of the skin, and sores surrounding the anus
Radiation therapy and chemotherapy can be used as a combination therapy, which is now considered the standard treatment method for Anal Cancer patients. Combinational therapy increases the effects of both types of treatment. However, the side effects are cumulative.
Surgery: Different surgical procedures may be performed depending on the stage of Anal Cancer, as determined by the healthcare provider.
- In the early stages, when the tumor is small and has not metastasized outside the anus, local excision may be done. During this procedure, the tumor is removed along with some of the nearby healthy tissue. The anal sphincter muscles that surround the anus and control bowel movements are not damaged during this procedure. Therefore, patients still have the ability to control their bowel movements following this procedure
- For late-stage Anal Cancers or cancers that have not responded to other treatment options, a procedure called abdominoperineal resection is performed. The surgeon removes the anus, rectum, and a section of the colon. The remaining part of the colon is attached to the abdomen to form an opening, termed colostomy. The colostomy allows wastes to travel directly from the colon, into a disposable bag located outside the body
How can Anal Cancer be Prevented?
Generally, it is not possible to prevent Anal Cancer. However, the following measures may be considered to lower one's risk for the same:
- Practicing safe-sex can reduce the risk for HPV and HIV infections, the two key risk factors for Anal Cancer
- Additionally, getting vaccinated against HPV is also considered a preventative measure against Anal Cancer. Gardasil and Cervarix are two vaccines administered against HPV
- As smoking is a risk factor for Anal Cancer, restraining from smoking can also reduce one’s risk for cancer
Regular medical screening can also be undertaken for individuals with a high risk for Anal Cancer.
- Anal pap smear: It is the same screening method used to detect cervical cancer in women. It involves using a swab to collect cells from the anal canal and then examining the cells under a microscope
- Anoscopy: It is another procedure used to screen for Anal Cancer. A special type of scope (called anoscope) is used to examine the lining of the anal canal
What is the Prognosis of Anal Cancer? (Outcomes/Resolutions)
The prognosis of Anal Cancer depends on the following factors:
- Histological subtype of the cancer
- Size of the tumor
- Tumor location in the anal canal
- Stage of the tumor
- Whether it has spread (metastasized) to the lymph nodes and other regions
Anal Cancer is staged as follows:
- Stage I: Anal Cancer is 2 cm in length, or less
- Stage II: Anal Cancer is larger than 2 cm in length
- Stage IIIA: Anal Cancer is of any size that has spread to nearby organs, including the vagina, urethra, or bladder; and it has spread to the lymph nodes near the rectum
- Stage IIIB: Anal Cancer is of any size that has spread to nearby areas and lymph nodes, or it has spread to the lymph nodes in the pelvis
- Stage IV: Anal Cancer has spread to distant parts, such as the lungs, liver, or brain
Furthermore, as with other forms of cancer, early detection is correlated with higher survival rates. Most Anal Cancer types can be treated effectively, if they are detected early. Tumors that have recurred may also be treated effectively.
For patients diagnosed with Anal Cancer, it is important to have periodic follow-up appointments with the physician, to evaluate the effects of the current treatment method and monitor for any recurrent tumors.
Additional and Relevant Useful Information for Anal Cancer:
Vaccinations against HPV:
- Males and females between the ages of 9 and 26 years can be vaccinated with Gardasil
- Females between the ages of 10 and 25 years can be vaccinated with Cervarix
Related Articles
Test Your Knowledge
Asked by users
Related Centers
Related Specialties
Related Physicians
Related Procedures
Related Resources
Join DoveHubs
and connect with fellow professionals

0 Comments
Please log in to post a comment.