Chronic Obstructive Pulmonary Disease (COPD)
What are the other Names for this Condition? (Also known as/Synonyms)
- CAFL (Chronic Airflow Limitation)
- CAO (Chronic Airflow Obstruction)
- Chronic Airflow Limitation (COPD)
What is Chronic Obstructive Pulmonary Disease? (Definition/Background Information)
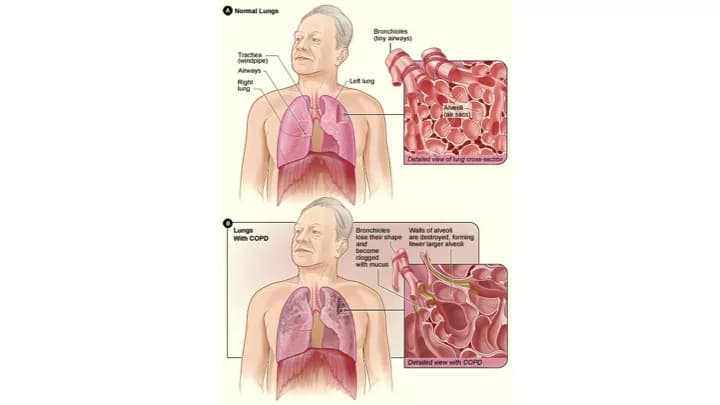
- Chronic Obstructive Pulmonary Disease (COPD) forms a group of conditions that cause severe damage to the lungs, affecting airflow, mainly expiration. These chronic conditions make it difficult for the affected individuals to breathe
- Chronic Obstructive Pulmonary Disease includes the following main conditions:
- Emphysema: Emphysema is a chronic lung condition that is part of a group of diseases known as chronic obstructive pulmonary disease (COPD). It primarily affects the air sacs (alveoli) in the lungs, causing them to become damaged and lose their elasticity. This results in difficulty exhaling air, trapping stale air in the lungs. Emphysema is often caused by long-term exposure to irritants, such as cigarette smoke, and leads to symptoms like shortness of breath, chronic cough, and reduced exercise tolerance
- Chronic Bronchitis: Chronic Bronchitis is another component of COPD. It is characterized by the inflammation and irritation of the bronchial tubes, leading to increased mucus production and persistent cough. This condition typically lasts for at least three months each year for two consecutive years. Chronic bronchitis is primarily caused by exposure to irritants, such as smoking or environmental pollutants, and it leads to symptoms like chronic cough with sputum production and frequent respiratory infections
- Asthma-COPD Overlap Syndrome: Asthma-COPD Overlap Syndrome (ACOS) is a term used to describe a condition where individuals exhibit characteristics of both asthma and COPD. It represents a complex overlap between these two obstructive lung diseases. People with ACOS may have a history of asthma but also display features typically seen in COPD, such as chronic bronchitis or emphysema. Symptoms include shortness of breath, coughing, wheezing, and exacerbations triggered by various factors. ACOS requires a tailored approach to management that combines elements of asthma and COPD treatment
- Individuals with Chronic Obstructive Pulmonary Disease have shortness of breath and cough with sputum/phlegm. The condition is diagnosed by various methods, including physical check-up, with emphasis on lung function
- The type and severity of Chronic Obstructive Pulmonary Disease determines treatment options that may include lifestyle changes, the use of inhalers, oxygen therapy, and medications
- Chronic Obstructive Pulmonary Disease is a chronic and progressive disease that may be managed through lifestyle modifications and the use of medications. In some cases, it may lead to irreversible lung damages. The prognosis of individuals with COPD may vary considerably depending on its severity
Who gets Chronic Obstructive Pulmonary Disease? (Age and Sex Distribution)
- Chronic Obstructive Pulmonary Disease is normally seen in chronic smokers. COPD is more commonly seen among the elderly population, but could be observed in younger individuals, if they start smoking early or if there is a genetic risk for COPD
- It can affect both genders equally
- The occurrence of COPD may be influenced by race, ethnicity, and environmental factors
What are the Risk Factors for Chronic Obstructive Pulmonary Disease? (Predisposing Factors)
The following are generally considered to be the leading risk factors for developing Chronic Obstructive Pulmonary Disease (COPD):
- Smoking, both tobacco and marijuana smoking, is the main risk factor; the affected individuals include primary and secondary smoke inhalers
- Smoking with pre-existing conditions that affect the lungs, such as asthma, or other respiratory disorders (particularly since childhood)
