What are the other Names for this Condition? (Also known as/Synonyms)
- Childhood Neuroblastoma
- Paediatric Neuroblastoma
- Pediatric Neuroblastoma
What is Neuroblastoma? (Definition/Background Information)
- Neuroblastoma is a type of cancer that is most commonly found in infants and young children. It is the third most common cancer in children after leukemia and brain cancer. Neuroblastoma develops from immature nerve cells of the sympathetic nervous system. The name is derived as “neuro” meaning nerves, and “blastoma” meaning cancer affecting immature (developing) cells
- Neuroblastomas most commonly originate in the adrenal glands, which are located on top of the kidneys. These tumors can also arise in other areas of the body such as the abdomen, neck, chest, spinal cord, or pelvis. Information on the number of cases based on tumor location is provided below:
- Neck (cervical region) - 1-5%
- Pelvic region - 2-3%
- Mediastinum (thoracic region) - 20%
- Retroperitoneal region (abdominal cavity) - 30-35%
- Adrenal glands - 35-40%
- The risk factors for tumor development are not well-established, but may include certain genetic disorders (such as Beckwith-Wiedemann and DiGeorge syndromes) and a positive family history. The cause of Neuroblastoma is believed to be due to genetic factors and several abnormalities have been noted
- The symptoms associated with Neuroblastoma can vary depending on the area of the body affected. Fatigue, loss of appetite, changes in bowel habits, and abdominal pain are commonly observed symptoms. Additionally, the presence of a lump in the affected area, may be noted
- Surgery, chemotherapy, and/or radiotherapy are the options used to treat Neuroblastomas. Factors such as the grade (degree of severity), cytogenetic and molecular features of the tumor, the child’s age, and whether the tumor has spread to other areas, are factors that help decide the best course of treatment to be followed
- The prognosis is generally favorable when Neuroblastomas are detected early and treated appropriately, in cases of small-sized localized tumors with a favorable tumor biology. Presently, no established screening protocols are available for Neuroblastoma
Neuroblastomas may be classified based on their histological features into the following types:
- Low-risk Neuroblastoma: It is mostly found in children younger than 1.5 years and has a favorable prognosis. This tumor observed that infants with this tumor type generally have a curable tumor condition
- High-risk Neuroblastoma: It is mostly found in children older than 1.5 years. The prognosis with this type is generally guarded and only half of the children with this tumor type survive beyond 5 years
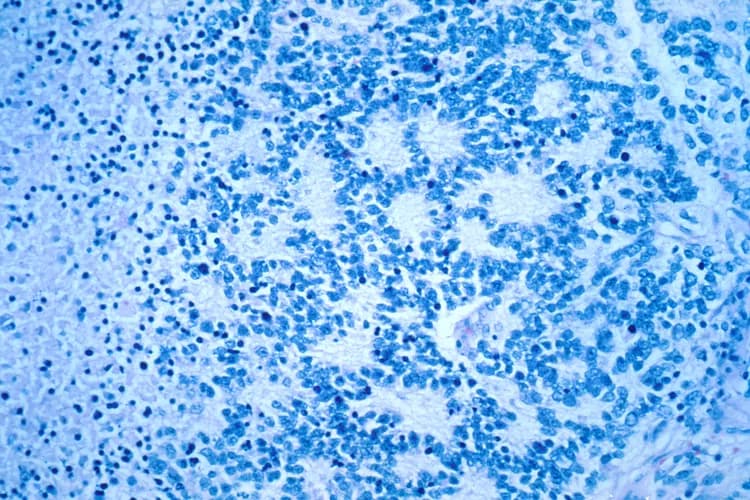
Tissue biopsy of Neuroblastoma is important in designating the tumor based on risk group assessment, which has a bearing on its treatment and prognosis. The histological classification of the tumor is based on the International Neuroblastoma Pathology Classification (INPC).
