Bodywide Immune Response Important For Fighting Cancer, Researchers Say
Fighting off cancer requires the concerted efforts of immune molecules throughout the body, rather than just in the tumor itself, according to a new study of laboratory mice by researchers at the Stanford University School of Medicine.
The finding helps settle an ongoing dispute among clinicians as to whether systemic, or whole-body responses, are as important as a robust response by immune cells in the tumor itself. The study may help clinicians understand why some people with cancer respond favorably to cancer immunotherapy, while others experience little or no benefit. It also suggests ways that the effectiveness of ongoing therapies could be quickly and easily monitored.
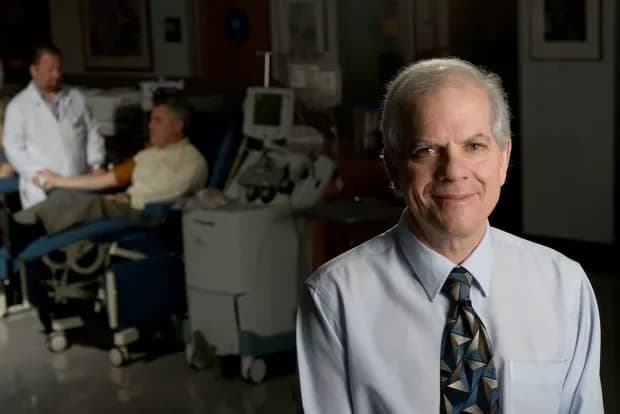
"Immunotherapy can be remarkably effective against cancer, but we don't know why some patients respond and some don't," said Edgar Engleman, MD, professor of pathology and of medicine. "We don't understand the parameters that determine efficacy. In this study, we analyzed millions of living cells simultaneously for 40 parameters from multiple tissues throughout the body to show that you need a systemwide immune response to effectively attack and eradicate a tumor."
Engleman is the senior author of the study, which will be published online Jan. 19 in Cell. The lead authors are Matthew Spitzer, PhD, a former Stanford graduate student who is now a postdoctoral scholar at the University of California-San Francisco; former Stanford postdoctoral scholar Yaron Carmi, PhD, who is now an assistant professor at Tel Aviv University; and Stanford postdoctoral scholar Nathan Reticker-Flynn, PhD.
Two-pronged approach
The researchers compared the immune responses of a special group of laboratory mice engineered to spontaneously develop triple-negative breast cancers. These cancers are resistant to a type of immunotherapy known as checkpoint blockade. Recently, however, Engleman and his colleagues showed that they could stimulate a successful immune response and eradicate tumors in the animals with a two-pronged approach that incorporated both a tumor-binding antibody and molecules that activated a type of immune cell called a dendritic cell.
"This finding allowed us to directly compare the responses to two immunotherapies," said Engleman. "What's going on in an effective response that's not happening in the ineffective response? What we found was quite revealing and gratifying."
Spitzer, Carmi and their colleagues collaborated with co-author Garry Nolan, PhD, a professor of microbiology and immunology at Stanford who has developed a way to use a technique known as mass cytometry to monitor the physical attributes of individual cells in samples of millions or billions. This allows researchers to piece together a dynamic picture of how multiple cell populations respond in real time to changing conditions like disease or drug therapies.
Spitzer and his colleagues used the technology to monitor the rise and fall of various populations of immune cells within the tumor as well as in other tissues -- including the lymph nodes, spleen, bone marrow and peripheral blood -- throughout the body immediately after immunotherapy and throughout tumor rejection.
The researchers found that in animals treated with the effective, two-pronged approach, the prevalence of immune cells -- including macrophages, dendritic cells and T cells -- in the tumor itself increased dramatically within three days of treatment, during a period known as "priming." These cells also divided more rapidly. In contrast, the tumors of the animals receiving the ineffective therapy, checkpoint blockade, displayed no such increase in prevalence or proliferation.
