Biomarkers Outperform Symptoms In Parsing Psychosis Subgroups
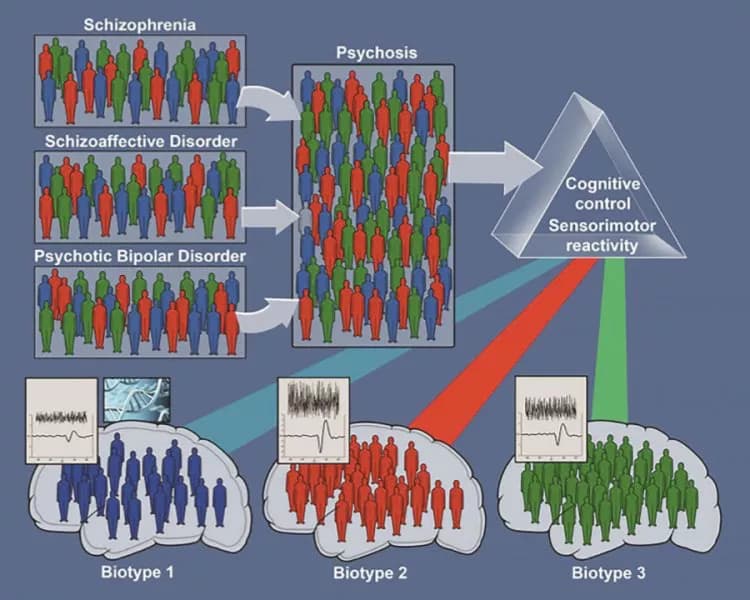
Three biomarker-based categories, called biotypes, outperformed traditional diagnoses, such as schizophrenia and bipolar disorder with psychosis, in sorting psychosis cases into distinct subgroups on the basis of brain biology, report researchers funded by the National Institutes of Health. A hallmark of severe mental illness, psychosis is marked by hallucinations and delusions, or false, irrational beliefs.
"The biotypes were more biologically homogeneous than categories based on observable symptoms," explained Bruce Cuthbert, Ph.D., acting director of the NIH's National Institute of Mental Health (NIMH), which funded the study. "Just as fever or infection can have many different causes, multiple psychosis-causing disease processes -- operating via different biological pathways -- can lead to similar symptoms, confounding the search for better care."
The results lend support to the institute's Research Diagnostic Criteria (RDoC) initiative, which frees scientists from designing research based on traditional diagnostic categories, encouraging them to explore groupings based on genomics, behavioral dimensions, physiological traits, or brain imaging findings. More precise diagnosis is expected to lead to improved treatments.
NIMH-funded researchers Carol Tamminga, M.D., of the University of Texas Southwestern Medical Center, Dallas; Brett Clementz, Ph.D., of the University of Georgia, Athens; and colleagues at other research centers, report on their multi-site study on Dec. 8, 2015 in the American Journal of Psychiatry.
The new findings come from a project called The Bipolar Schizophrenia Network on Intermediate Phenotypes (BSNIP). They add to increasing evidence of biological overlap between traditional, symptom-based diagnostic categories for disorders in which patients experience psychotic symptoms. The BSNIP study used sophisticated statistical approaches to sort such cases into homogeneous subgroups, based on multiple neurobiological measures and levels of analysis.
The researchers examined key biological and behavioral measures linked to psychosis in 1,872 participants -- patients diagnosed with schizophrenia, schizoaffective disorder and bipolar disorder with psychosis, their first-degree relatives and healthy control subjects. Measures such as performance on thinking, planning and memory tasks, eye-tracking, inhibition, and brainwave responses to auditory stimuli identified sets of biomarkers that differentiated subgroups of patients. Three distinct psychosis-related biotypes emerged that cut across clinical diagnosis boundaries.
These subsets of biomarkers differentiated groupings of psychosis cases from each other considerably better than did traditional clinical diagnoses. External measures -- social functioning, brain structure, and rates of psychosis-related illness and biomarker patterns in patients' first-degree relatives -- also validated the neurobiological distinctiveness of the biotype subgroups more than they did the distinctiveness of symptom-based categories.
