Basal Cell Carcinoma of Skin
What are the other Names for this Condition? (Also known as/Synonyms)
- BCC of Skin
- Cutaneous Basal Cell Carcinoma
- Malignant Trichoblastoma
What is Basal Cell Carcinoma of Skin? (Definition/Background Information)
- Basal Cell Carcinoma (BCC) of Skin is a malignant cancer affecting the skin. It is a slow-growing tumor generally observed in older individuals, in both men and women. BCC of Skin is one of the most common skin cancers. Along with squamous cell carcinoma of the skin, these constitute the two most common cancers in the world
- This malignant carcinoma, which may be present as a lesion on the sun-exposed areas of the body, has the potential to metastasize (spread) to the lymph nodes. Some lesions may grow to large sizes and ulcerate. They can also infiltrate into the adjoining soft tissues and nerves. Larger tumors also have a greater tendency to recur after treatment
- The cause of Basal Cell Carcinoma of Skin is unknown, but factors such as chronic sun exposure, smoking, and ionizing radiation, are known to contribute towards its development. Also, fair-skinned Caucasians have a greater risk than dark-skinned Africans and Asians. Many patients over time develop more than one, or many Basal Cell Carcinomas of the Skin
- Any combination of chemotherapy, radiation therapy, and invasive procedures (surgery) are used to treat Basal Cell Carcinoma of Skin. Small-sized tumors and tumors that have not metastasized can be cured through appropriate skin surgery
- The prognosis for metastatic tumors depends upon many factors including the stage of the tumor, health status of the individual, and treatment response. The overall prognosis of Basal Cell Carcinoma of Skin may be guarded
There are multiple types of Basal Cell Carcinoma of Skin:
- Superficial Basal Cell Carcinoma of Skin
- Nodular Basal Cell Carcinoma of Skin
- Infiltrating Basal Cell Carcinoma of Skin
- Micronodular Basal Cell Carcinoma of Skin
- Fibroepithelial Basal Cell Carcinoma of Skin
- Basal Cell Carcinoma of Skin with Adnexal Differentiation
- Basosquamous Carcinoma of Skin
- Keratotic Basal Cell Carcinoma of Skin
Who gets Basal Cell Carcinoma of Skin? (Age and Sex Distribution)
- Basal Cell Carcinoma of Skin generally affects elderly or older adults; some cases rarely develop in children too
- It can occur in both males and females; however;
- Among the older age group, males are affected more than females
- In the younger age group, females are affected more than males, which may be attributed to their tendency to acquire sun-tanned bodies or visit skin tanning parlors more
- This condition is observed worldwide across all racial and ethnic groups; however, lighter-skinned individuals (especially Caucasians) are more prone to BCC of Skin than darker-skinned individuals (such as Asians, Africans, etc.)
What are the Risk Factors for Basal Cell Carcinoma of Skin? (Predisposing Factors)
The risk factors that contribute to Basal Cell Carcinoma of Skin formation include:
- Prolonged sun exposure, exposure to ultraviolet (UV) light
- Use of tanning beds, tanning parlors
- Arsenic exposure
- Ionizing radiation
- Smoking
- Immunosuppression of any type: The immunosuppression needed to avoid organ transplant rejection can lead to a patient developing many Basal Cell Carcinomas of Skin
- The presence of certain genetic syndromes such as basal cell nevus syndrome (a rare autosomal dominant disorder) increases the risk
- Caucasians are more vulnerable compared to other darker-toned individuals
It is important to note that having a risk factor does not mean that one will get the condition. A risk factor increases one's chances of getting a condition compared to an individual without the risk factors. Some risk factors are more important than others.
Also, not having a risk factor does not mean that an individual will not get the condition. It is always important to discuss the effect of risk factors with your healthcare provider.
What are the Causes of Basal Cell Carcinoma of Skin? (Etiology)
- The exact cause of development of Basal Cell Carcinoma of Skin is not completely known, in a majority of cases
- Although, genetic mutations have been detected in Basal Cell Carcinomas, which are currently being characterized
- Most BCCs are sporadic in origin i.e., they occur in a random fashion
What are the Signs and Symptoms of Basal Cell Carcinoma of Skin?
Basal Cell Carcinoma of Skin signs and symptoms may include:
- BCC is a generally slow-growing malignant tumor
- The tumor is a typical skin lesion, which has a papular and nodular appearance
- The surface of the papule may be red, if intact. Else, it may appear as an ulcer, if the surface is eroded
- It is typically observed on sun-exposed areas of the body; common sites include the head and neck region, arms and legs, etc.
