What are the other Names for this Condition? (Also known as/Synonyms)
- AFib (Atrial Fibrillation)
- Cardiac Rhythm Disorder due to Atrial Fibrillation
- Heart Rhythm Disorder due to Atrial Fibrillation
What is Atrial Fibrillation? (Definition/Background Information)
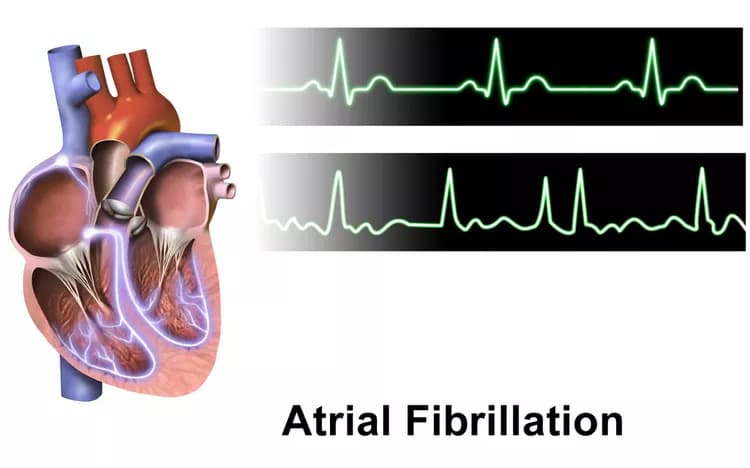
- Atrial Fibrillation (AF or AFib) is the most common and potentially serious heart rhythm disorder usually affecting older adults. The characteristic symptoms associated with this condition are rapid and irregular heartbeat, chest discomfort, and shortness of breath
- High blood pressure, advancing age, structural or functional defects of the heart, excess weight, and alcohol consumption are some known risk factors for the condition. In Atrial Fibrillation, certain erratic impulses (abnormalities in the electrical system of the heart) are generated in the atria. The reception of these chaotic impulses by the ventricles causes inefficient pumping of blood
- Episodes of Atrial Fibrillations can last for variable time periods and are classified according to the following types:
- Intermittent type: In this type, the Atrial Fibrillation may come on and off periodically lasting from a few seconds to hours. It may come back to normal rhythm within 1 week on its own or can progress to a chronic condition
- Chronic type: Here, the condition persists from more than a week (persistent Atrial Fibrillation) to more than a year (permanent Atrial Fibrillation). This type does not resolve on its own and can recur in spite of treatment
- Lone Atrial Fibrillation or Lone AF: This type is seen in individuals who are less than 60 years of age, with generally healthy hearts, and no other risk factors. The reasons for this type of Atrial Fibrillation are not clear
- Atrial Fibrillation constitutes nearly 33% of heart rhythm disorders and can have adverse consequences, such as heart failure or stroke, and increased risk of mortality, if left untreated. Hospitalization, to treat the condition, may be necessary in some cases of AFib
- Atrial Fibrillation is usually managed well with medications. Sometimes, the condition may need a more aggressive therapy with mild electric shock (cardioversion), pacemaker, or surgery (catheter ablation), depending on the severity of symptoms and underlying risk factors
- A healthy lifestyle with regular physical activity, reduced alcohol consumption, and avoidance of smoking are known to help prevent this condition
- The prognosis for Atrial Fibrillation is dependent upon factors that include the individual’s age, the extent of heart disease (if any), and how well the condition is managed
The following subtypes of Atrial Fibrillation are noted:
- Paroxysmal Atrial Fibrillation: Paroxysmal atrial fibrillation is a type of AF where irregular heart rhythm episodes occur sporadically and spontaneously. These episodes can be brief, lasting from seconds to days, and usually resolve on their own without medical intervention. Individuals with this type of AF may experience unpredictable symptoms such as palpitations, chest discomfort, or shortness of breath during episodes
- Persistent Atrial Fibrillation: Persistent atrial fibrillation is characterized by AF episodes that last for more than seven days. Unlike paroxysmal AF, it doesn't self-terminate and may require medical intervention, such as medications or cardioversion (a procedure to restore normal heart rhythm), to achieve a stable rhythm
- Long-Standing Persistent Atrial Fibrillation: This subtype of AF is characterized by continuous episodes of AF that have lasted for more than one year. Individuals with long-standing persistent AF often require more aggressive treatment strategies, which may include catheter ablation (a procedure to eliminate abnormal electrical signals in the heart) or long-term use of medications to manage the condition
- Permanent (Chronic) Atrial Fibrillation: Permanent or chronic atrial fibrillation is a type of AF where the irregular rhythm persists despite attempts to restore a normal rhythm. In these cases, healthcare providers and patients may decide not to pursue further interventions to convert the rhythm back to normal due to various factors, including the patient's overall health and preferences
- Valvular Atrial Fibrillation: Valvular atrial fibrillation is a specific type of AF that occurs in individuals with significant heart valve disease, particularly involving the mitral valve or the aortic valve. Valvular AF often requires more careful management, which may include addressing the underlying valve problem and anticoagulation therapy to reduce the risk of blood clots and stroke