Who gets Neuroblastoma? (Age and Sex Distribution)
- Neuroblastoma is the most common solid tumor found outside the brain (extracranial tumor) in children. It is one of the most common cancers in children (Pediatric Neuroblastoma), although per se it is a very rare form of malignancy
- The prevalence rate is 1 in 7,000 live births. In children less than 15 years, Neuroblastoma is found at an incident rate of 1 in 100,000 cases (of which 90% are diagnosed in children less than 5 years of age and 37% in infants); 19 months is the median age of diagnosis
- Thus, it occurs mostly in infants and young children under the age of 5 years. In infants, most cases are diagnosed within 30 days. The tumor can occur in older children and adults too. In adults over 20 years, the incidence rate is about 1 in 10 million cases, and the tumor is extremely rare
- The tumor is rarely congenital. In some cases, Neuroblastoma develops before birth, but is usually not detected until later, when the tumor grows and begins to cause certain characteristic symptoms, and/or after it has already spread to other parts of the body
- The tumor is to some extent more common in boys than girls
- Neuroblastoma is seen all over the world; there is no geographical, racial, or ethnic group restriction observed, though Caucasians have a slightly higher prevalence rate (than African Americans)
- Worldwide, more cases are reported from higher-income (developed) countries, in comparison to lower-income (developing/underdeveloped) countries
Note: Children having a family history of the tumor are reportedly diagnosed earlier with Neuroblastomas (average 9 months age at diagnosis). Also, in such children, multifocal primary Neuroblastomas are observed.
What are the Risk Factors for Neuroblastoma? (Predisposing Factors)
The risk factors of Neuroblastoma include:
- Children with a family history of Neuroblastoma may have a higher risk for developing this malignant tumor. However, this factor accounts only for 1-2 % of all Neuroblastomas. A vast majority of children who develop the tumor, do not have a family history of the same
- Association with certain genetic disorders including:
- Neurofibromatosis type 1 (NF1)
- Beckwith-Wiedemann syndrome
- DiGeorge syndrome
- Hirschsprung disease
- Hypoventilation syndrome
The potential risk factors (not definitely proven though) for Neuroblastoma include:
- Exposure to certain chemicals in industries: Researchers believe that the exposure of either parent to occupational chemicals from the electronics industry, farming, or other industries may play a role in its development
- Excessive alcohol consumption
- Smoking
- Infections during early childhood
- Use of certain drugs, medicines during pregnancy
- Hormone use and fertility drugs
- Hair dye application in expectant mothers
It is important to note that having a risk factor does not mean that one will get the condition. A risk factor increases one's chances of getting a condition compared to an individual without the risk factors. Some risk factors are more important than others.
Also, not having a risk factor does not mean that an individual will not get the condition. It is always important to discuss the effect of risk factors with your healthcare provider.
What are the Causes of Neuroblastoma? (Etiology)
Currently, the exact cause of Neuroblastoma is unknown. It has been reported that typically, 98% of the tumors are sporadic, while 2% are familial.
- As with other forms of cancer, Neuroblastoma is observed to develop because of the transformation of normal body cells to abnormal cells, as a result of genetic mutations
- These cancer cells divide uncontrollably, as they lack the mechanism of regulating their growth and division. Ultimately, the accumulation of cells leads to the formation of tumors
- The following genetic abnormalities have been identified as being responsible for Neuroblastoma development:
- ALK gene mutations have been implicated in both the sporadic and inherited forms of Neuroblastoma. ALK gene is involved in three-fourths of the familial cases of Neuroblastoma (germline mutations in ALK gene are associated with hereditary Neuroblastoma)
- PHOX2B gene mutations are rarely noted in Neuroblastoma. However, when this mutation is present (in familial Neuroblastoma), other conditions may coexist, namely congenital central hypoventilation syndrome (Ondine curse) and Hirschsprung disease. Hence, the presence of such mutations should prompt the healthcare provider to screen for these disorders too
- Abnormalities involving chromosomes 1 and 11 (deletion of genetic material) and tumor suppressor genes, such as KIF1B, which are observed in both sporadic and familial Neuroblastomas
- Amplification of MYCN gene (observed in one-fourth of the patients), mostly seen in high-risk tumors
- Other genes that may be involved in tumor formation include the NBPF10 gene
Some tumors, have specific single nucleotide polymorphisms (SNPs, types of genomic variables), that may be either associated with low-risk or high-risk Neuroblastomas.
