What are the other Names for this Condition? (Also known as/Synonyms)
- Angiosarcoma of Cervix
- Cervical Angiosarcoma
What is Angiosarcoma of Uterine Cervix? (Definition/Background Information)
- Angiosarcoma of Uterine Cervix is an infrequent, aggressive, and often rapidly-developing tumor, without signs and symptoms in the early stages. The tumor arises from the vascular linings which involve the blood vessels
- They are regarded as a type of high-grade malignancy that spreads and infiltrates the surrounding tissues and organs. “High-grade” means that the tumor is very aggressive
- Cervical Angiosarcomas are seen in adult women. The signs and symptoms of the tumor may include abnormal vaginal discharge and bleeding
- A combination of chemotherapy (drugs), radiation therapy, and surgical procedures, are used to treat these soft tissue tumors
- The outcome for an individual with Angiosarcoma of Uterine Cervix is poor, due to its aggressive nature and high metastasizing rate
Who gets Angiosarcoma of Uterine Cervix? (Age and Sex Distribution)
- Angiosarcoma of Uterine Cervix is a rare tumor that is seen in adult women; mostly in women during or after menopause (age 40 years and above)
- There is no known ethnic or racial preference
What are the Risk Factors for Angiosarcoma of Uterine Cervix? (Predisposing Factors)
No specific risk factors for Angiosarcoma of Uterine Cervix have been currently established. However, in general, the risk for angiosarcoma of soft tissue is linked to the following factors:
- A previously performed radiotherapy for other cancer conditions, called radiation-induced angiosarcoma. The radiation has an expected side effect of damaging the genetic material in the normal cells. This can lead to the development of a “secondary” cancer
- Chronic obstruction of the lymph vessels, called lymphedema
- Exposure to chemical and environmental contaminants such as arsenic, thorium dioxide, vinyl chloride, dioxin, and many other agents
- Presence of foreign materials in the body, such as graft material (plastic, steel), bone wax, polyester fiber (Dacron, from sutures), etc., which are sometimes known to act as carcinogenic (cancer-causing) agents
- Angiosarcoma of soft tissue has also been associated to occur in patients diagnosed with neurofibromatosis (type 1), Klippel-Trenaunay syndrome, and Maffucci syndrome
- Individuals affected by immune deficiency disorders, such as AIDS, have a higher risk of developing the tumor
It is important to note that having a risk factor does not mean that one will get the condition. A risk factor increases one's chances of getting a condition compared to an individual without the risk factors. Some risk factors are more important than others.
Also, not having a risk factor does not mean that an individual will not get the condition. It is always important to discuss the effect of risk factors with your healthcare provider.
What are the Causes of Angiosarcoma of Uterine Cervix? (Etiology)
The exact cause and mechanism of formation of Angiosarcoma of Uterine Cervix is unknown. They are thought to occur as a reactive process, owing to the effect of some preexisting factor(s).
Such preexisting factors may include:
- Radiation exposure
- Chronic lymphedema
- Exposure to chemicals and environmental pollutants
- Presence of foreign materials in the body for long periods (such as an implant or graft)
What are the Signs and Symptoms of Angiosarcoma of Uterine Cervix?
The signs and symptoms of Angiosarcoma of Uterine Cervix include:
- The soft tissue malignant tumors initially grow at a moderate rate, and then suddenly start progressing rapidly, during the later stages. In most cases, the initial tumor growth periods are asymptomatic
- Due to large size of tumor growth, the adjoining organs, nerves, and muscles, may be compressed or restricted. Often, these signs may be the first indications of the tumor
- The tumor may present as a flattened mass
- Abnormal vaginal discharge or vaginal bleeding
- Ulceration of the tumor may be observed
- Enlarged lymph nodes
- Pelvic pain
- Pain during sexual intercourse
- Frequent urination or urination difficulties
- Lower back pain
How is Angiosarcoma of Uterine Cervix Diagnosed?
