What are the other Names for this Condition? (Also known as/Synonyms)
- Embryonal RMS of Vagina
- Vaginal Embryonal Rhabdomyosarcoma
- Vaginal ERMS
What is Embryonal Rhabdomyosarcoma of Vagina? (Definition/Background Information)
- Rhabdomyosarcoma of Vagina is a very uncommon, high-grade malignant tumor of the vagina. It typically affects very young girls (mostly below age 2 years)
- The rhabdomyosarcoma (RMS) is an infrequent, but malignant ‘skeletal muscle’ tumor of the soft tissues. RMS tumors are poorly-defined, fleshy, expanding masses that form deep within the body tissues, or below the skin surface
- There are 3 types of rhabdomyosarcomas including the embryonal, alveolar, and pleomorphic subtypes. Embryonal Rhabdomyosarcoma (ERMS) of Vagina is the most common histological subtype of vaginal rhabdomyosarcoma
- Currently, there are no specific risk factors identified for Embryonal Rhabdomyosarcoma of Vagina. However, RMS may be associated with certain genetic disorders including Beckwith-Wiedemann syndrome, Costello syndrome, and neurofibromatosis type 1, among others
- The cause of formation of Embryonal Rhabdomyosarcoma of Vagina is not well-established. It is believed to occur due to certain genetic mutations
- The signs and symptoms of Vaginal Embryonal Rhabdomyosarcoma include the presence of a fleshy mass in the vagina. Due to this, an early detection of the tumor is generally enabled
- The treatment of Embryonal Rhabdomyosarcoma of Vagina is undertaken through surgery and/or chemotherapy. The prognosis of ERMS depends on many factors including the stage of the cancer and one’s response to therapy
Who gets Embryonal Rhabdomyosarcoma of Vagina? (Age and Sex Distribution)
- Embryonal Rhabdomyosarcoma of Vagina is a rare and invasive tumor affecting very young girls, less than 5 years old (infants and very young children); the average age is around 1.8 years
- Over 90% of Embryonal RMS of Vagina is seen in children below the age of 5 years. Occasionally, the tumor is known to affect young adult women
- No racial or ethnic preference is generally noted
What are the Risk Factors for Embryonal Rhabdomyosarcoma of Vagina? (Predisposing Factors)
Currently, no specific risk factors are noted for the development of Embryonal Rhabdomyosarcoma of Vagina. But, in general, rhabdomyosarcomas may be associated with the following factors:
- Family history of the condition has been observed, though very rarely
- Use of drugs, such as cocaine or marijuana, by the parent mother
- Carcinogens (some have been found on mice and certain types of fish)
- Beckwith-Wiedemann syndrome
- Costello syndrome
- Li-Fraumeni syndrome
- Neurofibromatosis (type) 1
- Noonan syndrome
It is important to note that having a risk factor does not mean that one will get the condition. A risk factor increases ones chances of getting a condition compared to an individual without the risk factors. Some risk factors are more important than others.
Also, not having a risk factor does not mean that an individual will not get the condition. It is always important to discuss the effect of risk factors with your healthcare provider.
What are the Causes of Embryonal Rhabdomyosarcoma of Vagina? (Etiology)
The exact cause and mechanism of formation of Embryonal Rhabdomyosarcoma of Vagina is unknown.
- A majority of the vaginal rhabdomyosarcomas are of the embryonal variant, which are thought to arise from embryonic connective tissues responsible for skeletal muscle development
- It is suspected that either inherited genetic defects or de novo (sporadic and spontaneous) genetic mutations may be the causative factors
- Chromosomes 2, 8, and 11 have been found to be altered, indicating complex mutations with gain/loss of genetic material. Also, an absence or modification of tumor suppressor gene has been observed. These changes are said to be responsible for ERMS; but the exact process how the tumor develops, is not clearly understood
What are the Signs and Symptoms of Embryonal Rhabdomyosarcoma of Vagina?