- High-risk tumors are associated with SNPs in the following genes:
- BARD1 at chromosome 2q35
- LMO1 at chromosome 11p15
- LIN28B at chromosome 6q16
- HACE1 at chromosome 6q16
- CASC15/NBAT-1 at chromosome 6p22
- Low-risks tumors are associated with SNPs in the following genes:
- DUSP12 at chromosome 1q23.3
- DDX4 at chromosome 5q11.2
- IL31RA at chromosome 5q11.2
- HSD17B12 at chromosome 11p11.2
Neuroblastoma starts to form at the embryonic stage of immature nerve cells, called neuroblasts, which are found in tissues.
- Normally, during the developmental process, neuroblasts mature into functioning nerve cells and are typically fully-developed by birth
- However, in the case of Neuroblastoma, the immature neuroblasts do not develop into nerve cells. Instead, they divide and multiply uncontrollably, leading to the formation of a tumor mass (Neuroblastoma)
What are the Signs and Symptoms of Neuroblastoma?
The signs and symptoms of Neuroblastoma vary depending on the site of the body affected, as well as the extent of spread to other areas of the body. The symptoms also arise as a result of the growing tumor pressing on the adjoining or surrounding tissues. The initial symptoms observed are irritability, loss of appetite, weight loss, and fatigue.
The origin of Neuroblastoma, in many cases, is in the adrenal glands and the tissues of the sympathetic nervous system. The tumor may be found anywhere from the neck region to the pelvic region. The signs and symptoms in both young children and adolescents are mostly the same.
The common signs and symptoms of Neuroblastoma include:
- An unusual lump in the abdomen, neck, or chest
- Abdominal pain; it is the most common symptom observed
- Swollen stomach
- Dark circles or bruises around the eyes
- Painless bluish lumps underneath the skin
- Chest or back pain
- Wheezing, difficulty breathing
- Drooping eyelids, unequal pupil size
- Fever
- Bulging eyes (proptosis)
- Easy bruising
- Bone pain or soreness
- Paleness
- Swelling in the legs
- Changes in bowel habits, including diarrhea or constipation
- Problems with urination
- Paralysis or inability to move a body part
Most commonly, Neuroblastomas are seen to arise in the adrenal glands. Occasionally, they may also arise in sites such as the chest, neck, abdomen, pelvic region, or the spinal cord. Older children are more often diagnosed with Neuroblastoma arising from the retroperitoneal and pelvic region, while more infants are diagnosed with tumors that arise in the neck and chest region.
How is Neuroblastoma Diagnosed?
Before diagnosing an individual with Neuroblastoma, a physician will first review the individual’s medical history including family history, and also conduct a thorough physical examination. Additional tests may be performed to help confirm the diagnosis and to determine the location and size of a tumor. These may include:
- Urine and blood tests: These tests may provide information on the causes of the symptoms experienced by the individual. Blood and urine tests can detect high levels of homovanillic acid (HVA) and vanillylmandelic acid (VMA), both catecholamine metabolites, made by the Neuroblastoma cells. Lab tests may also show decreased sodium levels (hyponatremia)
- Imaging tests: Imaging tests help in detecting a mass, which may suggest the presence of a tumor. These tests include X-ray, computerized tomography (CT), positron emission tomography (PET), ultrasound, and magnetic resonance imaging (MRI) scans. Imaging tests are also helpful to determine the spread of the tumor, which can help determine the best course of treatment to be followed. Rarely, Neuroblastoma is detected prenatally through a fetal ultrasound
- Iodine-123 metaiodobenzylguanidine scan (123-I-MIBG): In a MIBG scan, a radioactive substance is injected into blood, which will then bind to the Neuroblastoma cells. This test helps in determining whether the tumor has spread to other regions of the body or not
- Tissue biopsy: If a mass is found, the physician may have a sample of the tissue removed and sent to the laboratory for a histopathological examination. A pathologist will examine the biopsy under a microscope. After putting together clinical findings, special studies on tissues (if needed) and together with microscope findings, the pathologist arrives at a definitive diagnosis
- The pathologist may also request cytogenetic and molecular studies (for example N-myc) to determine genetic features of the cancerous cells, which is crucial in developing the most appropriate treatment plan for the affected individual
- Bone marrow biopsy: It may be helpful in determining tumor staging
Many clinical conditions may have similar signs and symptoms. Your healthcare provider may perform additional tests to rule out other clinical conditions to arrive at a definitive diagnosis.