A diagnosis of Angiosarcoma of Uterine Cervix may involve the following procedures:
- Evaluation of the individual’s medical history and a thorough physical (pelvic) examination
- Ultrasound scan of the abdomen
- CT or CAT scan with contrast of the abdomen and pelvis may show a well-defined mass. This radiological procedure creates detailed 3-dimensional images of structures inside the body
- MRI scans of the abdomen and pelvis: Magnetic resonance imaging (MRI) uses a magnetic field to create high-quality pictures of certain parts of the body, such as tissues, muscles, nerves, and bones. These high-quality pictures may reveal the presence of the tumor
- Colposcopy: The cervix is examined with an instrument, called a colposcope. This helps the physician get a magnified view of the cervix
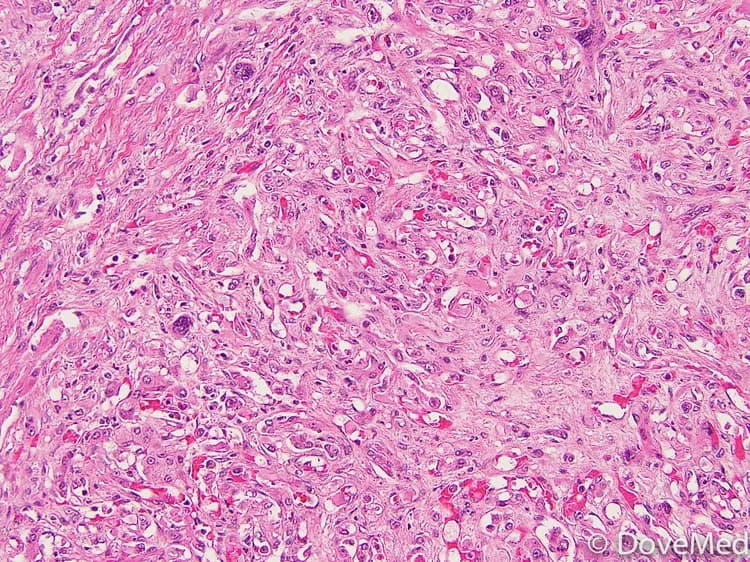
Cervical biopsy: Biopsy is the process of removing tissue for examination. A pathologist looks at the tissue sample under a microscope, to detect any evidence of cancer. Types of cervical biopsies include:
- Colposcopic biopsy: The abnormal areas of the cervix are visualized with a colposcope. After numbing the cervix with a local anesthetic, an instrument, called a biopsy forceps, is used to get a tissue sample. Mild cramps, pain, and some light bleeding, may occur following the procedure
- Endocervical curettage (endocervical scraping): The curette is an instrument that can be used to scrape out tissue. Using a curette, cells are scraped out from the endocervix (the inner part of the cervix, close to the uterus/womb) and examined under a microscope. Mild pain and bleeding maybe present following the procedure.
Cone biopsy or conization: This procedure is only helpful if the tumors are small enough to be completely excised by conization surgical procedure. In a majority of cases of Cervical Angiosarcoma, the tumor is diagnosed in the advanced stages, and hence, conization is rarely helpful.
- A cone-shaped piece of tissue is removed from the cervix during conization
- The exocervix (the outer part) forms the base of this cone, while the endocervix (the inner part) forms the apex
Two methods can be used to obtain a cone biopsy specimen:
- Loop electrosurgical procedure (LEEP, LLETZ): After numbing the area with a local anesthetic, a wire loop heated with electricity is used to remove a tissue specimen. This procedure, lasting about 10 minutes, may cause some cramping and mild-to-moderate bleeding, for a few weeks
- Cold knife cone biopsy: This procedure is performed, either under general anesthesia or under spinal anesthesia. The tissue sample is removed using a surgical scalpel or through laser
If tumor has metastasized (into the lungs or other regions) then PET scan, bone scan, and chest X-rays may be taken.
Note: Pap smear is not a good screening tool for Cervical Angiosarcoma.
Many clinical conditions may have similar signs and symptoms. Your healthcare provider may perform additional tests to rule out other clinical conditions to arrive at a definitive diagnosis.
What are the possible Complications of Angiosarcoma of Uterine Cervix?
The complications of Angiosarcoma of Uterine Cervix may include:
- Usually by the time Cervical Angiosarcomas are detected, it is likely that these tumors have grown aggressively, invaded locally, and metastasized damaging organs and tissues beyond repair
- The tumor has a high recurrence rate, even after surgical excision and removal
- Blood loss during invasive treatment methods may be heavy
- Damage of vital nerves, blood vessels, and surrounding structures during surgery
- Sexual dysfunction can take place as a side effect of surgery, chemotherapy, or radiation therapy
- Side effects from chemotherapy (toxicity), radiation therapy
How is Angiosarcoma of Uterine Cervix Treated?