- The tumor may be solitary or many in number. In children, if it is associated with basal cell nevus syndrome, then multiple lesions may be observed
- Some BCC of Skin may have pigmented appearance and may mimic a melanoma
- Most lesions are less than 1-2 cm, but some may grow to larger sizes of even 10 cm
- The lesion or tumor may grow and there may be itching sensation, ulceration, and bleeding
How is Basal Cell Carcinoma of Skin Diagnosed?
Some of the tests that may help in diagnosing Basal Cell Carcinoma of Skin include:
- Complete physical examination with detailed medical history evaluation
- Examination by a dermatologist using a dermoscopy, a special device to examine the skin
- Wood’s lamp examination: In this procedure, the healthcare provider examines the skin using ultraviolet light. It is performed to examine the change in skin pigmentation
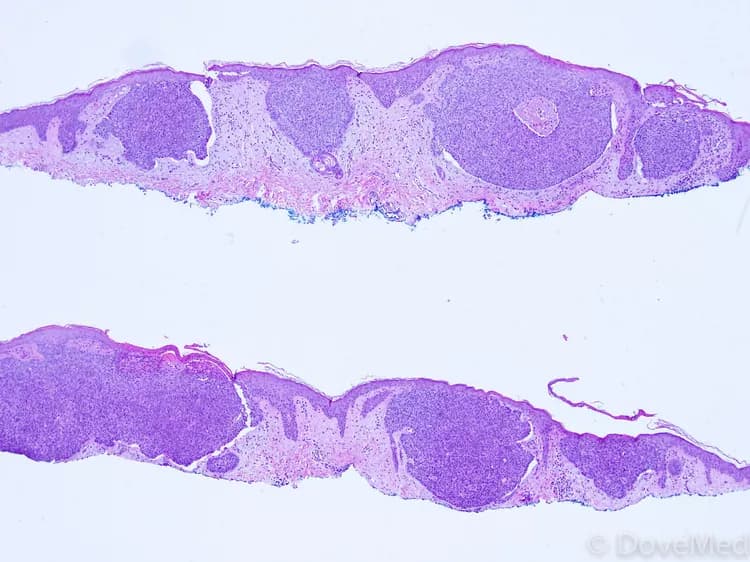
- Skin or tissue biopsy: A skin or tissue biopsy is performed and sent to a laboratory for a pathological examination, who examines the biopsy under a microscope. After putting together clinical findings, special studies on tissues (if needed) and with microscope findings, the pathologist arrives at a definitive diagnosis
- Differential diagnosis of other tumors should be ruled out; hence, biopsy is an important diagnostic tool
Many clinical conditions may have similar signs and symptoms. Your healthcare provider may perform additional tests to rule out other clinical conditions to arrive at a definitive diagnosis.
What are the possible Complications of Basal Cell Carcinoma of Skin?
The complications of Basal Cell Carcinoma of Skin could include:
- If the tumor becomes big, develops into a firm mass and ulcerates, it can get secondarily infected with bacteria or fungus
- Metastasis to regional lymph nodes can rarely occur. The tumor can also infiltrate into and destroy surrounding structures
- BCC of Skin can cause cosmetic issues, since these skin tumors can cause large ulceration (termed rodent ulceration)
- Recurrence of the tumor after a period of time; recurrence is frequently common with large tumors. The risk of recurrence is also higher with Infiltrative BCC and Micronodular BCC
- Side effects of chemotherapy (such as toxicity) and radiation
How is Basal Cell Carcinoma of Skin Treated?
In general, the treatment of Basal Cell Carcinoma of Skin depends upon a variety of factors including:
- The subtype of BCC
- The location of the tumor
- The number of tumors
- The size of the tumor
- Patient comorbidities
- Whether the tumor has metastasized
A combination of surgical treatment methods may be used to treat Basal Cell Carcinoma of Skin. The type of surgery may include:
- Curettage and cautery: This procedure is used for small tumors, usually not on the face. There is no requirement of sutures (stitches) after the surgery
- Excision of tumor: In this procedure, the tumor and surrounding tissue are removed with clear margins. Depending upon the amount of skin removed, surgical sutures may be necessary
- Mohs surgery: In this procedure, the tumor is removed layer by layer precisely, until clear margins are achieved. Each layer removed is examined under a microscope through a ‘frozen section’ procedure, examining between each stage for the presence of residual tumor
In most cases, a surgical removal of the entire tumor is the preferred treatment option. This can result in a cure.