The signs and symptoms of Embryonal Rhabdomyosarcoma of Vagina may include:
- Presence of fleshy (grape-like) polyps or infiltrative mass in the vagina
- Large masses can protrude into the vaginal canal and be externally visible in some cases
- The tumor may appear fluid-filled (edematous)
- In some cases, the skin over the mass may ulcerate and result in bleeding
- Vaginal bleeding is known to occur from large mass size
- Frequent urination due to compression/pressure of the tumor
- If the urinary bladder is involved, then it may obstruct the bladder and lead to retention of urine
- Pain in the pelvic or abdominal region
- Lower back pain
How is Embryonal Rhabdomyosarcoma of Vagina Diagnosed?
The following tools may be used towards establishing a diagnosis of Embryonal Rhabdomyosarcoma of Vagina:
- Evaluation of the individual’s medical history and a thorough physical (pelvic) examination
- Transvaginal ultrasound of the uterus can provide an image of the vagina and surrounding pelvic organs
- MRI scans can be used to observe if a vaginal tumor has the characteristics of cancer, along with visualizing the cancer spread (if it has spread to other areas)
- Plain radiographs of the chest can provide evidence if the tumor has spread to the lungs
- CT scans are rarely used in diagnosing vaginal cancer, but can be used to determine if metastasis has occurred
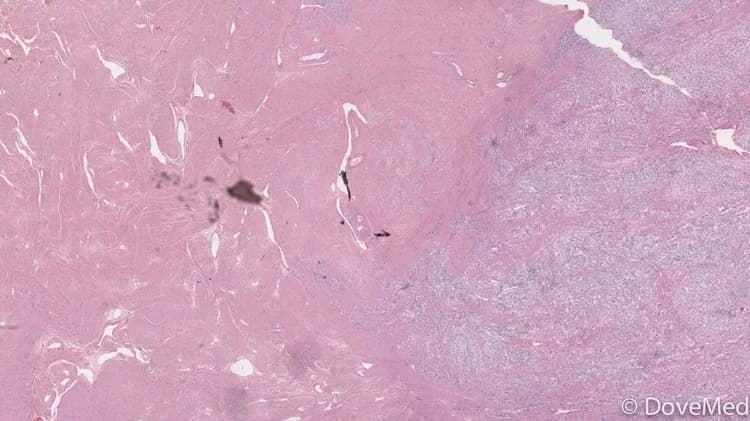
- A vaginal biopsy may be necessary to determine, if the tumor present is a rhabdomyosarcoma, or a different soft tissue sarcoma. In the tissue biopsy procedure, the physician removes a sample of the tissue and sends it to the laboratory for a histopathological examination. The pathologist examines the biopsy under a microscope and arrives at a definitive diagnosis after a thorough evaluation of the clinical and microscopic findings, as well as by correlating the results of special studies on the tissues (if required)
Many clinical conditions may have similar signs and symptoms. Your healthcare provider may perform additional tests to rule out other clinical conditions to arrive at a definitive diagnosis.
What are the possible Complications of Embryonal Rhabdomyosarcoma of Vagina?
Complications due to Embryonal Rhabdomyosarcoma of Vagina could include:
- Metastasis of the tumor to other sites in the body
- Recurrence of the tumor after surgery, when the entire tumor is not removed
- Side effects of chemotherapy (such as toxicity) and radiation
- Sexual dysfunction can take place as a side effect of surgery, chemotherapy, or radiation therapy, later in life
- Recurrence of the cancer following incomplete surgical removal is known to be frequent; recurrence is commonly observed in the pelvic region
How is Embryonal Rhabdomyosarcoma of Vagina Treated?
Once a diagnosis of vaginal cancer has been made, the extent to which the tumor has spread is assessed, known as staging. The staging for vaginal cancer is based upon the FIGO (International Federation of Gynecology and Obstetrics) and the AJCC (American Joint Committee on Cancer) TNM staging systems.