- Nonvalvular Atrial Fibrillation: Nonvalvular atrial fibrillation refers to AF that occurs in the absence of significant heart valve disease. It is the more common form of AF and is typically associated with risk factors such as hypertension, aging, and other medical conditions. Treatment for nonvalvular AF focuses on controlling heart rate and reducing stroke risk
- Acute Onset Atrial Fibrillation: Acute onset atrial fibrillation refers to the sudden and unexpected development of AF. It can occur in response to various triggers, including surgery, infections, or acute medical conditions. Prompt medical evaluation and management are crucial to address the underlying cause and stabilize heart rhythm
- Postoperative Atrial Fibrillation: Postoperative atrial fibrillation is a specific type of AF that occurs after surgery, especially in cardiac surgery or procedures involving the chest or lungs. It is a temporary form of AF that often resolves with medical treatment but requires careful monitoring in the postoperative period due to its potential impact on recovery
Who gets Atrial Fibrillation? (Age and Sex Distribution)
- Atrial Fibrillation affects approximately 0.5% of the world population, according to the World Health Organization (WHO)
- The condition is usually more common in males and the incidence is known to increase with advancing age
- The risk for developing Atrial Fibrillation is 0.1% per year before the age of 40 years. It increases to more than 1.5-2% per year after age 40. After age 40, the lifetime risk is reported to be 26% for men and 23% for women
- A-Fib is relatively more prevalent among Caucasians than individuals of African origin
What are the Risk Factors for Atrial Fibrillation? (Predisposing Factors)
Some risk factors associated with Atrial Fibrillation include:
- Heart-related conditions such as:
- Heart failure
- Sick sinus syndrome: A group of abnormal heart rhythm disorders
- Structural defects and functional heart disease
- Coronary heart disease
- Rheumatic heart disease
- High blood pressure
- Metabolic disorders (including diabetes)
- Excess alcohol consumption
- Smoking
- Excess body weight
- Sleep disorders with snoring
- Stress
- Certain medications (such as steroids)
- Advancing age
- Having family members with Atrial Fibrillation or atrial flutter
It is important to note that having a risk factor does not mean that one will get the condition. A risk factor increases one's chances of getting a condition compared to an individual without the risk factors. Some risk factors are more important than others.
Also, not having a risk factor does not mean that an individual will not get the condition. It is always important to discuss the effect of risk factors with your healthcare provider.
What are the Causes of Atrial Fibrillation? (Etiology)
Atrial Fibrillation is the erratic generation of electrical impulses by the upper chamber of the heart (atria). These chaotic impulses, when received by the lower chambers (ventricles) lead to irregular heartbeats and consequent poor blood flow.
The underlying causes of Atrial Fibrillation may include:
- Heart disease or heart-related conditions that include:
- Increased heart wall thickness
- Heart failure
- Heart attack
- Heart valve defects
- Other structural heart defects
- Infection in the heart
- Tumor affecting the heart
- High thyroid hormone levels; thyroid hormones regulate body metabolism
- Certain triggering factors such as drugs, tobacco, alcohol, caffeine, cocaine, stress, and low hemoglobin (anemia)
- Open surgery of heart
- Morbid obesity
- Disturbed sleep with snoring
- Lung diseases, such as chronic obstructive pulmonary disease (COPD), blood clots in lungs (pulmonary embolism), and elevated pressures in lungs (pulmonary hypertension)
In some cases, the cause of Atrial Fibrillation is unknown.
What are the Signs and Symptoms of Atrial Fibrillation?
The signs and symptoms of Atrial Fibrillation vary from individual to individual. Some individuals may have no symptoms (asymptomatic), while others may have severe and functionally-disabling signs and symptoms. The most common signs and symptoms include:
- Palpitations or irregular hearbeat
- Shortness of breath
- Fatigue
- Exercise intolerance
- Light-headedness
- Sweating
- Confusion
- Loss of consciousness
- Chest pain or chest discomfort
- Low blood pressure
- Rarely, shock and cardiac arrest
How is Atrial Fibrillation Diagnosed?
Since episodes of Atrial Fibrillation can last for variable time periods, with dormant intervals, the diagnosis of this condition depends on having ongoing symptoms. If an individual is in the phase of “dormant” disease, the diagnosis may be difficult.