- Environmental factors or bad quality of air such as exposure to toxic chemicals, fumes, or dust, including chronic exposure to smoke from cooking and winter heating in ill-ventilated spaces
- Occupational exposure: Certain jobs related to smoke and dust exposure, such as fire fighters and workers exposed to asbestos and construction dusts
- Age: Since the condition takes years to progress into a chronic stage, COPD is prevalent in older adults, especially individuals who are 65 years and older
- Genetics: Alpha-1 antitrypsin deficiency (AATD) in descendants of Northern European and other populations is known to be a genetic risk factor for COPD
It is important to note that having a risk factor does not mean that one will get the condition. A risk factor increases one's chances of getting a condition compared to an individual without the risk factors. Some risk factors are more important than others.
Also, not having a risk factor does not mean that an individual will not get the condition. It is always important to discuss the effect of risk factors with your healthcare provider.
What are the Causes of Chronic Obstructive Pulmonary Disease? (Etiology)
The following are some of the known/suspected causes of Chronic Obstructive Pulmonary Disease (COPD):
- Smoking: Smoking tobacco is the single most important factor for COPD, accounting for up to 90% of all cases
- Excessive secondhand smoke inhalation
- Smoke inhalation while cooking with burning fuels in poorly-ventilated homes
- Toxic fumes and dust inhalation in factories and other work environments
- Air pollution
- Prior lung damage due to various conditions
- Deficiency in alpha-1 antitrypsin, which is secreted in the liver and renders a protective effect on the lungs. This factor is observed in nearly 1% of the COPD cases
COPD affects the elasticity of the bronchial tubes causing them to generally over-expand and trap air in the lungs following exhalation.
What are the Signs and Symptoms of Chronic Obstructive Pulmonary Disease?
A person with Chronic Obstructive Pulmonary Disease may present with one or more of the following signs and symptoms:
- Difficulty breathing, initially on walking or following less exertion tasks
- One may experience breathing difficulties progressively
- Chronic cough
- Productive cough with sputum; blood in mucus and change in color or thickness of mucus
- Wheezing
- Fatigue
- Lightheadedness
- Cyanosis or blue hue along the lips and nails
- Recurring respiratory infections
- Loss of weight in later stages of the disease
- Headache in the mornings
- Flu-like symptoms including fever
- Slurred speech
Based on the severity and progression of the condition, the healthcare provider may classify COPD as mild, moderate, severe, or very severe.
How is Chronic Obstructive Pulmonary Disease Diagnosed?
A physician may employ the methods below to help diagnose Chronic Obstructive Pulmonary Disease (COPD):
- A thorough physical examination
- Learn about the medical history of the individual
- Smoking history
- Family history of COPD, lung transplant or liver transplant
- Assessment of the presenting signs and symptoms
- Pulse oximetry
- Electrocardiogram (ECG)
- Test for lung function called ‘spirometry’ or pulmonary function testing (PFT)
- Chest X-ray
- CT scan of chest
- Less commonly, computerized axial tomography scan (CAT scan) to check for emphysema and other abnormalities arising from COPD
- Arterial blood gas analysis to check for oxygenated blood and carbon dioxide; a measure of gas exchange
Many clinical conditions may have similar signs and symptoms. Your healthcare provider may perform additional tests to rule out other clinical conditions to arrive at a definitive diagnosis.
What are the possible Complications of Chronic Obstructive Pulmonary Disease?