The TNM classification for vaginal cancer is given below:
Tumor extent (T):
- Tis: Cancer cells are only in the most superficial layer of cells of the vagina without growth into the underlying tissues. This stage is also called carcinoma in situ (CIS) or vaginal intraepithelial neoplasia 3 (VaIN 3). It is not included in the FIGO system
- T1: The cancer is only in the vagina
- T2: The cancer has grown through the vaginal wall, but not as far as the pelvic wall
- T3: The cancer is growing into the pelvic wall
- T4: The cancer is growing into the bladder or rectum or is growing out of the pelvis
Lymph node spread of cancer (N):
- N0: The cancer has not spread to lymph nodes
- N1: The cancer has spread to lymph nodes in the pelvis or groin (inguinal region)
Distant spread of cancer (M)
- M0: The cancer has not spread to distant sites
- M1: The cancer has spread to distant sites
Stage grouping: Once the T, N, and M categories have been assigned, this information is combined to assign an overall stage in a process called stage grouping. The stages identify tumors that have a similar outlook and are treated in a similar way.
Stage 0 (Tis, N0, M0):
- In this stage, cancer cells are only in the top layer of cells lining the vagina (the epithelium) and have not grown into the deeper layers of the vagina
- Cancers of this stage cannot spread to other parts of the body
- Stage 0 vaginal cancer is also called carcinoma in situ (CIS) or vaginal intraepithelial neoplasia 3 (VaIN 3)
- This stage is not included in the FIGO system
Stage I (T1, N0, M0):
- The cancer has grown through the top layer of cells but it has not grown out of the vagina and into nearby structures (T1)
- It has not spread to nearby lymph nodes (N0) or to distant sites (M0)
Stage II (T2, N0, M0):
- The cancer has spread to the connective tissues next to the vagina but has not spread to the wall of the pelvis or to other organs nearby (T2)
- The pelvis is the internal cavity that contains the internal female reproductive organs, rectum, bladder, and parts of the large intestine
- It has not spread to nearby lymph nodes (N0) or to distant sites (M0)
Stage III - either of the following:
- T3, any N, M0:
- The cancer has spread to the wall of the pelvis (T3)
- It may (or may not) have spread to nearby lymph nodes (any N), but it has not spread to distant sites (M0)
OR
- T1 or T2, N1, M0:
- The cancer is in the vagina (T1) and it may have grown into the connective tissue nearby (T2)
- It has spread to lymph nodes nearby (N1), but has not spread to distant sites (M0)
Stage IVA (T4, Any N, M0):
- The cancer has grown out of the vagina to organs nearby (such as the bladder or rectum) (T4)
- It may or may not have spread to lymph nodes (any N)
- It has not spread to distant sites (M0)
Stage IVB (Any T, Any N, M1):
- Cancer has spread to distant organs such as the lungs (M1)
(Source: “The FIGO/AJCC system for staging vaginal cancer”; information provided by the American Cancer Society, February 2016)
Rhabdomyosarcoma of vagina is treated using several methods depending on the stage of the cancer. A specialist team of healthcare providers may be involved in treating the child. The treatment options may include the following measures:
- If the tumor can be surgically removed with minimal damage and mutilation of the genitalia, then a conservative surgery is attempted. Otherwise, a combination of radiation and chemotherapy may be administered to shrink and confine the tumor, before invasive procedures are sought
- Following a surgical excision and tumor removal, a dose of chemotherapy and/or radiation therapy may be administered to kill any remaining cancer cells
- Radiation therapy and chemotherapy may be necessary if the spread of the cancer to distant sites is noted
- Advanced stage tumors with metastasis may be treated on a case-by-case basis; often symptomatic treatment with radiation and/or chemotherapy is attempted
- Very infrequently, in order to treat the more aggressive tumors, a combination of stem cell transplant with chemotherapy (high-dose) may be necessitated
The treatment of Embryonal Rhabdomyosarcoma of Vagina involves surgery, which is the most common treatment option considered.
