What are the other Names for this Condition? (Also known as/Synonyms)
- Dysgerminoma of Ovary
- Female counterpart of Testicular Seminoma
What is Ovarian Dysgerminoma? (Definition/Background Information)
- Ovarian Dysgerminoma is a rare malignant tumor of the ovary that accounts for 2% of all ovarian tumors
- It is a rapidly growing tumor that occurs mostly as a single solid mass. Sometimes, it can also occur as a multiple masses or a combination of solid and cystic masses
- Ovarian Dysgerminoma is associated with dysgenic ovaries in Swyer syndrome, where an individual is a female externally but has XY genotype of a male
- The tumor usually occurs in one ovary. However, in 20% of the cases, especially in ovarian dysgenesis these tumors can affect both the ovaries
- The tumor originates from type of cell in ovary called Germ Cell and belongs to a category of Germ Cell Neoplasm (tumors)
- Ovarian Dysgerminoma is usually present with non-specific sign and symptoms such as:
- Pelvic mass
- Pelvic pain
- Abdominal pain
- Fluid in the abdomen
- The cause of Ovarian Dysgerminoma is mainly unknown. Sometimes the causes may involve:
- Genetic mutations
- The risk factors for Ovarian Dysgerminoma are mainly unknown. However females with Swyers syndrome having an Y chromosome are increased risk of developing Dysgerminoma of the Ovary
- The prognosis of Ovarian Dysgerminoma with prompt and appropriate treatment is excellent
- The treatment for Ovarian Dysgerminoma is
- Chemotherapy
- Surgery
- Radiation
- A combination of Chemotherapy (drugs), Radiation therapy, and surgical procedures
- The complications due to Ovarian Dysgerminoma are
- Metastasis to local and distant organs
- Infertility due to tumor invasion of the ovaries
- Infertility due to radiotherapy or chemotherapy
Who gets Ovarian Dysgerminoma? (Age and Sex Distribution)
- Ovarian Dysgerminoma is the tumor of young individuals and about 90% of the Ovarian Dysgerminomas can occur before the age of 30 years
- The mean average age of occurrence of Dysgerminoma of Ovary is around 22 years
- It can occur worldwide with is no ethnic or racial preference and hence can occur in any race or ethnic group
- Worldwide, no geographical localization of Ovarian Dysgerminoma has been reported
- It is rarely observed in postmenopausal women
- Though Ovarian Dysgerminoma do not usually run within families, rare cases of increased incidence within families, have been reported
What are the Risk Factors for Ovarian Dysgerminomas?
The risk factors for Ovarian Dysgerminoma are unknown in majority of cases. In some individuals the risk factors include:
- Young adult individuals of age group 20 to 30 years are at increased risk.
- Pregnancy: Dysgerminoma of the Ovary is the most common malignant Ovarian Tumor that occurs in pregnant individuals
- Genetic mutations: Studies have found that, currently the females having Y chromosomes are at increased risk of Ovarian Dysgerminoma. In addition the Dysgerminomas of the Ovaries are also associated with:
- Presence of Isochromosome 12p wherein the long arms of both the chromosome 12 are absent and the short arms fuse together to form Isochromosome 12p
- Amplification in the short arm of chromosome 12
- Mutation in the exon region of c-Kit (CD117). But unfortunately the mutation is present in Exon 17 instead of Exon 11 region. If the mutation was present in the Exon 11 of CD117 the tumor could be treated with imatinib
- Family history: Women with a family history of ovarian cancer are at an increased risk
- Having a past diagnosis of breast cancer increase the risk of developing ovarian cancer
- Having a past diagnosis of colorectal cancer increases the risk of developing ovarian cancer
- Having a past diagnosis of endometrial cancer increases the risk of developing ovarian cancer
- High-fat diet may increase the risk. This is not proven definitively
- Smoking: Some studies have shown that long-standing smoking increase the risk
- A weakened immune system (immune-compromised) increase the risk of Ovarian Dysgerminoma
- Family history of Ovarian Dysgerminoma
- Prior history of Chemotherapy for different malignancy
It is important to note that having a risk factor does not mean that one will get the condition. A risk factor increases one's chances of getting a condition compared to an individual without the risk factors. Some risk factors are more important than others.