What are the possible Complications of Neuroblastoma?
The possible complications from Neuroblastoma include:
- Metastasis (spread) of the tumor to other areas of the body, such as the bones, lymph nodes, liver, orbit, and skin, leading to functional and/or anatomical derangement of the affected organ
- Swollen abdomen and breathing difficulties may be noted, when the tumor has metastasized to the liver
- Bone marrow metastasis can cause decreased blood cell count (pancytopenia)
- Skin nodules present bluish discoloration, when skin is involved through metastasis
- Spread of tumor to the orbit (orbital metastasis) can result in eye-related symptoms
- In adolescents, bone marrow metastasis is uncommon (unlike in young children), while spread of malignancy to the brain and lung is more common (which is generally not seen in young children though)
- Children with cancer spread generally show anemia, high blood pressure, and fever
- It is reported that nearly 80% of the cases in children over 10 years present with metastasis, at the time of diagnosis
- Spinal cord compression is another potential complication associated with Neuroblastoma located on the spine. As the tumor grows, it can press upon the spinal cord leading to paralysis of the arms/legs and pain
- Some tumors can secrete vasoactive intestinal peptide (VIP) hormone causing severe (watery) diarrhea that is also noted with chemotherapy
- Tumors in the neck can cause Horner’s syndrome that consists of contracted pupil (myosis), drooping eyelid (ptosis), decreased sweating (anhidrosis), depression of eye ball (or enophthalmos, which occurs due to compression of nerves)
- Side effects of chemotherapy and/or radiotherapy
Neuroblastomas may have the ability to secrete hormones, which can affect distant ‘normal’ body tissues and cause symptoms. This can lead to a condition known as paraneoplastic syndrome. Paraneoplastic symptoms are rare in children; but, it can result in permanent neurological damage.
The symptoms of paraneoplastic syndromes include:
- High blood pressure and/or rapid heartbeat
- Reddening of the skin
- Sweating
- A rare paraneoplastic syndrome that affects children with Neuroblastoma is called opsoclonus-myoclonus-ataxia. It is characterized by rapid eye movement (dancing eyes) and difficulty in coordination (dancing feet). Tumors associated with opsoclonus/myoclonus syndrome are known to have favorable prognosis
How is Neuroblastoma Treated?