The main diagnostic tools that aid in the detection of A-Fib include:
- Physical examination by a healthcare professional that includes listening to the heartbeat, checking for blood pressure and pulse rate, and evaluating family history
- Electrocardiography (EKG or ECG)
- Echocardiography to detect structural abnormalities of the heart
- Transesophageal echocardiography is performed in some individuals
- Exercise stress test: To record the heartbeat, blood pressure, and other parameters, while the individual is walking on the treadmill or (exercise) cycling. This is indicative of how well one’s heart works during exercise
- Blood tests: Checking for thyroid hormone level, liver function, kidney function, blood count, and body electrolytes level
- Other tests such as scanning of the heart (echocardiogram) and chest X-ray, may be needed to check for underlying heart disease
- If Atrial Fibrillation is not continuous and happens intermittently (once a while), special monitors such as a Holter monitor, event recorder, or loop recorder may be required
Many clinical conditions may have similar signs and symptoms. Your healthcare provider may perform additional tests to rule out other clinical conditions to arrive at a definitive diagnosis.
What are the possible Complications of Atrial Fibrillation?
Atrial Fibrillation can cause serious complications such as the following:
- Heart failure: Heart’s inability to pump blood efficiently to meet the body’s demands
- Blood clot formation precipitating stroke: One should be aware of stroke warning signs such as facial drooping, arm weakness, and speaking difficulties
Note: In case of an emergency and the listed symptoms are observed, immediately contact your local emergency number (or 911 in the US).
- Side effects from treatment medications
- Uncontrolled or recurrent Atrial Fibrillation in spite of treatment
- Sudden death due to development of ventricular arrhythmia
How is Atrial Fibrillation Treated?
Individuals, who have Atrial Fibrillation without any symptoms or any underlying heart conditions, do not need any treatment. The treatment of Atrial Fibrillation with symptoms has mainly 3 goals as outlined below:
- Controlling the heart rate: Decreasing the rapid heart rate to the optimum level through medications
- Controlling the heart rhythm, which is achieved through:
- Converting irregular heart rhythm to normal rhythm that is mostly attained through medications
- But, some cases may require electric shock therapy (electric cardioversion)
- Minor surgical procedures such as catheter ablation and maze surgery (a type of open heart surgery)
- Or, implanting special devices (pacemaker) inside the heart to achieve regular rhythm
- Prevention of stroke: All types of Atrial Fibrillation classes (intermittent or chronic) have equal risk for stroke, irrespective of duration of episodes. By calculating the CHADS2 SCORE (a scoring system used by healthcare professionals to assess the risk for having a stroke), an individual is advised to start either on aspirin or other powerful blood thinners for stroke prevention
Regular checkups with the healthcare provider at least every 6 months is needed and advised. Some individuals may require more frequent appointments or urgent care to assess the side effects of medications or to evaluate persistent symptoms. Controlling and eliminating the underlying risk factors causing AFib is an important and recognised method of Atrial Fibrillation treatment.
How can Atrial Fibrillation be Prevented?
The preventive measures recommended for Atrial Fibrillation include:
- Healthy lifestyle with regular exercise and heart healthy diet
- Avoidance of smoking, alcohol, excess caffeine, unnecessary medications
- Management of underlying conditions, such as high blood pressure, diabetes, cholesterol, heart failure, heart attack, and thyroid hormone levels
- Managing stress through stress relaxation techniques such as yoga and medication
- Adequate rest and proper sleep
- Regular check up with a healthcare professional or cardiac specialist
What is the Prognosis of Atrial Fibrillation? (Outcomes/Resolutions)
The prognosis of Atrial Fibrillation depends on how well the heart rate and rhythm are controlled by treatment, how effectively the underlying causes responsible for the condition are managed, and modification of one’s lifestyle.
- Without treatment, most cases (except Lone Atrial Fibrillation) can result in serious complications that have the potential to be fatal
- The risk of stroke reduces by 70% when an individual is on blood-thinning medication. However, those who discontinue medication increase their risk of stroke by 5-7% annually
- The prognosis for Lone Atrial Fibrillation which occurs in younger individuals (under 60 years of age) with no associated cardiovascular disease is excellent. Studies have shown that the prognosis in such individuals is comparable to that of the general population
Additional and Relevant Useful Information for Atrial Fibrillation:
Abnormal electrical impulses in Atrial Fibrillation:
- The heart has two upper chambers (right and left atria) and two lower chambers (right and left ventricles)
- Normally, electrical signals responsible for heart contraction initiate in right upper chamber (right atrium) at a specific focal site called the sinoatrial node (SA node) and spread to entire right and left atria
- Then, these impulses are conducted down to the lower chambers (ventricles) at a constant rate, via a bypass connection in between the upper and lower chambers, called the atrioventricular node (AV node)
- In Atrial Fibrillation, this normal pace is lost due to many factors resulting in chaotic impulse formation originating from abnormal and multiple places in the atria other than from the SA node
- So the ventricles receive impulses haphazardly and rapidly leading to ineffective pumping of the heart
In the USA, Atrial Fibrillation reportedly affects between 2-5 million individuals.
Related Articles
Test Your Knowledge
Asked by users
Related Centers
Related Specialties
Related Physicians
Related Procedures
Related Resources
Join DoveHubs
and connect with fellow professionals

0 Comments
Please log in to post a comment.