People with different biotypes differed in their mix of psychosis-related impairments. For example, cases classified as Biotype 1 showed the most severe impairment in a set of brain functions that the researchers distilled into a construct they call "cognitive control" -- the ability to flexibly exert control over attention and information processing to meet one's goals. Biotype 1 cases were also the most socially impaired. Biotype 2 cases showed intermediate levels of impaired cognitive control, but had normal to accentuated brain responses to sensory inputs and fast visual orienting, a set of brain functions called "sensorimotor reactivity" -- the ability to detect and process sensory stimuli. Those classified as Biotype 3 showed normal cognitive control, modestly impaired sensorimotor reactivity, were the least socially impaired and had the lowest positive (e.g., hallucinations and delusions) and negative (e.g., blunted emotion) symptoms.
Each biotype overlapped with the traditional diagnostic categories. For example, among Biotype 1 cases, 59 percent had a schizophrenia diagnosis, while among Biotype 3 cases 44 percent had a bipolar disorder with psychosis diagnosis.. Among Biotype 3 cases, 32 percent had schizophrenia, and among Biotype 1 cases, 20 percent had bipolar disorder with psychosis.
Differences in brain structure also distinguish the three biotypes, further validating the categorizations. On brain MRI scans, Biotype 1 cases -- and to a lesser degree Biotype 2 cases -- showed reduced gray matter, the brain's working tissue, across several areas of the cortex, or outer mantle, known to process higher-order information. By contrast, in Biotype 3 cases, the largest of the groups, such reduced gray matter was mostly localized in emotion-processing areas in deeper brain regions. No brain structural differences distinguished the traditional categories of schizophrenia and schizoaffective disorder from each other.
Unaffected first-degree relatives of psychosis cases tended to show similar, but reduced, abnormalities in cognitive control, sensorimotor reactivity, social functioning and brain structure, suggesting that they may harbor "constitutional" risk factors for the biotypes.
The different patterns of biomarkers across the biotypes may help to explain discrepancies in replicating biomarker studies across different clinical research centers, say the researchers. For example, since they tend to be the most compromised, Biotype 1 cases are more likely to be recruited in inpatient settings, while Biotype 2 and -3 cases are more likely to be found in outpatient settings. So even if patients have the same nominal diagnosis, they might tend to have different underlying illness processes. Similarly, researchers with mostly Biotype 3 cases might conclude that not much can be learned from studying first-degree relatives (their relatives were largely normal on the biomarkers) -- and/or that a large portion of the genetic risk for psychosis comes from spontaneous mutations.
"The biotypes outcome provides proof-of-concept that structural and functional brain biomarker measures can sort individuals with psychosis into groups that are neurobiologically distinctive and appear biologically meaningful," said Dr. Tamminga.
The new findings suggest several leads for future research, say the investigators. Biotypes 1 and 2 may lend themselves to genetic studies, while Biotype 3 cases may yield more leads on environmental contributions to psychosis risk. Treatments for Biotype 1 should target cognitive control and enhance brain mechanisms for discerning the relevance of environmental stimuli. Cases with Biotypes 1 and 2 might be good candidates for treatments that correct neuronal activity levels through effects on cellular potassium or calcium channels.
The above post is reprinted from materials provided by NIH/National Institute of Mental Health. Note: Materials may be edited for content and length.
Disclaimer: DoveMed is not responsible for the adapted accuracy of news releases posted to DoveMed by contributing universities and institutions.
Primary Resource:
Clementz, B. A., Sweeney, J. A., Hamm, J. P., Ivleva, E. I., Ethridge, L. E., Pearlson, G. D., ... & Tamminga, C. A. (2015). Identification of Distinct Psychosis Biotypes Using Brain-Based Biomarkers. American Journal of Psychiatry.
Related Articles
Test Your Knowledge
Asked by users
Related Centers
Related Specialties
Related Physicians
Related Procedures
Related Resources
Join DoveHubs
and connect with fellow professionals

0 Comments
Please log in to post a comment.