What are the other Names for this Condition? (Also known as/Synonyms)
- Diffuse-Type Giant Cell Tumor (D-TGCT)
- Extraarticular Pigmented Villonodular Tenosynovitis
- PVNS (Pigmented Villonodular Synovitis)
What is Pigmented Villonodular Synovitis? (Definition/Background Information)
- Pigmented Villonodular Synovitis (PVNS) is an extremely infrequent, soft tissue tumor. It involves the joint fluid sac, tendon sheath, and synovial membrane of the joints
- Synovial fluid is the lubricating fluid found in the joints (like knee, elbow), and synovium refers to the thin membrane that lines or covers the joint space
- PVNS is generally a large and firm tumor. It frequently affects the knee followed by the hip, and can exhibit pronounced symptoms. It can rarely metastasize. It has a very high chance of recurrence after surgical removal. Hence, this condition is considered to be of low-grade malignancy
- The treatment of choice is a surgical removal of the entire tumor, followed by radiation therapy. The prognosis is generally excellent, when the tumor is completely removed
Who gets Pigmented Villonodular Synovitis? (Age and Sex Distribution)
- Pigmented Villonodular Synovitis normally affects individuals, below the age of 40 years. However, a wide age range is seen
- There is a slight female predominance
- No ethnic or racial preference is seen
What are the Risk Factors for Pigmented Villonodular Synovitis? (Predisposing Factors)
No clear risk factors have been established. Nevertheless, the following conditions are thought to be associated with Pigmented Villonodular Synovitis, in some way:
- Degenerative disorders of the joints - many cases of PVNS are noted with this condition
- In some specimens, chromosomal aberrations have been found
It is important to note that having a risk factor does not mean that one will get the condition. A risk factor increases ones chances of getting a condition compared to an individual without the risk factors. Some risk factors are more important than others.
Also, not having a risk factor does not mean that an individual will not get the condition. It is always important to discuss the effect of risk factors with your healthcare provider.
What are the Causes of Pigmented Villonodular Synovitis? (Etiology)
- The exact cause and mechanism of Pigmented Villonodular Synovitis formation is unknown
- Some of the theories proposed relate to - abnormal cell growth conditions and genetic defects
- However, the generally accepted theory is that PVNS might form as a reactive process to an injury-related inflammation, causing an uncontrolled cell proliferation
What are the Signs and Symptoms of Pigmented Villonodular Synovitis?
The presentations are based on the location of the tumor. Pigmented Villonodular Synovitis signs and symptoms include:
- In the initial growing phase, these superficial lesions (those which are located below the skin surface) are asymptomatic
- The soft tissue tumors grow at an extremely slow rate. They are firm or pliable and may grow to a large size; they are also poorly defined
- The inflamed tumor may present pain and feeling of tenderness, with locally impaired function (of the adjoining organs), if the tumor is big. Inconvenience with limited joint motion range or pain, may be seen as the tumor slowly increases in size
- Joint instability with or without joint locking; which include joint pain, swelling, and joint stiffness
- The knee (in 75% of the cases) and hip (in 15% of the cases) are usual sites for PVNS, followed by the shoulder, elbow, and ankle. The tumors are mostly observed around the joints and bones
- The least affected areas are the finger, wrist, toe, and groin region. In some very rare cases, the buttocks and abdominal cavity have also been affected
How is Pigmented Villonodular Synovitis Diagnosed?