Surgery:
- Vaginectomy: It is the surgical removal of a part of the vagina (called partial vaginectomy), or the entire vagina (called total vaginectomy), or the vagina and its surrounding affected structures/tissues may also be removed (called radical vaginectomy)
- Radical trachelectomy: The surgeon removes the cervix, upper part of the vagina, and nearby lymph nodes, while preserving the ability to have children (in future)
- Pelvic exenteration: The entire vagina, the surrounding tissues, and the pelvic lymph nodes are removed. In addition, depending on the extent of tumor spread, parts affected around the region (such as the cervix, uterus, rectum, colon, etc.) may be removed. Recovery from this surgery usually takes a long period
- Arterial embolization may be used to provide temporary relief from the symptoms, and reduce blood loss during a surgical procedure
Chemotherapy:
- Medications are used to kill the tumor cells, which may be given as oral pills or injected into veins
- A combination of chemotherapy medications may be used
- Chemotherapy may be used in addition to radiation and/or surgery, to treat cancers that have spread or recurred. When chemotherapy and radiation therapy are used together, it is called concurrent chemoradiation
- Side effects of chemotherapy may include nausea, vomiting, hair loss, loss of appetite, diarrhea, fatigue, increased risk of infection, mouth sores, and easy bruising, depending on the drugs used
Radiation therapy:
- This procedure uses high-energy beams to kill the cancer cells
- These beams may be delivered from outside the body (external beam radiation therapy) or the radioactive material maybe placed inside the vagina (internal radiation therapy or brachytherapy)
- Possible side effects may include:
- Fatigue, nausea, vomiting, and diarrhea
- Bladder irritation, leading to inflammation (cystitis)
- Ovaries may be affected resulting in menstrual changes, or premature menopause
- The vulva and vagina may be affected, causing soreness, or even scar tissue formation
Post-operative care is important and one must maintain minimum activity levels, until the surgical wound heals. Follow-up care with regular screening and check-ups are important and encouraged.
How can Embryonal Rhabdomyosarcoma of Vagina be Prevented?
- Current medical research has not established a way of preventing the formation of Embryonal Rhabdomyosarcoma of Vagina
- Genetic counseling and testing: If there is a family history of the condition, then genetic counseling will help assess risks, before planning for a child
- Due to its high metastasizing potential and recurrence rate, regular medical screening at periodic intervals with blood tests, scans, and physical examinations, are mandatory for those who have already been treated for this tumor
What is the Prognosis of Embryonal Rhabdomyosarcoma of Vagina? (Outcomes/Resolutions)
- The prognosis of Embryonal Rhabdomyosarcoma of Vagina depends on a combination of factors that include:
- The size of the tumor and the extent of its invasion: Individuals with small-sized tumors fare better than those with large-sized tumors
- Stage of cancer: With lower-stage tumors, when the tumor is confined to site of origin, the prognosis is usually excellent with appropriate therapy. In higher-stage tumors, such as tumors with metastasis, the prognosis is poor
- Cell growth rate of the cancer
- Overall health of the individual: Individuals with overall excellent health have better prognosis compared with those with poor health
- Individuals with bulky disease have a poorer prognosis
- Involvement of the regional lymph nodes, which can adversely affect the prognosis
- Involvement of vital organs may complicate the condition
- The surgical respectability of the tumor (meaning, if the tumor can be removed completely)
- Whether the tumor is occurring for the first time, or is a recurrent tumor. Recurring tumors have worse prognosis compared to tumors that do not recur
- Response to treatment: Tumors that respond to treatment have better prognosis compared to tumors that do not respond to treatment
- Progression of the condition makes the outcome worse
- With medical advancements and comprehensive treatment practices, the prognosis of Embryonal Vaginal RMS has shown great improvement. The overall cure rates range from between 90-95% (per the WHO) and the 10 year survival rate is around 90%
- The combination chemotherapy drugs used, may have some severe side effects (like cardio-toxicity). This chiefly impacts the elderly adults, or those who are already affected by other medical conditions. Individuals, who tolerate chemotherapy sessions better, generally have better outcomes
Additional and Relevant Useful Information for Embryonal Rhabdomyosarcoma of Vagina:
Amongst pediatric soft tissue sarcomas (affecting children less than 15 years), rhabdomyosarcomas form the largest category of malignant tumors.
Related Articles
Test Your Knowledge
Asked by users
Related Centers
Related Specialties
Related Physicians
Related Procedures
Related Resources
Join DoveHubs
and connect with fellow professionals

0 Comments
Please log in to post a comment.