What are the other Names for this Condition? (Also known as/Synonyms)
- Clot in the Lungs
- Lung Embolism
- Venous Thromboembolism to Lung
What is Pulmonary Embolism? (Definition/Background Information)
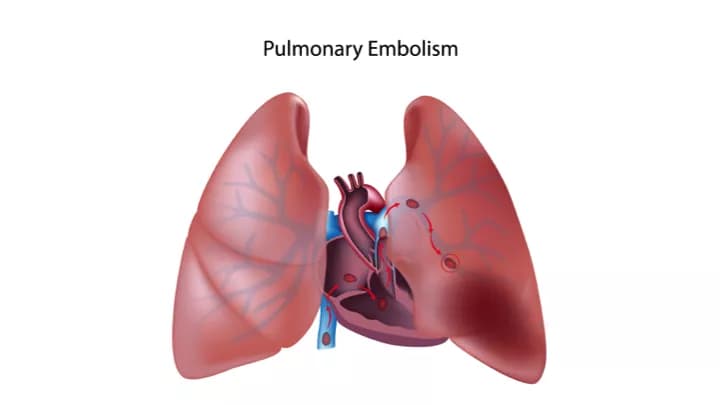
- Pulmonary Embolism is a condition in which one or more of the blood vessels supplying blood to the lungs is/are blocked. It is a life-threatening condition
- It typically occurs when a blood clot from another part of the body is dislodged and gets stuck in the blood vessels of the lung. The usual site of such a blood clot formation, in majority of cases, is thrombosis of the lower legs (a condition called deep vein thrombosis)
- Apart from a blood clot, the blockage can also be caused by fatty tissue, an air bubble, or amniotic fluid, in case of newborns
- Pulmonary Embolism may be diagnosed through blood tests and radiological studies of the lung. The complications due to the condition may include lung collapse, lung infarction, or in severe cases, even death
- The treatment of Pulmonary Embolism includes the use of blood thinners and surgery, if necessary. The prognosis depends upon several factors such as the size of the blood clot (or obstruction), the severity of symptoms, and overall health status of the individual
Who gets Pulmonary Embolism? (Age and Sex Distribution)
- Pulmonary Embolism can occur in otherwise healthy individuals and affect people of all age groups, race, and both genders
- It is very rare in children, but more common in old age and among Afro-American population
- Pregnant women are at an increased risk of Pulmonary Embolism after delivering the baby, for a period of time
- Individuals with some pre-existing diseases or conditions are also at an increased risk for Pulmonary Embolism
What are the Risk Factors for Pulmonary Embolism? (Predisposing Factors)
The majority of individuals with Pulmonary Embolism have one or more of the risk factors at the time of presentation. The following conditions increase the susceptibility of an individual to Pulmonary Embolism:
- Presence of deep vein thrombosis of legs (deep vein thrombosis, or DVT, refers to blood clots deep in the leg veins, away from the skin surface)
- Prolonged immobilization that may take place due to conditions such as a long flight, stroke, or paralysis
- The presence of certain pre-existing conditions such as cancer, longstanding heart disease, and hypertension
- Previous history of pulmonary embolism
- Smoking: Some women smokers taking oral contraceptives and over 35 years old, are especially at risk
- Pregnancy
- Aspiration of amniotic fluid in case of newborns
- Recent surgery
- Obesity
- Fracture of the thigh bone is a risk factor for fat embolism
- Sometimes, in a hospitalized patient, when tubes are placed into the large veins of the neck, the patient might get an air embolism; it is also known as an iatrogenic air embolism
- Deep sea or underwater diving without appropriate decompression (on the way up)
It is important to note that having a risk factor does not mean that one will get the condition. A risk factor increases ones chances of getting a condition compared to an individual without the risk factors. Some risk factors are more important than others.
Also, not having a risk factor does not mean that an individual will not get the condition. It is always important to discuss the effect of risk factors with your healthcare provider.
What are the Causes of Pulmonary Embolism? (Etiology)
- Pulmonary Embolism is most often caused by blood clots that form elsewhere in the body and travel to the lungs
- Rarely, the condition can also be caused by fat globules, air bubbles in blood, or small pieces of tumor that travel to the lungs
What are the Signs and Symptoms of Pulmonary Embolism?
The signs and symptoms of Pulmonary Embolism may develop quite suddenly. Most often, the affected individuals have deep vein thrombosis. Individuals may present with varied symptoms, which may include:
- Difficulty breathing
- Chest pain: Chest pain may become worse on breathing in, exerting, or while coughing
- Cough: It may be a dry cough, or there may be blood in the phlegm, or the cough may contain blood alone
- Cold clammy skin
- Wheezing
- Calf or thigh pain, swelling of the feet with tenderness
- Confusion
- Fainting: Patient with Pulmonary Embolism may faint suddenly or may feel lightheaded
If an individual is ascending from a deep sea dive, the presence of the above symptoms could be due to inadequate decompression.
