Biochemical Clues May Predict Who Develops Alzheimer Disease–And Who Doesn’t
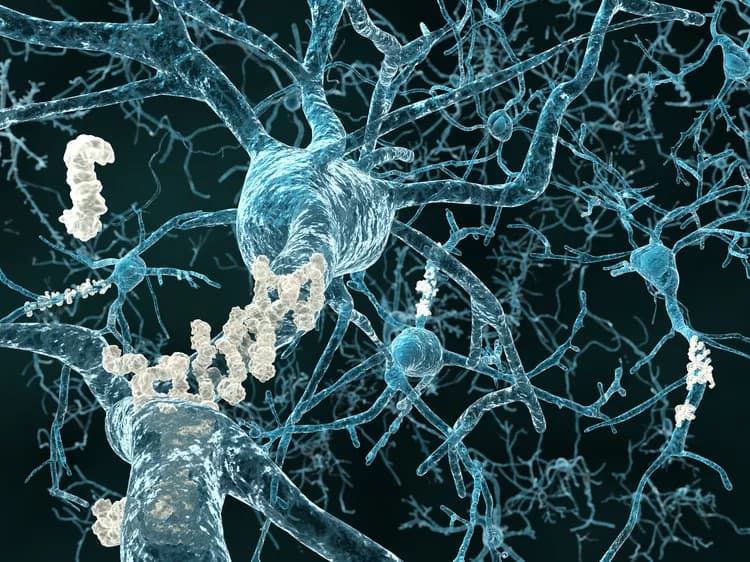
Investigators have wondered why the brains of some cognitively-intact elderly individuals have abundant pathology on autopsy or significant amyloid deposition on neuroimaging that are characteristic of Alzheimer disease (AD). Researchers reporting in The American Journal of Pathology investigated biochemical factors and identified differences in proteins from parietal cortex synapses between patients with and those without manifestation of dementia. Specifically, early-stage AD patients had elevated concentrations of synaptic soluble amyloid-β (Aβ) oligomers compared to controls who were not demented but displayed signs of AD pathology. Synapse-associated hyperphosphorylated tau (p-tau) levels did not increase until late-stage AD.
“Our results suggest that effective therapies will need to target synaptic Aβ oligomers, and that anti-amyloid therapies will be much less effective once synaptic p-tau pathology has developed, thus providing a potential explanation for the failure of amyloid-based trials,” explained lead investigator Karen H. Gylys, PhD, of the UCLA School of Nursing and the Mary S. Easton Center for Alzheimer’s Research at UCLA.
The investigators analyzed brain autopsy samples from different regions in the brain (parietal, superior parietal, entorhinal cortex, and hippocampus) from 46 patients who were classified into groups based on clinical and pathologic criteria: four cognitively-normal elderly controls, two patients with spinocerebellar ataxia type II, 15 patients with no clinical history of dementia but with histopathological signs of AD-related pathology (high-pathology controls), and 24 patients who were clinically demented and histopathologically diagnosed with AD. Patients with early-stage AD were distinguished from those in later stages. Flow cytometry analysis of synaptosomes (resealed nerve terminals) was used to measure the concentrations of two of the biochemical hallmarks of AD, Aβ and p-tau, in synaptic terminals.
Investigators examined whether synaptic Aβ levels were associated with neuritic plaque levels in the parietal cortex. They found little or no evidence of Aβ immunolabeling in either of the control groups but observed a rise in synaptic Aβ concentration associated with increasing neuropathologic disease stages. Synaptic Aβ levels highly correlated with the occurrence of plaque.
Next researchers investigated how Aβ levels are related to clinical dementia. They measured synapse-associated soluble oligomers, known as oAβ in the parietal cortex, levels of which did not correlate with Aβ plaque counts. However, levels of synaptic oAβ in early-stage AD, but not late-stage AD, were significantly elevated relative to both the neuropathologically normal and high pathology groups. “The sharp oAβ elevation in early AD cases suggests that the clinical syndrome of AD dementia may emerge once the level of synapse-associated soluble oligomers exceeds a certain threshold,” noted Dr. Gylys.
Investigators studied the timing of the biochemical changes, noting that other investigators have found evidence that the soluble oligomers of Aβ are the primary toxic peptides that initiate downstream tau pathology as part of the “amyloid cascade hypothesis” of AD. They reported synaptic accumulation of Aβ in the earliest plaque stages, prior to the appearance of synaptic p-tau, which was generally absent until late-stage AD. Aβ and tau levels correlated better in samples from the hippocampus and entorhinal cortex, regions of the brain that are affected earlier in AD than the parietal cortex.
In future work, the authors aim to clarify the precise mechanisms by which soluble Aβ oligomers affect tau and lead to synaptic dysfunction in AD. An intriguing question is whether therapies that slow Aβ oligomer accumulation might delay or even prevent the onset of AD-related dementia. “The correspondence between our human and animal data suggests that this and related animal models will be useful for understanding the progress of synaptic pathology and developing therapies to protect synaptic terminals,” commented Dr. Gylys.
The above post is a redistributed news release provided by The American Journal of Pathology. Note: Materials may be edited for content and length.
Disclaimer: DoveMed is not responsible for the adapted accuracy of news releases posted to DoveMed by contributing universities and institutions.
Related Articles
Test Your Knowledge
Asked by users
Related Centers
Related Specialties
Related Physicians
Related Procedures
Related Resources
Join DoveHubs
and connect with fellow professionals

0 Comments
Please log in to post a comment.