Once a diagnosis of Neuroblastoma has been established, the extent to which the tumor has spread is assessed, known as staging. The system used to stage Neuroblastoma is the International Neuroblastoma Staging System (INSS), which is as follows:
- Stage 1: Localized tumor confined to the area of origin
- Stage 2A: Unilateral tumor with incomplete gross resection; identifiable ipsilateral and contralateral lymph node negative for tumor
- Stage 2B: Unilateral tumor with complete or incomplete gross resection; with ipsilateral lymph node positive for tumor; identifiable contralateral lymph node negative for tumor
- Stage 3: Tumor infiltrating across midline with or without regional lymph node involvement; or unilateral tumor with contralateral lymph node involvement; or midline tumor with bilateral lymph node involvement
- Stage 4: Dissemination of tumor to distant lymph nodes, bone marrow, bone, liver, or other organs except as defined by Stage 4S
- Stage 4S: Age <1-year-old with localized primary tumor as defined in Stage 1 or 2, with dissemination limited to liver, skin, or bone marrow (less than 10% of nucleated bone marrow cells are tumors)
The majority of Neuroblastoma cases require some form of treatment. The type of treatment required is dependent on several factors, which include:
- The child’s age
- Stage of cancer (whether the tumor has spread to other areas of the body)
- Microscopic and genetic characteristics of the tumor
With this information, the healthcare provider may be able to classify the cancer as low-risk, intermediate-risk, or high-risk. The combination of treatment options is determined by the risk category and may include:
Surgery:
- Surgery can be used to remove the tumor. The size and location of the tumor can influence whether the tumor can be removed completely
- In low-risk patients, surgery may be the only treatment method needed
- Surgically removing tumors in close proximity to vital organs, such as the lungs, may be associated with complications
In individuals categorized as intermediate-risk, additional treatment options, including chemotherapy may be necessary following the removal of tumor.
In individuals categorized as high-risk, the treatment options, such as chemotherapy, radiation therapy, stem cell transplantation, biological therapy, and immunotherapy, may be necessary following the surgical removal of tumor.
Chemotherapy:
- Chemotherapy uses drugs to kill cancer cells or prevent their further growth
- While chemotherapy is utilized to target cancerous cells, it can also cause damage to healthy, normal cells in the body, resulting in side effects
Radiation therapy:
- Radiation therapy uses high-energy waves, such as X-rays, to kill the cancer cells
- This type of treatment may be beneficial for children with low-risk and intermediate-risk Neuroblastoma, especially if surgery and chemotherapy have not proved to be helpful
- For high-risk Neuroblastoma, radiation therapy may be used following surgery and chemotherapy, to prevent the cancer from returning
Autologous stem cell transplant:
- This type of treatment, along with intensive chemotherapy, may be useful with high-risk Neuroblastomas
- In this procedure, the individual’s blood stem cells are collected and stored. Following this, high doses of chemotherapy drugs are then administered to destroy the cancerous cells
- After the chemotherapy treatment, the stored stem cells are then injected into the child to allow the formation of new blood cells
Immunotherapy:
- Immunotherapy drugs are used to enhance the body’s immune system and its ability to defend against cancerous cells
- Individual’s with high-risk conditions may undergo immunotherapy to increase the immune system’s fight against the Neuroblastoma cells
Note:
- Newer therapies include biological therapy (using isotretinoin) and antibody therapy (using cytokine proteins) have been used in the treatment
- ALK kinase inhibitors are helpful in treating recurrent tumors and those tumors that do not respond to treatment (refractory Neuroblastoma)
- Treatment may be undertaken for symptoms, such as spinal cord compression (causing paralysis) and severe diarrhea
- Appropriate therapy is necessary following surgery, to recover from neurological symptoms caused by the tumor
Observation: In some rare cases, Neuroblastoma may disappear on its own, without any treatment. Therefore, sometimes, the physicians may use what is known as “watchful waiting” before planning ahead with treatment options.
How can Neuroblastoma be Prevented?
Current medical research has not established a method of preventing Neuroblastoma.
