Actinic Keratosis of Skin
What are the other Names for this Condition? (Also known as/Synonyms)
- Actinic (Solar) Keratosis of Skin
- Atrophic Keratosis
- Sun-Induced Skin Changes - Keratosis
What is Actinic Keratosis of Skin? (Definition/Background Information)
- Prolonged exposure to the sun’s ultraviolet rays, results in damage of skin DNA causing patches of rough, scaly, and thickened skin. This is called Actinic Keratosis (AK) of Skin
- The affected regions typically include, body areas exposed to the sun, such as the face, neck, bald portion of the scalp, hands, and the upper chest
- Actinic Keratosis of Skin is considered precancerous, since it has the potential to progress into the skin cancer squamous cell carcinoma of skin
Who gets Actinic Keratosis of Skin? (Age and Sex Distribution)
- Actinic Keratosis of Skin form over many years. Hence, they are mostly observed in adults over 50 years of age or more. They can also occur in the 20 and over age group, if there is significant early sun exposure
- No gender inequality has been observed; both men and women are equally prone to the condition. This factor varies across geographical regions and is based on the nature of one’s occupation and recreational activities
- Dark-skinned people are less affected; fair-skinned individuals are affected the most
- Australia has a very high prevalence of Actinic Keratosis of Skin (1 in 2 adults over 40 years of age)
What are the Risk Factors for Actinic Keratosis of Skin? (Predisposing Factors)
The risk factors for Actinic Keratosis of Skin include:
- Exposure to intense sun for long periods during the course of work or due to outdoor sports activities
- People living in geographical regions where hot-dry climatic conditions prevail
- Individuals with weak immune system, which could be due to cancer treatment, AIDS, or those on immunosuppressant drugs after receiving an organ transplant
- Those who easily sunburn because of light pigmentation
It is important to note that having a risk factor does not mean that one will get the condition. A risk factor increases one's chances of getting a condition compared to an individual without the risk factors. Some risk factors are more important than others.
Also, not having a risk factor does not mean that an individual will not get the condition. It is always important to discuss the effect of risk factors with your healthcare provider.
What are the Causes of Actinic Keratosis of Skin? (Etiology)
- Actinic Keratosis of Skin is caused when skin cells (the keratinocytes that form the epidermis) are damaged from prolonged (and frequently severe) exposure to the ultraviolet (UV) component of the sun over decades
- The source of UV may be from recreational indoor tanning and medical phototherapy too
- Welding, flying airplanes, and other occupations can expose workers to increased ultraviolet radiation
- Research has indicated that the human papillomavirus (HPV) can multiply the risk for Actinic Keratosis. The mechanism by which the virus contributes to the formation of Actinic Keratosis is presently unclear
What are the Signs and Symptoms of Actinic Keratosis of Skin?
The main diagnostic criterion for Actinic Keratosis of Skin is the visible change in the skin. The signs and symptoms generally include:
- Initial formation of slightly rough skin lesions, which later turn to dry, pink, scaly patches
- Gradually the lesions get thicker and inflamed. The patches grow in size
- Multiple lesions are often seen within a region or in other sun-exposed areas
- Itching or burning may be experienced
- Pain, bleeding, and seeping results from minor trauma
- Typical body regions affected include the face and lips, hairless portion of the scalp, neck, arms (hand, forearm), and upper chest
How is Actinic Keratosis of Skin Diagnosed?