A diagnosis of Pigmented Villonodular Synovitis is made using the following tools:
- Physical exam with evaluation of medical history
- MRI scan of the tumor site
- Ultrasound studies
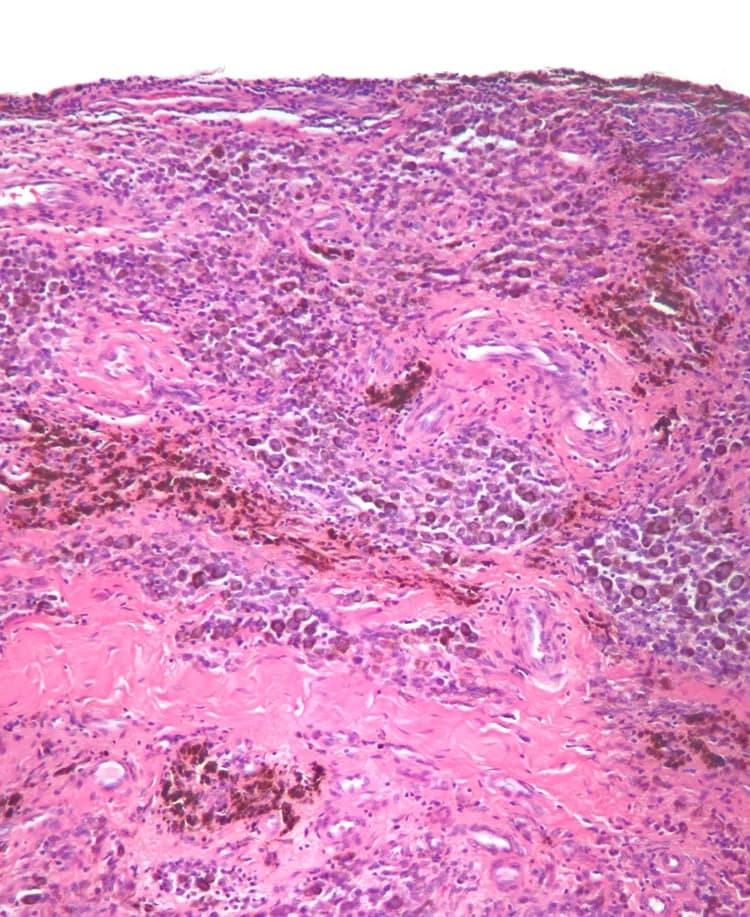
- Histopathological studies conducted on a biopsy specimen - the specimen is examined under a microscope by a pathologist, to arrive at a definitive diagnosis
- Joint aspiration of the synovial fluid. In case of PVNS, the joint fluid is often bloody
- Differential diagnosis, to eliminate other tumor types should be considered before arriving at a definitive diagnosis
Many clinical conditions may have similar signs and symptoms. Your healthcare provider may perform additional tests to rule out other clinical conditions to arrive at a definitive diagnosis.
What are the possible Complications of Pigmented Villonodular Synovitis?
Complications are dependent on the site and severity of Pigmented Villonodular Synovitis. These include:
- PVNS may have infiltrated into adjoining tissues and muscles
- Metastasis is rare, but if it occurs, then this may affect the lungs and lymph nodes. The tumor may invade into the adjoining cartilage and bone, causing them to degenerate
- The mobility of the joints can be constrained and lead to difficulty in walking and performing normal daily activities, thereby affecting the quality of life
- Damage of the knee, hip, or elbow, or other organs, vital nerves, and blood vessels, during surgery
- PVNS is known to having a medium to high recurrence rate (between 18-50%), after surgical excision and removal. Often multiple surgeries may be required to eliminate the tumor completely
How is Pigmented Villonodular Synovitis Treated?
Treatment measures for Pigmented Villonodular Synovitis include the following:
- Wide surgical excision of PVNS with removal of the entire tumor, followed by radiation therapy, remains the standard treatment mode. If the tumor is not fully removed, then it has a high probability of recurrence
- In some cases skin grafting and tendon reconstruction may be required
- Total joint replacement is a treatment modality for advanced PVNS
- When it is unsafe to surgically remove the lesion on account of weak health condition of the individual, non-invasive procedures (like radiotherapy) are adopted
- Post-operative care is important: A minimum activity level is to be ensured, until the surgical wound heals
- Follow-up care with regular screening and check-ups are important to watch for any recurrences and metastatic behavior. Often several years of active vigilance is necessary
How can Pigmented Villonodular Synovitis be Prevented?
- Current medical research has not established a way of preventing Pigmented Villonodular Synovitis occurrence. It is mainly managed through surgical intervention procedures
- Regular medical screening at periodic intervals with blood tests, radiological scans, and physical examinations, are mandatory for those who have been diagnosed with the tumor
- Due to its high chances of recurrence, often several years of active follow-up vigilance is necessary
- The recurrence risk may be compounded by the presence of other degenerative bone diseases and external injuries
What is the Prognosis of Pigmented Villonodular Synovitis? (Outcomes/Resolutions)
- The prognosis is generally excellent with surgical intervention - which is on a complete removal of the lesion, even if they are deep-seated. Pigmented Villonodular Synovitis recurrence risk is dependent on the effectiveness of the surgery
- Multiple recurrences are possible with PVNS - the recurrence risk being dependent upon the tumor location. It is observed that the tumor occurring within a joint, has a lower recurrence rate, than tumors that occur outside the joint
- PVNS is known to have a metastatic potential and can change into a dangerous sarcoma. However, this is an infrequent occurrence
Additional and Relevant Useful Information for Pigmented Villonodular Synovitis:
There are two types of Pigmented Villonodular Synovitis tumors, namely:
- Localized type of Pigmented Villonodular Synovitis: When pain and swelling affect a focal area of a joint, it is called Localized PVNS. These tumors are more easily treated
- Diffuse type of Pigmented Villonodular Synovitis: When the tumor affects the entire joint, it is called Diffuse PVNS
Related Articles
Test Your Knowledge
Asked by users
Related Centers
Related Specialties
Related Physicians
Related Procedures
Related Resources
Join DoveHubs
and connect with fellow professionals

0 Comments
Please log in to post a comment.