What are the other Names for this Condition? (Also known as/Synonyms)
- Achondroplastic Dwarfism
- Chondrodystrophia Fetalis Calcificans
What is Achondroplasia? (Definition/Background Information)
- Achondroplasia is a genetic disorder that affects bone growth and development. It is caused by a mutation in the FGFR3 gene
- Most cases of Achondroplasia (about 90%) arise due to a new mutation, not passed on by the parents. The disorder can also be passed on to the offspring (as an autosomal dominant trait) from one or both parents having the disorder
- The normal function of the protein coded by the FGFR3 gene is to inhibit cartilage growth. A normal cartilage is required for proper bone growth. When FGFR3 gene is mutated, it results in increased inhibition of cartilage growth, which ultimately results in suppressed skeletal growth
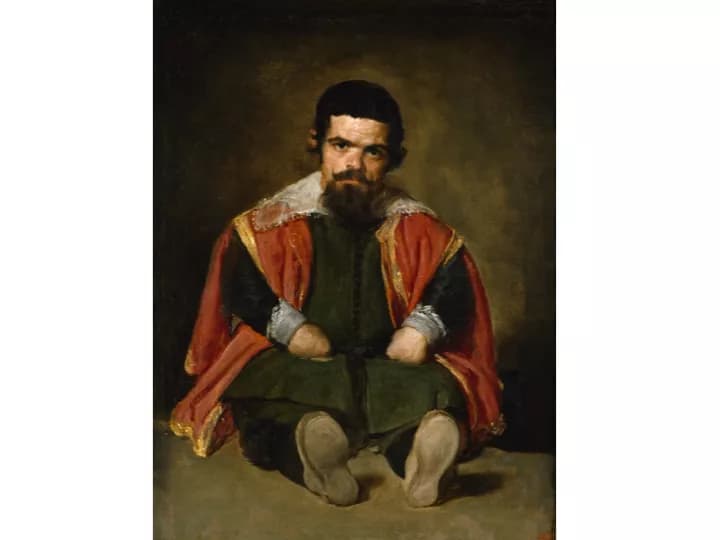
- Achondroplasia affected individuals are short in stature and often have disproportionately short limbs, when compared to the rest of their body
- Achondroplasia does not have a cure. However, the bony abnormalities are usually not associated with changes in intelligence, reproductive capacity, or how long the individuals may live
- Affected individuals may need lifelong treatment that may involve the use of growth hormones, limb lengthening, and other surgical procedures, with appropriate management of the complications that arise from the condition
- The prognosis for Achondroplasia is generally ‘fair to good’ and many individuals are able to generally lead normal lives, with only a slight reduction in overall life expectancy
Who gets Achondroplasia? (Age and Sex Distribution)
- Achondroplasia is one of the most common causes of dwarfism in the world. It is the most common cause of abnormal skeletal development. The chance of occurrence is 1 case per 15,000-40,000 births
- Individuals with Achondroplasia are affected from birth and symptoms exist throughout their lives
- It has equal frequency of incidence in both males and females
- The condition can occur worldwide. There is no racial or ethnic preference noticed
What are the Risk Factors for Achondroplasia? (Predisposing Factors)
The risk factors of Achondroplasia include:
- In 10% of Achondroplasia affected individuals, the condition is inherited as an autosomal dominant trait, i.e. the FGFR3 gene mutation is passed on to the child from an affected parent. Thus, a positive family history of the condition increases one’s risk
- In 90% of Achondroplasia affected individuals, the FGFR3 gene mutation is a new mutation (whose parents do not have the mutated gene). The risk factors in these individuals remain unknown
It is important to note that having a risk factor does not mean that one will get the condition. A risk factor increases one’s chances of getting a condition compared to an individual without the risk factors. Some risk factors are more important than others.
Also, not having a risk factor does not mean that an individual will not get the condition. It is always important to discuss the effect of risk factors with your health care provider.
What are the Causes of Achondroplasia? (Etiology)
Achondroplasia is a genetic disorder in which there is a mutation of FGFR3 gene. This mutation can happen in two ways:
- Through a new random mutation; this happens in a majority of cases (90%)
- Through autosomal dominant inheritance, which occurs in the remaining 10% of cases
Autosomal dominant: Autosomal dominant conditions are traits or disorders that are present when only one copy of the mutation is inherited on a non-sex chromosome. In these types of conditions, the individual has one normal copy and one mutant copy of the gene. The abnormal gene dominates, masking the effects of the correctly function gene. If an individual has an autosomal dominant condition, the chance of passing the abnormal gene on to their offspring is 50%. Children, who do not inherit the abnormal gene, will not develop the condition or pass it on to their offspring.
