Inflammatory bowel disease (IBD), of which Crohn's disease and ulcerative colitis are the main types, is on the increase in the United States, affecting more than 1.6 million people and explaining perhaps the increase in advertisements offering treatments and cures. Another intestinal disease is colon cancer, a leading cause of death, which is linked to diet and one's genetic predisposition to the disease.
What is already known in the field of cell biology is that a transcription factor, called hepatocyte nuclear factor 4-alpha (HNF4-alpha), plays a key role in both diseases, transcription factors being proteins that help transcribe DNA into its close cousin, RNA, which is then translated into proteins which do the work of the cell. HNF4-alpha comes in two major isoforms, P1-HNF4-alpha and P2-HNF4-alpha (hereafter P1 and P2, respectively), but just how these isoforms are distributed in the gut and how each isoform plays a role in colitis and colon cancer are not understood.
Now, working on mice, a team of researchers at the University of California, Riverside has determined the distribution of the P1 and P2 isoforms in the colon. They report in the journal eLife that maintaining a balance of P1 and P2 is crucial for reducing risk of contracting colon cancer and colitis.
"P1 and P2 have been conserved between mice and humans for 70 million years," said Frances M. Sladek, a professor of cell biology, who led the research project. "Both isoforms are important and we want to keep an appropriate balance between them in our gut by avoiding foods that would disrupt this balance and consuming foods that help preserve it. What these foods are is our next focus in the lab."
The intestine is the only adult tissue in the body that expresses both P1 and P2. Sladek and her team have shown for the first time that these isoforms perform non-redundant functions in the intestine and are relevant to colitis and colitis-associated colon cancer.
"Our study also suggests that finding a drug to stabilize one isoform should be more effective than targeting both isoforms for treating colitis and colon cancer," said Karthikeyani Chellappa, the first author of the research paper and a former postdoctoral researcher in Sladek's lab.
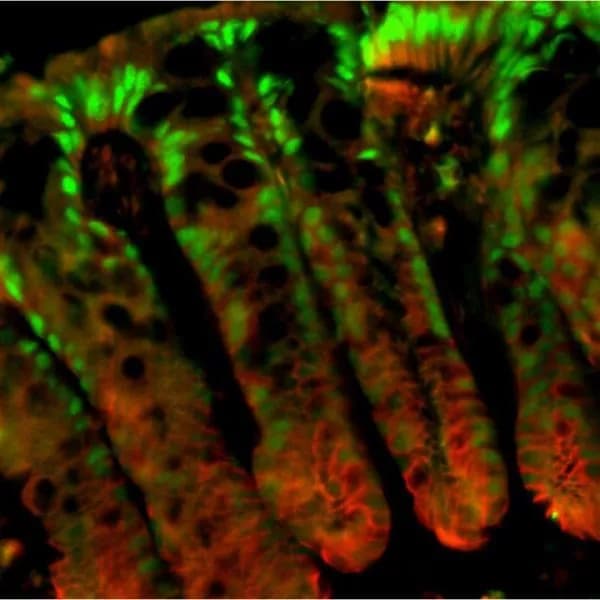
Sladek explained that the colonic epithelial surface has finger-like invaginations (into the colonic wall) called colonic crypts that house stem cells at their base. These stem cells help regenerate new epithelial cells that continuously migrate up towards the surface, thus ensuring complete renewal of the intestinal lining every three-five days.
The researchers observed that the P1-positive cells were found in the surface lining and the top portion of the crypt (green in the accompanying image) while P2-positive cells were mostly in the proliferative compartment in the lower half of the crypt (proliferation marker is red in the image.) Further, when transgenic mice -- genetically engineered to have only either P1 or P2 -- were subjected to a carcinogen and, subsequently, to an irritant to stress the epithelial lining of the colon, the researchers found that the P1 mice showed fewer tumors than wildtype control mice. When treated with irritant alone, these mice were resistant to colitis. In sharp contrast, mice with only P2 showed more tumors and were much more susceptible to colitis.
The researchers explain these findings by invoking the "barrier function" -- a mucosal barrier, generated by the colon's epithelial cells, that prevents bacteria in the gut from entering the body. In the case of P1 mice, this barrier function was enhanced. The P2 mice, on the other hand, showed a compromised barrier function, presumably allowing bacteria to pass through.
Next, the researchers examined genes expressed in the P1 and P2 mice. They found that RELM-beta, a cytokine (a signaling molecule of the immune system) expressed in the gastrointestinal tract and implicated in colitis, was expressed far more in the P2 mice than the P1 mice.
"This makes sense since a reduced barrier function means bacteria can go across the barrier, which activates RELM-beta," Sladek said. "We also found that the P2 protein transcribes RELM-beta more effectively than the P1 protein."
Next, Poonamjot Deol, an assistant project scientist in Sladek's lab and the second author of the eLife study, will lead a project aimed at understanding how diet affects the distribution of P1 and P2 in the gut. She and others in the lab also plan to investigate how obesity and colitis may be linked. (Diet studies performed in Sladek's lab in the past illustrated soybean oil's adverse effect on obesity.)
"In the case of colitis, could soybean oil be playing a part in allowing bacteria to get across the barrier function?" Deol said. "We do not know. We know its detrimental effect on obesity. But more research needs to be done where colitis is concerned."
The above post is reprinted from materials provided by University of California - Riverside. The original item was written by Iqbal Pittalwala.Note: Materials may be edited for content and length.
Disclaimer: DoveMed is not responsible for the adapted accuracy of news releases posted to DoveMed by contributing universities and institutions.
Primary Resource:
Chellappa, K., Deol, P., Evans, J. R., Vuong, L. M., Chen, G., Briançon, N., ... & Sladek, F. M. (2016). Opposing roles of nuclear receptor HNF4α isoforms in colitis and colitis-associated colon cancer. eLife, 5, e10903.
Related Articles
Test Your Knowledge
Asked by users
Related Centers
Related Specialties
Related Physicians
Related Procedures
Related Resources
Join DoveHubs
and connect with fellow professionals

0 Comments
Please log in to post a comment.