Preeclampsia is a hypertensive disorder that can complicate pregnancy and can cause maternal and prenatal mortality and morbidity. Timely intervention by healthcare providers can save the mother and the baby. Swelling and high albumin in the urine during the 20th week or the first week after delivery is common in preeclampsia patients.
Symptoms of preeclampsia:
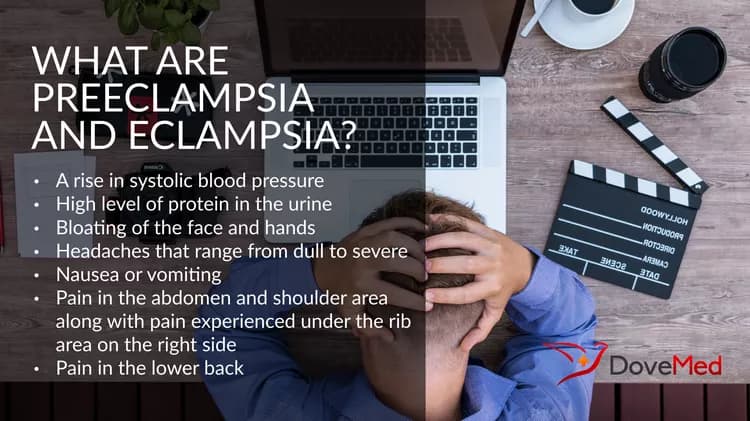
The biggest drawback is that there are no symptoms until hospitalization. Though, some of the signs to watch out for include:
- A rise in systolic blood pressure of more than 30 mm Hg and diastolic blood pressure raising by 15 mm Hg or more. Blood pressure more than 140/90 is a cause for concern
- High level of protein in the urine
- Bloating of the face and hands often known as edema is caused due to accumulation of excess fluids.
- Headaches that range from dull to severe is a cause for concern
- Nausea or vomiting that would not go away after the first trimester has to be monitored for preeclampsia
- Pain in the abdomen and shoulder area called as epigastric pain, along with pain experienced under the rib area on the right side has to be monitored
- Pain in the lower back is common
- Increase in weight of around 2 pounds in a week following leakage is a cause for concern
- Blurriness in vision
- Shortness of breath
The American College of Obstetricians and Gynecologists (ACOG) in 2013 informed that proteinuria may not be a cause for preeclampsia.
Eclampsia:
Eclampsia causes spastic seizures that is not due to a brain condition and can lead to coma, if left unattended or untreated. Factors like diet, genetics, and conditions related to blood vessels, can lead to eclampsia. Healthcare providers are still not sure what exactly causes the condition. Though, in most cases it is followed by preeclampsia.
Risk factors for preeclampsia:
Nearly 5% of women develop preeclampsia especially during their first pregnancy. Women already having complaints of high blood pressure or vascular disease before pregnancy, have a high risk of preeclampsia.
Leaving preeclampsia untreated can lead to eclampsia. This condition can become fatal, if left untreated. The placenta detaches itself early in the pregnant women having this condition. a lack of blood flow to the placenta can result in preterm birth and breathing disorder in the baby. A life-threatening condition called ‘HELLP’ that causes disintegration of red blood cells, low platelet count and high secretion of liver enzymes may occur. Preeclampsia can lead to cardiovascular disease. Constant monitoring is needed for pregnant women who suffer from headaches, vision disorder, faint fetal heartbeat and vaginal bleeding.
Preeclampsia can be diagnosed with a series of blood tests and urine tests. Tests of liver function can also help identify the condition.
Treatment of preeclampsia:
- Strict bed rest is recommended for woman with mild preeclampsia.
- Restriction of salt intake and drinking more water is recommended. But, it was inferred that reducing the intake of dietary salt cannot prevent preeclampsia, according to study conducted by Duley and team, which is found in the WHO recommendations for prevention and treatment of pre-eclampsia and eclampsia
- Magnesium sulfate doses can bring back the reflexes to normal and reduce seizures
- 8-6 weeks after delivery the symptoms of preeclampsia may subside
- Monitoring the woman’s condition after labor is important to prevent eclampsia
Related Articles
Test Your Knowledge
Asked by users
Related Centers
Related Specialties
Related Physicians
Related Procedures
Related Resources
Join DoveHubs
and connect with fellow professionals

0 Comments
Please log in to post a comment.