Increase in regulatory T cells
Importantly, the researchers also observed an increase in a class of T cells called regulatory T cells in the effectively treated animals during priming. The presence of these cells during tumor rejection was surprising because they have in the past been correlated with a negative prognosis for many tumors.
"Our observation of an increase in the prevalence of these cells in successfully treated tumors runs counter to conventional wisdom and points out the complex nature of immune responses that lead to successful immunotherapy," said Engleman.
Tumor rejection in the effectively treated animals began by day eight. However, in contrast to the priming phase, the researchers observed no differences in the rate of immune cell proliferation in tumors between the two groups of animals during this time. In fact, immune cell proliferation in the tumor ceased altogether by the rejection phase. This finding suggests that, although the initial immune response occurred primarily in the tumor, immune responses in other parts of the body are likely responsible for sustaining the immune attack.
Spitzer and his colleagues observed increases in the number and activity of immune cells in lymph nodes near the tumor during both the priming and rejection phases in the effectively treated animals. Surprisingly, the same types of immune cell increases were seen during the priming and rejection phases in the spleen as well as in lymph nodes that were located a great distance from the tumor. Moreover, the researchers were able to document similar stage-specific changes in the activity and prevalence of immune cells in the peripheral blood.
In particular, a marked increase in a type of memory CD4 T cell was seen in the blood, as well as in peripheral lymphoid organs, during the rejection phase in mice that received effective therapy. This finding is important because the rise in these CD4 T cells may prove useful as an indicator of treatment efficacy in cancer patients who receive different forms of immunotherapy, thus allowing researchers and clinicians to develop a way to accurately monitor the effectiveness of ongoing immunotherapies with a simple, noninvasive blood test. This possibility was supported when the researchers analyzed immune cells in the blood of patients with melanoma who had received immunotherapy. The results showed that a similar subset of CD4 T cells was associated with a positive response.
"The idea would be to use the rise of these CD4 T cells as a biomarker to tailor treatment to each individual," said Engleman. "Physicians could learn quickly whether a therapy is working, or if it should be abandoned in favor of a new approach."
Beyond identifying a potential biomarker of effective therapy, the researchers showed that when the CD4 T cells in successfully treated mice were injected into the tumors of untreated animals, the cells stopped the tumors from growing.
Validating importance of systemic response
The importance of the systemic immune response was validated when the researchers gave the mice a compound that inhibited the ability of immune cells to migrate from secondary lymphoid organs, such as the lymph nodes and spleen, to the tumor site. This intervention allowed sustained tumor growth even in the face of a previously effective treatment.
"In the past, researchers focused on understanding in very minute detail what is happening at the molecular level in immune cells inside the tumor," said Engleman. "But we took an approach that allowed us to zoom out and look at the immune system as a whole. This enabled us to unveil how immune cells work together throughout the body to reject a tumor, and the approach promises to be widely useful in many clinical situations."
In addition to guiding cancer therapy, the researchers also believe the technique could be useful in tracking the changes that occur during an autoimmune disease flare, or to learn more about how the body marshals its forces to fight off an infection.
The work is an example of Stanford Medicine's focus on precision health, the goal of which is to anticipate and prevent disease in the healthy and precisely diagnose and treat disease in the ill.
Materials provided by Stanford University Medical Center. Original written by Krista Conger. Note: Content may be edited for style and length.
Disclaimer: DoveMed is not responsible for the accuracy of the adapted version of news releases posted to DoveMed by contributing universities and institutions.
Primary Resource:
Spitzer, M. H., Carmi, Y., Reticker-Flynn, N. E., Kwek, S. S., Madhireddy, D., Martins, M. M., ... & Fong, L. (2017). Systemic Immunity Is Required for Effective Cancer Immunotherapy. Cell. DOI: 10.1016/j.cell.2016.12.022
Related Articles
Test Your Knowledge
Asked by users
Related Centers
Related Specialties
Related Physicians
Related Procedures
Related Resources
Join DoveHubs
and connect with fellow professionals

0 Comments
Please log in to post a comment.