Chronic Obstructive Pulmonary Disease (COPD) could potentially lead to the following complications:
- Worsening of breathing
- Poor sleep due to shortness of breath
- Depression and anxiety; restlessness
- Poor quality of life: This may develop due to many factors, such as for example, an inability to perform small tasks like getting dressed or participating in simple physical activities
- Frequent respiratory infections and increased susceptibility to common cold and influenza
- Risk for developing pneumonia
- Acute exacerbations, which are worsening symptoms for a few days/weeks, brought on by exposure to inflammatory or infectious triggers
- Increased risk for heart conditions such as hypertension and coronary artery disease
- Pulmonary hypertension, which is increased pressure in the blood vessels of the lungs
- Higher risk of developing lung cancer, in comparison to people without COPD
- Thinning of the bones (osteopenia or osteoporosis) due to repeated steroid use
- Malnutrition with advanced COPD
How is Chronic Obstructive Pulmonary Disease Treated?
A management of Chronic Obstructive Pulmonary Disease may involve lifestyle changes, as well as the use of devices (bronchodilators) and medications to improve the quality of the patient’s life, as below:
- Smoking cessation is the most effective way of slowing COPD progression
- Vaccinations: Pneumococcal vaccine and annual flu shots are recommended, if the individual is not allergic to the same
- Use of bronchodilators to ease breathing and coughing (short-term like albuterol and ipratropium; long-acting ones like salmeterol, formoterol, and tiotropium)
- Use of steroids (which are anti-inflammatory in nature) in either oral or inhaler forms
- A combination of inhaled bronchodilators and steroids
- Antibiotics during exacerbations, especially to treat bacterial lung infections
- Phosphodiesterase -4 (PDE-4) inhibitors in tablet form
- Oxygen therapy in case of low levels of oxygen in blood
- Pulmonary rehabilitation involving therapists for diet, exercise, and counseling for depression and anxiety
- Surgery to remove damaged lung tissue (big air sacs in the lungs)
- In extremely severe cases, a lung transplantation may be required
How can Chronic Obstructive Pulmonary Disease be Prevented?
The prevention of Chronic Obstructive Pulmonary Disease may involve the following:
- Refraining from smoking, as this is an established cause of COPD
- Avoiding polluted environments or wearing personal protective gear when such environment is unavoidable (occupation-related or if it is an occupational hazard)
- Avoid very cold or hot weather
- Exercising regularly
- Eating nutritious food
- Maintaining a healthy body weight
- Breathing exercises
- Drinking plenty of water
- Taking an active role in disease management by regularly keeping appointments, following medications, and therapy regimens
- Taking steps to prevent infections such as washing hands frequently and avoiding individuals with infections
- Consider annual flu shots
What is the Prognosis of Chronic Obstructive Pulmonary Disease? (Outcomes/Resolutions)
It is not possible to reverse the damage to the lungs in Chronic Obstructive Pulmonary Disease (COPD). However, the symptoms can be managed and further damage to the lungs slowed through treatment, preventing exacerbations of COPD. However, the progression of COPD may greatly vary from one individual to another.
- For mild cases of COPD, the prognosis is generally good; the symptoms may be manageable with lifestyle changes and medication use, slowing progression of the disease
- Severe cases of COPD may require life-long medications and treatment
- Individuals with severe COPD especially on home oxygen therapy may be advised to look into end-of-life care decisions. The prognosis in such cases is generally unfavorable
- Home nebulizer machine, pulse oximeter device, home oxygen therapy, and non-invasive ventilation machine for night-time use, may be beneficial depending on the severity of the COPD. It is recommended to discuss these options with a pulmonologist
Additional and Relevant Useful Information for Chronic Obstructive Pulmonary Disease:
The following DoveMed website link is a useful resource for additional information:
Related Articles
Test Your Knowledge
Asked by users
Related Centers
Related Specialties
Related Physicians
Related Procedures
Related Resources
Join DoveHubs
and connect with fellow professionals

0 Comments
Please log in to post a comment.