Also, not having a risk factor does not mean that an individual will not get the condition. It is always important to discuss the effect of risk factors with your healthcare provider.
What are the Causes of Ovarian Dysgerminomas? (Etiology)
The exact cause of Ovarian Dysgerminoma is unknown; however they are thought to occur if the Germ Cells that escape encapsulation from the Ovarian Follicle fail to die. The other causes include:
- Genetic defects like presence Y chromosome in females or presence of isochromosome 12p, amplification in the region of short arm of chromosome 12 and mutations in the exon 17 of CD117
- Individuals with the family history of Ovarian cancers are at increased risk of Dysgerminoma of the Ovary
- Exposure to the following:
- Radiation
- Chemical
- Certain food
- Foreign body
- Pesticides
- Exposure to carcinogens in cigarette smoke
- Prior history of Chemotherapy for different malignancy
- Currently, research is underway to improve our understanding of the Ovarian Dysgerminoma
What are the Signs and Symptoms of Ovarian Dysgerminomas?
There are no specific signs and symptoms of Ovarian Dysgerminoma. But the Ovarian Dysgerminomas present with non-specific presentations that include:
- Abdominal Pain (the pain is usually a Pelvic pain)
- Abdominal Swelling due to the mass or due to fluid accumulation in belly (called ascites)
- Increased Abdominal Girth due fluid accumulation (ascites)
- Persistent feeling of abdominal bloating with nausea or vomiting
- Changes in bowel movements such as Constipation
- Feeling full sooner after a meal (easily having a feeling of Satiety.)
- Loss of appetite with weight loss
- Fatigue (Feeling tired easily)
- Frequent Urination (polyuria) and difficulty while urinating
- Frequent pain during sex (dyspareunia)
- Abnormal menstrual bleeding
- Ovarian Dysgerminoma usually presents as a single mass in the ovary
- Rarely, the tumor can occur as multiple nodules within the same ovary too
- Sometimes, the tumors have been observed to be present at birth
- The nodule is typically are around 10 cm in size (along the larger dimension) at the time of presentation, however some may grow to greater sizes
- The mass is usually well-defined, but sometimes it may be poorly defined
- They are locally aggressive and damage surrounding tissues
- These tumors can be locally aggressive, meaning that the tumor may spread to local areas
- The Ovarian Dysgerminomas may occur as a new growth which develops over weeks to months
How is Ovarian Dysgerminomas Diagnosed?
Ovarian Dysgerminomas are mainly diagnosed by a thorough physical examination and a complete medical history. The diagnosis also involves:
- Pelvic examination
- Complete blood count (CBC) with differential of white blood cells
- Liver function Test (LFT)
- Blood tests called serum tumor markers:
- Elevated Placental Alkaline Phosphatase
- CA-125 test
- Human chorionic gonadotropin (HCG)
- Alpha-fetoprotein (AFP)
- Lactate dehydrogenase (LDH)
- Inhibin
- Estrogen levels
- Testosterone levels
- Exploratory Laparoscopy (Diagnostic laparoscopy): This is a procedure wherein abdomen is examined using a minimally invasive technique. During this procedure a tissue biopsy and tissue for culture. Minimally invasive approach helps decrease complications and decreases the length of stay at hospital. Diagnostic laparoscopy is also helpful in the staging the tumor
