What are the other Names for this Condition? (Also known as/Synonyms)
- Testicular Seminoma
What is Seminoma of Testis? (Definition/Background Information)
- Seminoma of Testis is a malignant testicular tumor of germ cells, which are the precursors of sperms. It is a common malignant testicular tumor that can occur either in one or both the testis
- It can be classified into 3 distinct types:
- Classic Seminoma - the most common histologic type
- Anaplastic Seminoma - observed in 5-15% of the individuals
- Spermatocytic Seminoma - a rare variant that occurs in older adults
- Seminoma of Testis is the most common tumor type in young males, 20-35 years of age. It occurs mostly as a solid mass that is either homogenous or nodular and presents a rapid growth
- The complications of Testicular Seminomas are mainly due to metastasis to local and distant organs, and as result of side effects of chemotherapy and radiotherapy
- The cause of Testicular Seminoma is unknown in many cases, but it is associated with cryptorchidism (or undescended testis), genetic mutations (especially involving the amplification of short arm of chromosome 12 or mutations in chromosome 9), and other factors
- A combination of radiotherapy, chemotherapy (drugs), and surgical procedures may be used to treat Seminoma of Testis. Debulking surgery to reduce tumor mass followed by radiotherapy and chemotherapy may also be undertaken. The debulking procedure helps the chemotherapy treatment to be more effective, because there is less tumor mass for the drugs to act on
- In most of the cases, the cancer is detected before it spreads to other parts of the body. The prognosis of seminoma is very good among testicular cancers, even in advanced metastatic stage
Who gets Seminoma of Testis? (Age and Sex Distribution)
- Seminoma of Testis can occur worldwide in males of any age. But, they commonly tend occur in young adult males around the age of 20-35 years
- Seminomas account for only 0.3-0.6% of all cancers affecting males. It is rarely observed in children
- Individuals of all racial and ethnic background may be affected. However, the tumor is more common among the Caucasians than Africans; it is more commonly seen in the Caucasian population of Denmark, Germany, Norway, Hungary, Switzerland, and other European countries
What are the Risk Factors for Seminoma of Testis? (Predisposing Factors)
Following are the risk factors for Seminoma of Testis:
- Undescended testis is the major risk factor for Testicular Seminoma. In this condition, one or both the testicles fail to descend into the scrotum from the abdomen. Normally, the testicles descend into the scrotum, either before birth or within few months after birth. In some cases, it never descends, causing the testicles to remain in the abdomen, even one year after birth. Undescended testis present in the abdomen has the highest chance of developing Testicular Seminoma, followed by its presence in the inguinal canal
- Presence of carcinoma in situ (CIS) or intratubular germ cell neoplasia increases the risk of testicular cancer
- Family history of testicular cancer
- HIV infection and decreased immunity due to a kidney transplant has been shown to increase risk for some testicular cancers
- Infertility
- Smoking: Some studies have shown that longstanding smoking increase the risk
- Presence of hypospadias, inguinal hernia
- Atrophy of testis due to variety of causes
- Presence of a condition called gonadal dysgenesis, wherein there is an abnormal development of a testicle
- Individuals with low birth weight may have increased risk of developing the tumors
- Prior history of chemotherapy for a different malignancy
It is important to note that having a risk factor does not mean that one will get the condition. A risk factor increases one's chances of getting a condition compared to an individual without the risk factors. Some risk factors are more important than others.
Also, not having a risk factor does not mean that an individual will not get the condition. It is always important to discuss the effect of risk factors with your healthcare provider.
What are the Causes of Seminoma of Testis? (Etiology)
In many cases, the cause of Testicular Seminoma remains unknown. Among known causative factors, the most common cause of Seminoma of Testis is cryptorchidism, or the failure of the testes to descend into the scrotum. Some of the other causes may include:
- Genetic defects
- Smoking
- A weakened immune system (immune-compromised)
- Exposure to:
- Radiation
- Chemicals
- Pesticides
- Family history of testicular cancer
- Increasing age
- Is not associated with any known congenital syndrome
- Prior history of chemotherapy for different malignancy
- Amplification of short arm of chromosome 12 or chromosome 9 are seen in Seminoma of Testis
Currently, research is underway to improve our understanding of Testicular Seminoma.
What are the Signs and Symptoms of Seminoma of Testis?
The Seminoma of Testis is most non-lethal of all testicular cancers and is mostly diagnosed in 75% of the cases in the early stages, when the tumor is localized to the testis. However, in approximately 15% of the cases, the tumor might have involved the regional lymph nodes, and 5-10% presents with the involvement of juxta-regional nodes or visceral metastases.