How is Pulmonary Embolism Diagnosed?
The signs and symptoms of Pulmonary Embolism are highly variable and non-specific and so, testing is essential to establish a definitive diagnosis of the condition.
- Complete physical examination with evaluation of one’s medical history
- Electrocardiogram (ECG): It is a graphical representation of the electrical activity of the heart. It is useful in the diagnosis of Pulmonary Embolism. However, an ECG is not considered specific or sensitive enough to diagnose (or exclude) Pulmonary Embolism.
- D-dimer blood test: It is a blood test used to detect the levels of a substance, d- dimer, which gets elevated in those with Pulmonary Embolism
- Ventilation perfusion scan (or V/Q lung scan): The lungs are imaged after inhalation of a radioactive substance and injection of a radioactive dye into one of the blood vessels. The images can reveal, if any of the arteries in the lungs are blocked
- CT pulmonary angiogram: A dye is injected into one of the veins and then pictures of the chest, using special type of x-rays, are taken. The blockage in any of the arteries can be visualized
- Pulmonary angiography: In this test, a catheter is placed in a large vein in the body and a dye is introduced, which gets into one of the major pulmonary vessels. The dye shows up on an x-ray image, which helps find the site of blockage
Many clinical conditions may have similar signs and symptoms. Your healthcare provider may perform additional tests to rule out other clinical conditions to arrive at a definitive diagnosis.
What are the possible Complications of Pulmonary Embolism?
Pulmonary Embolism is a potentially dangerous condition. It can result in sudden death. Individuals with the condition are at increased risk of getting recurrent embolism. Other complications may include:
- Bleeding inside the lung
- Failure of heart to function effectively (congestive heart failure)
- Respiratory failure, when the patient is unable to maintain the normal amount of oxygen and carbon dioxide (required by the body) through breathing
- Pulmonary hypertension, which is increased pressure in the pulmonary arteries
How is Pulmonary Embolism Treated?
Pulmonary Embolism is a life-threatening condition and patients may require an ICU admission. Depending on their condition, life-supporting measures, such as mechanical ventilation and other supportive care, might be needed. During mechanical ventilation, a patient’s breathing is maintained by a machine, in accordance with the clinical condition of the patient.
Specific treatment measures for Pulmonary Embolism may include the following:
- Medicines which dissolve the clot (or embolus): These medications may be given intravenously (heparin), intramuscularly (lovenox), or orally (warfarin). These medications prevent any further clot formation and dissolve the existing clot/embolus
- Surgery may be required to remove the clot or a catheter may be used (like the one used for a pulmonary angiography)
- Sometimes, individuals with an increased risk of recurrent Pulmonary Embolism, or those who are not suitable candidates for blood-thinning medications might need “inferior vena cava filter”. It is a filter that is put in one of the large veins of the body that carries blood from the lower legs. The filter acts as a sieve and traps any large clots, preventing them from moving up to the lungs
How can Pulmonary Embolism be Prevented?
Some individuals get clots when they have been sitting for too long (such as on a long-distance flight). An effective ways of preventing clots from developing in the deep veins of legs and resultant Pulmonary Embolism is to avoid sitting for a prolonged period of time.
Other methods to prevent Pulmonary Embolism include:
- In patients who are bedridden, use of special type of stockings called compression stockings, to avoid pooling of blood in the deep veins
- Reduce weight (if you are obese or overweight)
- Avoid smoking
- Consult the physician before starting on oral contraceptives
- Undertake careful decompression after an underwater diving (wear proper equipment while scuba-diving)
- Do not skip your blood-thinner medications, which have been prescribed by the healthcare provider
What is the Prognosis of Pulmonary Embolism? (Outcomes/Resolutions)
The outcome of Pulmonary Embolism is highly variable and depends on many factors. While it could lead to sudden death in some patients, in others, there could be a complete resolution of symptoms. There could also be a subset of patients who are asymptomatic.
The outcome is generally poor in patients with the following features:
- Age over 80 years
- History of cancer
- Prolonged heart and lung (cardiopulmonary) disease
- Severe dysfunction of heart and lungs due to the blockage
With reference to the above, the healthcare provider may notice the following parameters:
- Heart rate ≥ 110 beats per minute
- Systolic blood pressure < 100 mm Hg
- Arterial oxygen saturation < 90%
Individuals who do not have (some or any of) the above characteristics generally have a better prognosis.
Additional and Relevant Useful Information for Pulmonary Embolism:
- Deep vein thrombosis (DVT) is a blood clot that occurs in a deep vein of the leg. Most of these blood clots occur in the leg or thigh; though, they may also occur in other parts of the body
The following article link will help you understand deep vein thrombosis:
http://www.dovemed.com/diseases-conditions/deep-vein-thrombosis/
Related Articles
Test Your Knowledge
Asked by users
Related Centers
Related Specialties
Related Physicians
Related Procedures
Related Resources
Join DoveHubs
and connect with fellow professionals

0 Comments
Please log in to post a comment.