A diagnosis of Actinic Keratosis of Skin is made by:
- Physical examination of the skin
- The history and visual inspection are usually adequate for a diagnosis of the condition
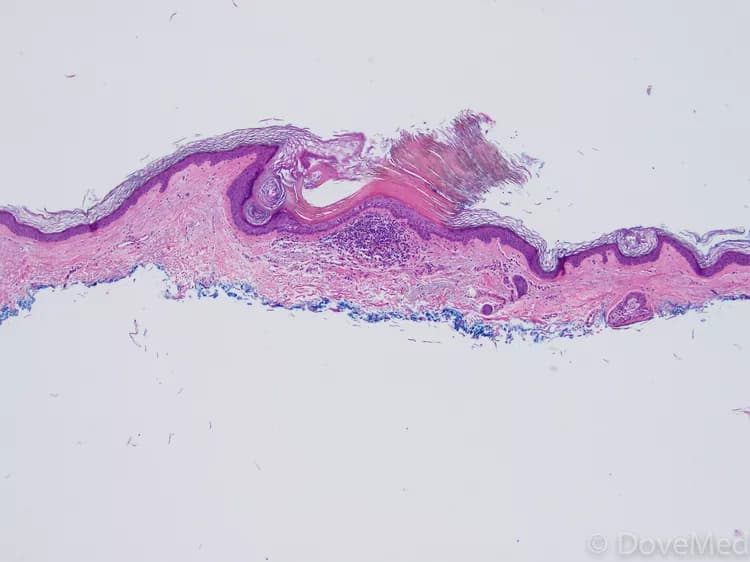
- A skin biopsy is done when there is a diagnostic question in the mind of the practitioner. Most frequently the differential diagnosis lies between Actinic Keratosis and superficial squamous cell carcinoma of the skin or in situ basal cell carcinoma of the skin. The skin biopsy is analyzed by a pathologist under a microscope for a definitive diagnosis
Many clinical conditions may have similar signs and symptoms. Your healthcare provider may perform additional tests to rule out other clinical conditions to arrive at a definitive diagnosis.
What are the possible Complications of Actinic Keratosis of Skin?
The possible complications due to Actinic Keratosis of Skin could be:
- Discomfort and irritability of the affected skin
- The main complication that may arise from Actinic Keratosis of Skin is that it could develop to form squamous cell carcinoma (a common form of skin cancer). This normally takes place if the treatment is delayed, or the condition is left untreated
How is Actinic Keratosis of Skin Treated?
Commencing early treatment can help prevent a progressive deterioration of Actinic Keratosis of Skin, and avoid complications. Several management measures are available and these include:
- Use of topical ointments, lotions, and creams. These may be antiseptic and anti-inflammatory applications. Most common are imiquimod, 5-flurouracil, diclofenac, and Ingenol topical
- Chemical peeling, in which strong chemicals applied on the skin, cause it to peel and shed, giving way to formation of new skin
- Use of photodynamic light or laser therapy: Light destroys the damaged cells after they are treated with a special medical application
- Cryotherapy: Controlled use of liquid nitrogen to freeze intracellular water, killing the cells and causing them to slough-off
- Complete removal of the affected skin by a biopsy is also curative
How can Actinic Keratosis of Skin be Prevented?
A few methods to prevent Actinic Keratosis of Skin include:
- Avoiding prolonged and chronic exposure to the sun. If this is unavoidable ( due to an occupational requirement), then taking safety steps to reduce exposure to the UV rays, by using sunscreens with high sun-protection factor, wide-brimmed hats, and protective clothing
- Being aware of the hazards of prolonged sun exposure and taking steps to protect oneself. Modifying one’s profession to stay out of the sun during the period when it is the most intense
- Avoiding excessive sunbathing (particularly for fair-skinned individuals), usage of tanning beds, sun lamps, and chemical agents that accelerate sun tanning
- Individuals, who are regularly exposed to the sun or work under the sun, should get their skin periodically examined by a physician. This is crucial if they suspect, or if there are any noticeable skin changes
What is the Prognosis of Actinic Keratosis of Skin? (Outcomes/Resolutions)
- Early diagnosis, followed by consistent follow-up, with timely treatment of Actinic Keratosis of Skin, and consistent sun protection can help result in an excellent prognosis
- Severe cases of Actinic Keratosis may cause permanent facial (or body) marks and pigmented scars, especially if proper treatment is not administered, or is delayed. In such cases, cosmetic surgery may be required to restore facial skin
- There is also a chance that some of the lesions may develop to form invasive skin cancers, when chronic sun exposure and other risk factors are high
Additional and Relevant Useful Information for Actinic Keratosis of Skin:
Even though dark-skinned individuals are at a very low risk for Actinic Keratosis of Skin, it has been observed that skin malignancies that form in them, are known to be particularly aggressive. The cause for this finding is unknown.
Related Articles
Test Your Knowledge
Asked by users
Related Centers
Related Specialties
Related Physicians
Related Procedures
Related Resources
Join DoveHubs
and connect with fellow professionals


0 Comments
Please log in to post a comment.