The signs and symptoms of Seminoma of Testis may include the following:
- In a majority of the cases, the tumor is present as a single mass (or lump) within the testicle; though rarely, the tumor can occur as multiple masses within a single testicle too
- The testicular mass may or may not be accompanied with pain in the testis or groin region
- Feeling of heaviness in the scrotum with or without scrotal enlargement
- May be accompanied with the presence of fluid in the scrotum, called hydrocele
- Abdominal pain (usually a pelvic pain)
- Abdominal swelling due to the mass or due to fluid accumulation in belly (called ascites)
- Increased abdominal girth due to fluid accumulation (ascites)
- Persistent feeling of abdominal bloating with nausea or vomiting
- Changes in bowel movements such as constipation
- Breast pain due to hormonal production by the tumor. There may be breast enlargement, termed as gynecomastia
- Back pain may be caused by metastasis of the tumor to the abdomen; difficulty in breathing due to spread to lungs
- Swelling of one or both the legs
- Loss of appetite with weight loss; feeling full sooner after a meal (easily having a feeling of satiety)
- Fatigue (feeling tired easily)
- Frequent urination (polyuria) and difficulty while urinating
- Headache, vomiting, and paralysis due to spread to central nervous system
- Low blood pressure and anemia due to blood loss
- Seminomas are intermediately growing tumors that takes about weeks to months to grow
How is Seminoma of Testis Diagnosed?
Seminoma of Testis is diagnosed by a complete medical history and a thorough physical examination. In addition, the following examinations and diagnostic tests are helpful:
- Testicular examination
- Complete blood count (CBC) with differential of white blood cells
- Liver function Test (LFT)
- Blood tests, called serum tumor markers: Normal levels of alpha fetoprotein (AFP) is particularly seen with Seminoma of Testis
- Other blood tests that may be performed include:
- Human chorionic gonadotropin (hCG) levels are elevated
- Lactate dehydrogenase (LDH) blood test
- Testosterone levels blood test
- Differential diagnosis, to eliminate other tumor types are often considered, before arriving at a definitive diagnosis
- Genetic testing to determine the mutation in the tumors that may help either with diagnosis, treatment, or prognosis
- Radiological imaging studies such as:
- X-ray of the chest, abdomen, and pelvic region
- Ultrasound scans of the pelvic region: Usually testicular ultrasonography and abdominal ultrasound are performed. These studies are very helpful in suspecting a testicular tumor
- CT scan of the brain to rule out brain metastasis
- Vascular radiological studies of abdomen and pelvic region
- Whole body bone scan
- Positron emission tomography (PET) scan or PET/CT scan
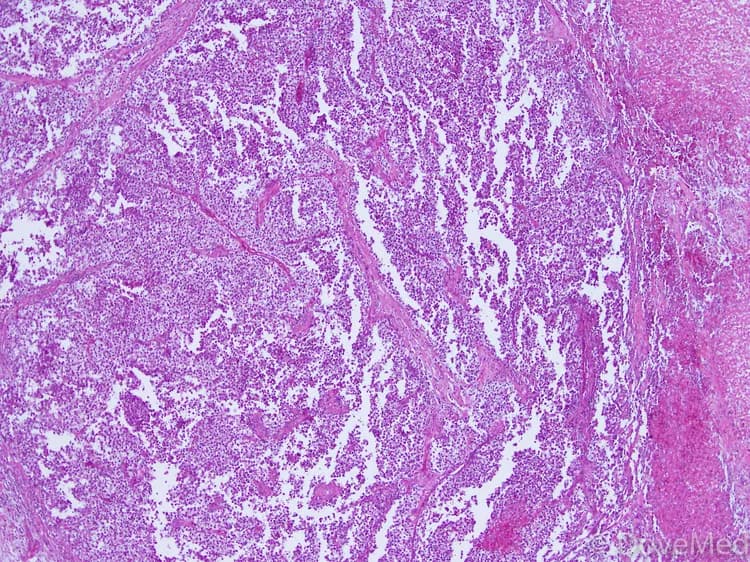
- A tissue biopsy of the tumor: A tissue biopsy is performed and sent to a laboratory for a pathological examination. A pathologist examines the biopsy under a microscope. After putting together clinical findings, special studies on tissues (if needed) and with microscope findings, the pathologist arrives at a definitive diagnosis. Sometimes, the pathologist may perform special studies, which may include immunohistochemical stains, histochemical stains, molecular testing and very rarely electron microscopic studies. Examination of the biopsy under a microscope by a pathologist is considered to be gold standard in arriving at a conclusive diagnosis
Many clinical conditions may have similar signs and symptoms. Your healthcare provider may perform additional tests to rule out other clinical conditions to arrive at a definitive diagnosis.
What are the possible Complications of Seminoma of Testis?