- In a normal individual, the FGFR3 gene codes for the fibroblast growth factor receptor 3 (FGFR3) protein, which is important in developing and maintaining bone growth
- When a mutation occurs in this gene, endochondral (cartilage) growth is affected, thus affecting skeletal growth
What are the Signs and Symptoms of Achondroplasia?
Achondroplasia usually begins to manifest at birth and the signs and symptoms may include:
- Short-statured individuals:
- Males with Achondroplasia grow to an average height of 52 inches (132 cm)
- Females grow to an average height of 49 inches (124 cm)
- Short limbs, especially the upper limbs
- Delayed motor milestones: Starting to walk may be delayed up to 18-24 months
- Short fingers and toes
- Large head with prominent forehead
- Bowed legs
- Decreased muscle tone
- Loose joints
- Crowded and or misaligned teeth
- Compression of spinal cord due to narrowing of the spinal canal
- Breathing difficulties due to smaller rib cage capacity
- Recurrent ear infections, which may progress to hearing issues
How is Achondroplasia Diagnosed?
A diagnosis of Achondroplasia would involve:
- While the disease cannot be confirmed until after birth, the physical features of Achondroplasia are distinct and are usually apparent on a prenatal ultrasound exam
- After birth, Achondroplasia is initially (and often) diagnosed based on a thorough evaluation of the individual’s medical history and a complete physical examination. An evaluation of medical history will determine, if there is a presence of predisposing factors such as a family history
- The diagnosis may be confirmed by a simple radiological x-ray testing of the skeleton
- Genetic testing may be used, but is usually not necessary to arrive at a diagnosis
- Imaging techniques may be used if there are other associated conditions (such as a spinal cord compression)
Many clinical conditions may have similar signs and symptoms. Your healthcare provider may perform additional tests to rule out other clinical conditions to arrive at a definitive diagnosis.
What are the possible Complications of Achondroplasia?
The complications of Achondroplasia may include:
- Delayed gross motor milestones such a beginning to sit, walk, etc.
- Frequent ear infections that may lead to hearing loss
- Restrictive lung disease due to a smaller rib cage. This can manifest as difficulty in breathing, frequent lung infections, and other conditions
- Spinal stenosis or narrowing of the spinal canal can compress the spinal cord. This may cause paralysis, breathing difficulty, pain, bladder or bowel incontinence, tingling and weakness in the legs, making daily life further complicated or difficult for those with the condition
How is Achondroplasia Treated?
Currently, there is no cure for Achondroplasia. The treatment measures for managing the signs and complications of this genetic disorder may include:
- Treatment with growth hormones and limb lengthening surgeries, though these remain controversial. Their efficacy may be depend on various factors such as the general condition of the individual, age, family support system, access to advanced healthcare facilities, and other factors
- Growth hormones may be used to increase the growth rate of individuals affected with Achondroplasia during their first year of life
- Surgery can also be performed to lengthen the arms or legs. It is not a common practice though, because it is painful and takes a long duration of time
- Preventative measures may be taken to help control the complications that arise due to Achondroplasia
- Ear infections should be promptly treated using antibiotics and ear tubes, in order to prevent hearing loss from occurring
- Dental crowning may be used to fix misaligned, crowded teeth
How can Achondroplasia be Prevented?
Currently, there are no known methods to prevent Achondroplasia from occurring in a child.
- But, it is possible to provisionally diagnose Achondroplasia before birth, and hence, offer a choice to the parents as to how they want to proceed with the pregnancy. Prenatal ultrasound is helpful in this regard
- Genetic testing can also be done before birth, to determine if the infant has the disorder. Cells can be obtained using chorionic villi sampling or amniocentesis and subsequent genetic tests can be conducted to determine if the FGFR3 mutation exists
- Novel non-invasive diagnostic testing, in which the fetal cells are extracted from mother’s blood and analyzed for the presence of mutation (analysis of cell-free fetal DNA), can also be performed
- If there is a family history of the condition, then genetic counseling will help assess risks before planning for a child
- Active research is currently being performed to explore the possibilities for treatment and prevention of inherited and acquired genetic disorders
What is the Prognosis of Achondroplasia? (Outcomes/Resolutions)
- Currently, there is no cure for Achondroplasia. However, the symptoms can be managed to improve the individual’s overall quality of life
- Most individuals reach an average height of 4-5 feet. Intelligence is usually not affected by the mutated FGFR3 gene, and hence, they are able to lead relatively normal lives
- Preventative measures, appropriate and timely management of complications can help individuals live a better quality of life
Additional and Relevant Useful Information for Achondroplasia:
Please visit our Congenital & Genetic Disorders Center for more physician-approved health information:
https://www.dovemed.com/diseases-conditions/congenital-genetic-disorders/
Related Articles
Test Your Knowledge
Asked by users
Related Centers
Related Specialties
Related Physicians
Related Procedures
Related Resources
Join DoveHubs
and connect with fellow professionals

0 Comments
Please log in to post a comment.