Once a diagnosis of cervical cancer has been made, the extent to which the tumor has spread is assessed. This is called staging.
Following is the staging protocol for cervical cancer, according to the American Joint Committee on Cancer (AJCC), updated July 2016:
Stage 0 cervical cancer (carcinoma in situ):
- In this stage, abnormal cells are found in the innermost lining of the cervix
- These abnormal cells may become cancer and spread into nearby normal tissue
Stage I cervical cancer: The cancer is found only in the cervix. Stage I is divided into stages IA and IB, based on the amount of cancer that is found.
- Stage IA: A very small amount of cancer that can only be seen with a microscope is found in the tissues of the cervix
- In stage IA1, the cancer is not more than 3 mm deep and not more than 7 mm wide
- In stage IA2, the cancer is more than 3 mm, but not more than 5 mm deep; it is not more than 7 mm wide
- Stage IB: It is divided into stages IB1 and IB2, based on the size of the tumor
- In stage IB1, the cancer can only be seen with a microscope and is more than 5 mm deep and more than 7 mm wide; or the cancer can be seen without a microscope and is not more than 4 cm
- In stage IB2, the cancer can be seen without a microscope and is more than 4 cm
Stage II cervical cancer: The cancer has spread beyond the uterus, but not onto the pelvic wall (the tissues that line the part of the body between the hips), or to the lower third of the vagina. Stage II is divided into stages IIA and IIB, based on how far the cancer has spread.
- Stage IIA: The cancer has spread beyond the cervix to the upper two-thirds of the vagina, but not to tissues around the uterus
- Stage IIA is divided into stages IIA1 and IIA2, based on the size of the tumor
- In stage IIA1, the tumor can be seen without a microscope and is not more than 4 cm in size
- In stage IIA2, the tumor can be seen without a microscope and is more than 4 cm in size
- Stage IIB: The cancer has spread beyond the cervix to the tissues around the uterus, but not onto the pelvic wall
Stage III cervical cancer: The cancer has spread to the lower third of the vagina, and/or onto the pelvic wall, and/or has caused kidney problems. Stage III is divided into stages IIIA and IIIB, based on how far the cancer has spread.
- Stage IIIA: The cancer has spread to the lower third of the vagina, but not onto the pelvic wall
- Stage IIIB: The cancer has spread to the pelvic wall; and/or the tumor has become large enough to block the ureters (the tubes that connect the kidneys to the urinary bladder). This blockage can cause the kidney to enlarge or stop working
Stage IV cervical cancer: In stage IV, the cancer has spread beyond the pelvis, or can be seen in the lining of the bladder and/or rectum, or has spread to other parts of the body. Stage IV is divided into stages IVA and IVB, based on where the cancer has spread.
- Stage IVA: The cancer has spread to the nearby organs, such as the urinary bladder or rectum
- Stage IVB: The cancer has spread to other parts of the body, such as to the lymph nodes, lung, liver, intestine, or bone
(Source: Stages of Cervical Cancer, July 2016, provided by the National Cancer Institute at the National Institutes of Health; U.S. Department of Health and Human Services)
The treatment of Angiosarcoma of Cervix may be undertaken as:
- Any combination of chemotherapy, radiation therapy, and invasive procedures (surgery) are used to treat Cervical Angiosarcomas
- Surgery may include the following procedures:
- Conization procedure, besides helping with the biopsy, can also help in treating very early-stage cervical cancers in women, who want to preserve their childbearing ability
- Radical trachelectomy: The surgeon removes the cervix, upper part of the vagina, and nearby lymph nodes, while preserving the ability to have children
- Hysterectomy: In this procedure, the uterus and cervix are removed. This is done by making an incision on the abdomen (termed abdominal hysterectomy), or through the vagina (termed vaginal hysterectomy), or by using a laparoscope (termed laparoscopic hysterectomy). Surgery is performed under general or epidural anesthesia, though the ability to have children is lost. Complications, such as bleeding, infection, or damage to the urinary tract, or the intestinal system may occur in rare cases
- Radical hysterectomy: The uterus, cervix, the upper part of the vagina and tissues, next to the uterus are removed. Additionally, some pelvic lymph nodes may also be surgically taken out. The surgery is performed under anesthesia and may be carried out, via an incision made on the abdomen or by using laparoscopy. With this invasive procedure, the ability to have children is lost. Rarely, complications such as bleeding, infection, or damage to the urinary tract or the intestinal system, may occur. Removal of lymph nodes may lead to swelling of legs (lymphedema)
- Pelvic exenteration: The uterus, tissues surrounding the uterus, cervix, pelvic lymph nodes, and the upper part of the vagina, are removed. In addition, depending on the tumor spread, the remainder of the vagina, the bladder, rectum, and a part of the colon, may also be removed. Recovery from this surgery takes a long period
- Embolization may be used to provide temporary relief from the symptoms, and reduce blood loss during a surgical procedure
- Chemotherapy:
- Medications are used to kill the tumor cells, which may be given as oral pills or injected into veins
- A combination of chemotherapy medications may be used
- Radiation therapy:
- This procedure uses high-energy beams to kill the cancer cells
- These beams may be delivered from outside the body (external beam radiation therapy) or the radioactive material maybe placed inside the vagina or the uterus (internal radiation therapy or brachytherapy)
- Post-operative care is important: One must maintain minimum activity levels, until the surgical wound heals
- Follow-up care with regular screening and check-ups are important
How can Angiosarcoma of Uterine Cervix be Prevented?