- Colonoscopy: A colonoscopy may be performed to assess the extent of tumor spread
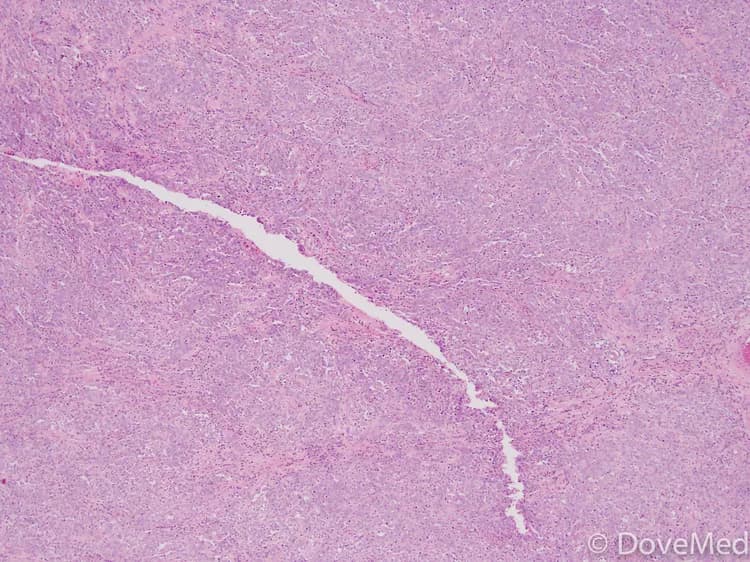
- A tissue biopsy of the tumor: A tissue biopsy is performed and sent to a laboratory for a pathological examination. A pathologist examines the biopsy under a microscope. After putting together clinical findings, special studies on tissues (if needed) and with microscope findings, the pathologist arrives at a definitive diagnosis. Sometimes, the pathologist may perform special studies, which may include immunohistochemical stains, histochemical stains, molecular testing and very rarely electron microscopic studies. Examination of the biopsy under a microscope by a pathologist is considered to be gold standard in arriving at a conclusive diagnosis
- Differential diagnosis, to eliminate other tumor types are often considered, before arriving at a definitive diagnosis
- Genetic testing
- Radiological Imaging studies such as:
- X-Ray of the abdomen and pelvic region
- Barium enema X-ray
- CT scan of the abdomen and pelvic region
- MRI scan of abdomen and pelvic region
- Ultrasound scans of the pelvic region. Usually Transvaginal ultrasonography (TVS) and abdominal ultrasound are performed
- Vascular radiological studies of abdomen and pelvic region
- If the tumor has metastasized then radiological examination to determine the extent of metastasis may be performed. These may include:
- X-Ray of the affected region
- Barium enema X-ray
- CT scan of the affected region
- MRI scan of the affected region
- Ultrasound scans of the affected region
- Vascular radiological studies of the affected region
- Whole body bone scan
- Positron emission tomography (PET) scan or PET/CT scan
Many clinical conditions may have similar signs and symptoms. Your healthcare provider may perform additional tests to rule out other clinical conditions to arrive at a definitive diagnosis.
What are the possible Complications of Ovarian Dysgerminoma?
The main complication of Ovarian Dysgerminoma is infertility due to invasion of ovary by tumor or due to side effect of chemotherapy. The other complications of Ovarian Dysgerminoma may include:
- There may be a rapid growth of the tumor which may invade into surrounding tissue causing tissue damage
- The tumor may recur after surgical excision if incompletely removed
- Deep-seated tumors (those buried in the body tissues), may create problems for adjoining tissues and organs by compressing them (due to mass effect of the tumor)
- Frequent sites of metastasis are the lungs, lymph nodes, liver, and bones
- Blood loss during invasive treatment methods may be heavy
- Inadvertent damage of vital nerves, blood vessels, and surrounding structures during surgery may occur depending on the location of the tumor in the body. Some tumors which are away from the vital organs can be removed usually with no significant damage. However, some tumors may grow close to vital organs and structure which makes the surgical removal difficult and challenging
- Ovarian Dysgerminoma can metastasize to other regions of the body. Extensive metastasis may result in a fatality
- Side effects from chemotherapy (toxicity), radiation therapy
How is Ovarian Dysgerminoma Treated?