- Cancer screenings are important tests in that they can detect cancer in its earliest stages, which would help optimize treatment efforts. Nevertheless, currently, there are no standardized screening tests for Neuroblastomas
- Regular medical screening at periodic intervals with blood tests, imaging scans, and physical examinations, are mandatory for those who have already had the tumor removed or destroyed. This is because Neuroblastomas have a high metastasizing (spreading capacity) potential and the possibility of recurrence
In general, preventive methods for cancers include reducing contributory risk factors, such as:
- Smoking
- Unhealthy diet and lifestyle
- Obesity
- Exposure to toxins
- Unnecessary medication
What is the Prognosis of Neuroblastoma? (Outcomes/Resolutions)
The prognosis for Neuroblastoma can vary from one child to another and is dependent on a set of several factors that include:
- Age of the child
- Location of the tumor
- The physical and genetic characteristics of the tumor cells (including histological type of tumor)
- Stage of the tumor: With lower-stage tumors, when the tumor is confined to the site of origin, the prognosis is usually better with appropriate therapy. In higher-stage tumors, such as tumors with metastasis, the prognosis is poor
- Response to treatment: Tumors that respond to treatment have better prognosis compared to tumors that do not respond to treatment
- Involvement of the regional lymph nodes (in children older than 12 months): Metastasis to the regional lymph nodes on the same side as the tumor, does not alter the prognosis and does not make the tumor a higher stage tumor. In contrast, involvement of regional lymph nodes on the opposite side of the tumor, worsens the prognosis and upstages the tumor
Neuroblastoma is curable in some cases. Often times, there is a favorable response to treatment, if the cancer has not already spread. Children diagnosed before the age of 12 months, most of the times, see a more successful outcome.
Disease-free survival factors for Neuroblastoma include the following:
- Neuroblastoma that is confined to the site of tumor origin (showing absence of metastasis) in children of any age
- Advanced stage tumor in children younger than 1.5 years with histologically favorable tumor
Prognosis based on primary tumor site:
- Adrenal gland primary tumors have a higher likelihood for unfavorable Neuroblastoma, along-with MYCN gene abnormalities. Many adrenal gland tumors are diagnosed at advanced stages (stage 4), have unfavorable tumor histology, and are seen in children of age less than 18 months
- Tumors in the thoracic region had better prognostic values. Study reports indicate fewer recurrences and fatalities; also, MYCN gene abnormalities are observed in lesser number of cases
- Multiple primary tumors (multifocal tumors) that are seen in infants, typically show good prognosis, in many cases. Many such tumors may show positive family history and ALK gene mutations
The factors that point to a poor prognosis include:
- Age of tumor onset beyond 18 months
- Advanced stage of tumor (including metastasis)
- Presence of N-myc oncogene mutation: Tumors showing MYCN gene amplification have unfavorable histology
- Deletion of genetic material on the short arm (p) of chromosome 1
- Unfavorable Shimada histology index (a classification index for Neuroblastomas)
In children less than 1 year, the 5-yr survival rate is 95%; while in children between 1-14 years, it is 68%. The overall 5-year survival rate is 71%, considering children of all ages. It has also been reported that:
- All individuals over age 10 years (adolescents, young and old adults) have worse long-term overall prognosis, independent of tumor stage or location
- Older children with advanced stage of tumor have among the worst prognosis, when compared to young children
- Neuroblastoma tumors in a newborn child and those diagnosed in the fetal stage have similar prognosis to Neuroblastoma tumors in older children (over 18 months of age), when tumor type with similar histological features are compared
- Most tumors reported in Afro-Americans belong to high-risk group and portray poorer prognosis (lower survival rates) in comparison to tumors reported in Caucasians, even though more number of Neuroblastoma cases are reported among the Caucasian race
As with any tumor, it is important to have follow-up appointments with a physician to monitor for any returning tumors. Close monitoring in children after surgery, to watch out for long-term treatment side effects (such as from chemotherapy) is essential and is recommended.
Additional and Relevant Useful Information for Neuroblastoma:
In some studies, spontaneous regression of Neuroblastoma, without treatment, has been described. Studies inform that such regression has been occasionally observed in tumors having the following criteria:
- Almost triploid number (3 sets) of chromosomes
- Absence of MYCN gene amplification
- There is no loss of genetic material on the short arm (p) of chromosome 1
However, further studies are necessary to understand this phenomenon.
Please visit our Cancer & Benign Tumors Health Center for more physician-approved health information:
Related Articles
Test Your Knowledge
Asked by users
Related Centers
Related Specialties
Related Physicians
Related Procedures
Related Resources
Join DoveHubs
and connect with fellow professionals

0 Comments
Please log in to post a comment.