There is no definitive method to prevent Angiosarcoma of Uterine Cervix occurrence. However, certain general precautions that decrease the incidence of cancer in the body may be considered.
- Adopting a lifestyle that avoids prolonged exposure to pollutants and carcinogens, either at home or at work may help in preventing cancers
- Due to its high metastasizing potential and high recurrence rate, regular medical screening at periodic intervals with blood tests, scans, and physical examinations, are mandatory for those who have already been treated for this tumor
What is the Prognosis of Angiosarcoma of Uterine Cervix? (Outcomes/Resolutions)
- Angiosarcoma of Uterine Cervix is a rare, very aggressive, and highly-malignant tumor. The long-term prognosis depends on a combination of factors, such as:
- The size of the tumor and the extent of its invasion: Individuals with small-sized tumors fare better than those with large-sized tumors
- Stage of cancer: With lower-stage tumors, when the tumor is confined to site of origin, the prognosis is usually excellent with appropriate therapy. In higher-stage tumors, such as tumors with metastasis, the prognosis is poor
- Cell growth rate of the cancer
- Its ki-67 value - a protein found in cells that is a good indicator of how fast the tumor cells are growing. The ki-67 value is determined by a pathologist and is usually mentioned in the pathology report
- Overall health of the individual: Individuals with overall excellent health have better prognosis compared with those with poor health
- Age of the individual: Older individuals generally have poorer prognosis than younger individuals
- Individuals with bulky disease have a poorer prognosis
- Involvement of the regional lymph nodes, which can adversely affect the prognosis
- Involvement of vital organs may complicate the condition
- The surgical respectability of the tumor (meaning, if the tumor can be removed completely)
- Whether the tumor is occurring for the first time, or is a recurrent tumor. Recurring tumors have worse prognosis compared to tumors that do not recur
- Response to treatment: Tumors that respond to treatment have better prognosis compared to tumors that do not respond to treatment
- Progression of the condition makes the outcome worse
- The best treatment practice for Angiosarcoma of Cervix involves a combination of radiotherapy with surgical intervention. However, given the high rate of recurrence and metastasis, the long-term outcome (5-year) is poor for most individuals
- An early diagnosis and prompt treatment of the tumor generally yields better outcomes than a late diagnosis and delayed treatment
- The combination chemotherapy drugs used, may have some severe side effects (like cardio-toxicity). This chiefly impacts the elderly adults, or those who are already affected by other medical conditions. Individuals, who tolerate chemotherapy sessions better, generally have better outcomes
Additional and Relevant Useful Information for Angiosarcoma of Uterine Cervix:
Angiosarcomas can occur anywhere in the body; the most common tumors include the following:
- Angiosarcoma of skin
- Angiosarcoma of breast
- Angiosarcoma of spleen
- Angiosarcoma of liver
- Angiosarcoma of soft tissue
Related Articles
Test Your Knowledge
Asked by users
Related Centers
Related Specialties
Related Physicians
Related Procedures
Related Resources
Join DoveHubs
and connect with fellow professionals

0 Comments
Please log in to post a comment.