The treatment of Ovarian Dysgerminomas depends on the stage of the tumor. The treatment for Ovarian Dysgerminoma includes:
- Chemotherapy: The tumors in early stage that is limited to the ovaries respond excellently to radiotherapy or platinum-based chemotherapy. This is especially important in individuals who like to have children in future
- Surgery
- Radiation
- A combination of Chemotherapy (drugs), Radiation therapy, and surgical procedures
- De-bulking surgery to reduce tumor mass followed by combination of chemotherapy and radiation therapy. The de-bulking procedure helps the chemotherapy treatment to be more effective because there is less tumor mass for the drugs to act on
- The surgery may involve a total abdominal hysterectomy (complete removal of uterus), removal of both ovaries and fallopian tubes (called bilateral salpingo-oophorectomy, omentectomy (removal of fat around the intestines), biopsy of lymph nodes within the abdomen, removal of other tissues in the pelvis and abdomen as needed
- If the tumor is present only in one ovary then, the surgeon may perform a procedure called unilateral salpingo-oophorectomy. In this procedure only the affected ovary and fallopian tube are removed. The uterus is not removed (without a hysterectomy). The other ovary and fallopian tube is also not removed
- But in individuals with Gonadal Dysgenesis both the ovaries are removed, even if there is no tumor in other ovary, because there is very high risk of Dysgerminoma re-occurring in the other ovary
- Removal of tumor as much as possible (called de-bulking procedure) is performed before chemotherapy in advanced stages of tumor
- Chemotherapy before de-bulking procedure or after the de-bulking procedure depending on the individual’s circumstances
- Radiation therapy
- The tumor does not recur after a complete surgical excision
- Complete surgical excision of the tumor is generally considered to be curative
- If the tumors are not completely removed, then they may recur after a period of time. Hence, it is important to completely remove them through surgery
- Embolization (clotting the vessels in the tumor) is used to provide temporary relief from the symptoms, and reduce blood loss during a surgical procedure
- The best treatment practice for Ovarian Dysgerminoma involves a combination of chemotherapy, radiation therapy and/or surgical intervention
- Females who would like have kids can have their ovum cryopreserved, before beginning the treatment
- Post-operative care is important: Minimal activity is allowed, until the surgical wound heals
- Follow-up care with regular screening and check-ups are important
- Your healthcare provider will determine the best course of treatment depending on your individual circumstances
How can Ovarian Dysgerminoma be Prevented?
The cause of Ovarian Dysgerminoma is unknown. Hence, there are no known methods to prevent the tumor occurrence. In general, the following may be considered:
- In individuals having Ovarian Dysgenesis, both the ovaries are prophylactically removed to prevent the re-occurrence of Ovarian Dysgerminoma
- Early diagnosis with close monitoring, and treatment of the tumor is important
- Prompt treatment and early tumor recognition will help in having an optimal outcome
- Genetic testing of the expecting parents (and related family members) and prenatal diagnosis (molecular testing of the fetus during pregnancy) may help in understanding the risks better during pregnancy
- If there is a family history of the condition, then genetic counseling will help assess risks, before planning for a child
- Eliminating the modifiable risk factors helps in the prevention of Ovarian Dysgerminoma
- Currently, there are no specific methods or guidelines to prevent Ovarian Dysgerminoma genetic condition
- Ovarian Dysgerminoma often requires several years of follow up and active vigilance
What is the Prognosis of Ovarian Dysgerminoma? (Outcomes/Resolutions)
The prognosis of Ovarian Dysgerminoma is excellent with treatment, especially in early stages. The prognosis of Ovarian Dysgerminoma also depends upon
- The stage of the tumor
- The type of tumor
- The size of the tumor
- Age of the individual
- Overall health of the individual
- Tumor stage at detection
- Location of tumor
- Number of masses of tumors within the ovary
- Presence of metastasis and the organs involved with metastasis
- Its ki-67 value - a protein found in cells that is a good indicator of how fast the tumor cells are growing. The ki-67 value is determined by a pathologist and is usually mentioned in the pathology report
- Patient’s response to treatment such as chemotherapy
- Patient’s response to treatment such as radiation therapy
Additional and Relevant Useful Information for Ovarian Dysgerminoma:
Below is the link to clinical trials recruiting Ovarian Dysgerminoma patients:
https://clinicaltrials.gov/ct2/results?term=Dysgerminoma&recr=Open
Related Articles
Test Your Knowledge
Asked by users
Related Centers
Related Specialties
Related Physicians
Related Procedures
Related Resources
Join DoveHubs
and connect with fellow professionals

0 Comments
Please log in to post a comment.