The complications due to Seminoma of Testis may include:
- Infertility, depending on the type of treatment given
- Retrograde ejaculation, if nerves are damaged during the surgery
- There may be a rapid growth of the tumor, which may invade into surrounding tissues causing tissue damage
- The tumor may recur after surgical excision, if it is incompletely removed
- Sometimes by the time Testicular Seminoma is detected, it is likely that it has grown and metastasized aggressively, damaging organs and tissues beyond repair
- Deep-seated tumors (those buried in the body tissues), may create problems for adjoining tissues and organs by compressing them (due to mass effect of the tumor)
- Blood loss during invasive treatment methods may be heavy
- Complications of chemotherapy and radiation therapy, such as anemia, leucopenia, increased susceptibility to infections, and hair loss may occur
- Inadvertent damage of vital nerves, blood vessels, and surrounding structures during surgery may occur depending on the location of the tumor in the body (apart from the testicles). Some tumors, which are away from the vital organs, can be removed usually with no significant damage. However, some tumors may grow close to vital organs and structures, which makes their surgical removal difficult and challenging
- Sometimes tumor can metastasize to other regions of the body. Extensive metastasis may give rise to extensive bleeding resulting in a fatality. Frequent sites of metastasis are the lungs, lymph nodes, liver, and bones
How is Seminoma of Testis Treated?
A combination of chemotherapy (drugs), radiation therapy, and surgery may be employed by the healthcare provider. However, Seminoma of Testis is mainly treated by radiation therapy during the early stages. The treatment may also involve:
- The surgical removal of the testis with the biopsy of draining lymph nodes. The surgery may involve radical inguinal orchiectomy (removal of the testis), with biopsy of lymph nodes within the abdomen (termed retroperitoneal lymph node dissection or RPLND), and removal of other tissues in the pelvis and abdomen, as needed
- If needed, omentectomy (removal of fat around the intestines) may be performed
- Debulking surgery to reduce tumor mass followed by chemotherapy. Since Testicular Seminoma is highly-resistant to chemotherapy, the debulking procedure helps the chemotherapy treatment to be more effective, because there is less tumor mass for the drugs to act on
- Removal of tumor as much as possible (called debulking procedure) is performed before chemotherapy in advanced stages of tumor development
- Surgical removal of the metastatic tumors followed by radiation and chemotherapy
- Palliative therapy, in cases where curative treatment and care is not possible
- Post-operative care is important: One must maintain minimum activity levels, until the surgical wound heals
- Post-operative follow-up care with regular screening and check-ups are important, especially to monitor for any recurrences
How can Seminoma of Testis be Prevented?
Presently, there is no method to completely prevent the occurrence of Seminoma of Testis. However, the chances of its occurrence can be reduced by:
- Screening for undescended testis and performing corrective surgery or removal of testis, as necessary
- Monthly testicular self-examination after puberty is recommended to diagnose testicular tumors in its early stages
- Eliminating the modifiable risk factors helps in the prevention of Testicular Seminoma. These factors include quitting smoking, avoiding pesticides and chemical carcinogens, in general
- Genetic testing of the expecting parents (and related family members) and prenatal diagnosis (molecular testing of the fetus during pregnancy) may help in understanding the risks better during pregnancy
- If there is a family history of the condition, then genetic counseling will help assess risks, before planning for a child
- Regular medical screening at periodic intervals with blood tests, scans, and physical examinations, are mandatory to prevent recurrence for those who have already endured the tumor
What is the Prognosis of Seminoma of Testis? (Outcomes/Resolutions)
Germ cell cancers of testicle, such as Seminoma of Testis, usually have better prognosis than testicular cancers. The prognosis of Testicular Seminoma depends upon:
- The stage of the tumor
- The size of the tumor
- Age of the individual
- Overall health of the individual
- Tumor stage at detection
- Location of the tumor
- Number of masses of tumors within the testicle
- Presence of metastasis and the organs involved with metastasis
- Its ki-67 value - a protein found in cells that is a good indicator of how fast the tumor cells are growing. The ki-67 value is determined by a pathologist and is usually mentioned in the pathology report
A complete excision usually results in a low tumor recurrence. Testicular Seminoma often requires several years of follow up and active vigilance.
- The prognosis is excellent when the tumors are small and found below the testicular surface. Such tumors have a very low recurrence risk after complete surgery removal
- This kind of tumor is also known to have a very good cure rate after surgical excision and chemotherapy, even in advanced cases, wherein the tumor has metastasized to distant lymph nodes or lungs
Additional and Relevant Useful Information for Seminoma of Testis:
- Under the microscope, Seminoma of Testis consists of uniform cells of clear cytoplasm, large nucleus, and well-defined cellular border. It is always accompanied by normal serum alpha protein levels
- The gene chip assays can identify multiple mutations in the tumor and help physicians decide on the best course of treatment
- There are many online groups available for individuals diagnosed with Germ Cell Neoplasia of Testis that provide supportive care, encouragement, and bring a measure of relief to the affected individuals and their families
Related Articles
Test Your Knowledge
Asked by users
Related Centers
Related Specialties
Related Physicians
Related Procedures
Related Resources
Join DoveHubs
and connect with fellow professionals

0 Comments
Please log in to post a comment.