- If the tumor has metastasized (in rare cases), then a combination of chemotherapy, radiation therapy, and invasive procedures may be used to treat the tumor
- Targeted therapy medications are generally used for locally infiltrated or metastatic BCCs. This therapy destroys the tumor cells by acting against the proteins that are responsible for tumor growth
- Large tumors that have infiltrated surrounding structures can be treated with radiation therapy (the use of high-energy beams to kill cancer cells)
- Large tumors after complete skin excision may need skin grafting
- Post-operative care is important: One must maintain minimum activity levels, until the surgical wound heals
Other techniques to treat this skin cancer (sometimes, when surgery may not be an option) may include:
- Photodynamic therapy: In this procedure, a chemical cream is applied onto the tumor, which sensitizes the tumor to light (photosensitization). After the cream application, the tumor is exposed to light. This combination of chemical therapy and light therapy kills the tumor. Usually this technique results in good cosmetic outcomes
- Radiation treatments: These can be curative and are generally painless. However, there are certain long-term complications that should be considered
- Oral hedgehog signal inhibitor medications: Vismodegib and sonidegib can shrink extremely large Basal Cell Carcinomas of Skin, making surgery feasible. These medications are used when primary surgery and radiation therapy are contraindicated
- Cryotherapy: Here the tumor tissue is destroyed through a freezing technique. Typically liquid nitrogen is used to freeze the tumor
- Topical creams, such as 5-fluorouracil cream and imiquimod cream, are two examples that can be used for topical treatment. These creams may be applied for several weeks, which slowly destroys the tumor. These options are typically used in very thin tumors only
Note: If multiple lesions occur in children, then the possibility of basal cell nevus syndrome should be eliminated.
Generally, proper follow-up care with regular screening and check-ups are important and encouraged. In the case of large lesions, close follow-up and periodic observation is essential, since they have a tendency to recur.
How can Basal Cell Carcinoma of Skin be Prevented?
Currently, Basal Cell Carcinoma of Skin is a malignant skin cancer that has no preventive measures. However, the following factors may help reduce the risk for the condition:
- Avoid or minimize sun exposure
- Limit the use of tanning beds, tanning parlors
- Smoking cessation
- If it is caused by certain underlying disorders, then treating the underlying condition may help in the treatment and early cure of BCC of Skin
- Regular medical screening at periodic intervals with blood tests, scans, and physical examinations, are mandatory, due to its metastasizing potential and high possibility of recurrence. Often several years of active vigilance is necessary
- For immunocompromised patients with organ transplantation, HIV/AIDS, or leukemia/lymphoma, regular skin examinations by a dermatologist as often as three months is recommended
What is the Prognosis of Basal Cell Carcinoma of Skin? (Outcomes/Resolutions)
- In general, the prognosis of Basal Cell Carcinoma of Skin is excellent, if it is detected and treated early. However, if it metastasizes to the local lymph nodes, the prognosis is guarded or unpredictable
- In such cases of metastatic BCC of Skin, its prognosis depends upon a set of several factors that include:
- Stage of tumor: With lower-stage tumors, when the tumor is confined to site of origin, the prognosis is usually excellent with appropriate therapy. In higher-stage tumors, such as tumors with metastasis, the prognosis is poor
- The surgical resectability of the tumor (meaning, if the tumor can be removed completely)
- Overall health of the individual: Individuals with overall excellent health have better prognosis compared to those with poor health
- Age of the individual: Older individuals generally have poorer prognosis than younger individuals
- Whether the tumor is occurring for the first time, or is a recurrent tumor. Recurring tumors have a poorer prognosis compared to tumors that do not recur
- Response to treatment: Tumors that respond to treatment have better prognosis compared to tumors that do not respond so well to treatment
- Without treatment (or with delayed treatment), Basal-Cell Cancer of Skin can metastasize and this may result in a poor prognosis. Nevertheless, metastasis is rare and occurs in about 1 in 10,000 cases only
- BCCs of the head that have infiltrated through the skull into the brain have poor prognosis
- Close and regular follow-up and long-term monitor for recurrence of BCC has to be maintained
Additional and Relevant Useful Information for Basal Cell Carcinoma of Skin:
There are also other types of Basal Cell Carcinoma of Skin, which include:
- Cystic Basal Cell Carcinoma of Skin: When examined under the microscope, they have large cystic spaces, and hence the name
- Sclerosing Basal Cell Carcinoma of Skin: The tumor cells are present in a dense fibrous stroma, when examined under the microscope, and hence the name. It is also known as Morpheaform BCC
- Pigmented Basal Cell Carcinoma of Skin: These tumors have brown to dark brown pigmentation, which is due to accumulation of melanin pigment within the tumor. Due to its appearance, the tumor may be confused with malignant melanoma
Related Articles
Test Your Knowledge
Asked by users
Related Centers
Related Specialties
Related Physicians
Related Procedures
Related Resources
Join DoveHubs
and connect with fellow professionals


0 Comments
Please log in to post a comment.