Glaucoma
What are the other Names for this Condition? (Also known as/Synonyms)
- Acquired Glaucoma
- Angle Closure Glaucoma
- Tunnel Vision due to Glaucoma
What is Glaucoma? (Definition/Background Information)
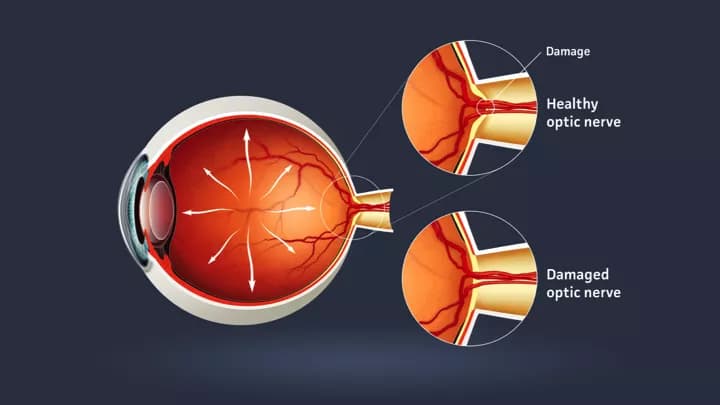
- Glaucoma is a group of eye disorders in which the optic nerves connecting the eyes and brain are progressively damaged, leading to reduced peripheral vision and potential blindness
- This condition is usually caused by increased pressure within the eyes, known as intraocular pressure (IOP), which is dependent upon a balance between the fluid that is entering and leaving the eyes
- Individuals with Glaucoma have clear vision in the central area; but, the side or peripheral vision is lost. The complications of untreated Glaucoma include blind spots in the peripheral vision, tunnel vision, and total blindness
- The treatment of Glaucoma depends on the type of Glaucoma and response to treatment. In general, individuals with Glaucoma who responds to treatment have a better prognosis than those who do not respond
There are various types of Glaucoma:
- Primary Open Angle Glaucoma: This is the most common type of Glaucoma, which is usually adult-onset, affecting both the eyes (Bilateral Glaucoma). It is estimated that 1% of individuals over 40 years have Primary Open Angle Glaucoma
- Adults: Progressive optic neuropathy that occurs with IOPs greater than 21 mm Hg
- Congenital: Port-wine stain
- Secondary Open Angle Glaucoma:
- Psuedoexfoliation Syndrome
- Pigmentary Dispersion Syndrome
- Primary Angle-Closure Glaucoma:
- Pupillary Block
- Plateau Iris Syndrome
- Secondary Angle-Closure Glaucoma:
- Neovascular Glaucoma
- Uveitic Glaucoma
- Inflammatory Glaucoma:
- Glaucomatocyclitic Crisis
- Fuch’s Heterochromic Iridocyclitis
- Traumatic Glaucoma (Angle Recession Glaucoma)
- Normal Tension Glaucoma
- Steroid-Induced Glaucoma
Who gets Glaucoma? (Age and Sex Distribution)
- Generally, individuals over the age of 40 are affected by Glaucoma; although, any individual is prone to the condition
- Both male and female sexes are affected by this eye disorder
- African Americans are most likely to develop Primary Open Angle Glaucoma
- East Asians are most likely to develop Normal Tension Glaucoma
What are the Risk Factors for Glaucoma? (Predisposing Factors)
The risk factors of Glaucoma include:
- All individuals over the age of 40 years are at risk of developing Glaucoma; however, in the case of African-Americans, the risk begins at a much younger age
- Individuals belonging to Afro-American or East Asian communities
- Ethnic background: East Asians have a shallow anterior chamber and because of this inborn structure, they seem to develop Glaucoma a lot easier than others
- Hereditary factor: If several family members suffer from Glaucoma, then family members of subsequent generations are also likely to be susceptible to the condition
- Diabetes: All diabetic patients carry an increased risk
- High Myopia: Patients, who suffer from high myopia, or nearsightedness, are at an increased risk
- Any previous eye injury or eye infection may be a cause for increasing the risk percentage
- Hypertension: Individuals with hypertension or high blood pressure are at a slightly increased risk
- Corticosteroids treatment: Patients, who have been prescribed corticosteroids, have a higher risk of developing Glaucoma
- Thin corneas: Patients with thinner corneas than average can have higher IOPs, which increases the risk for Glaucoma.
It is important to note that having a risk factor does not mean that one will get the condition. A risk factor increases ones chances of getting a condition compared to an individual without the risk factors. Some risk factors are more important than others.
Also, not having a risk factor does not mean that an individual will not get the condition. It is always important to discuss the effect of risk factors with your healthcare provider.
What are the Causes of Glaucoma? (Etiology)
- Glaucoma is an eye disease in which the fluid cannot drain properly, causing the pressure inside the eye to rise. This can lead to damage of the optic nerve
- A clear liquid, called aqueous humor, flows in and out of the anterior chamber - a small space in front of the eye. This fluid nourishes the nearby tissues, enabling proper vision
- But, when the balance between the inflow and outflow of fluid is affected, and when the fluid does not drain properly, the fluids build up inside the eye. This increase of intraocular pressure (IOP) damages the optic nerves and other parts of the eye, leading to loss of peripheral vision and potential blindness
- There are different types of Glaucoma and scientists have classified them as follows:
- Whether the Glaucoma is congenital or acquired
- Whether it is open-angle or closed-angle, depending on how the above-mentioned aqueous humor outflow is affected
- Whether the underlying cause for Glaucoma can be determined. It is called Primary Glaucoma, when the cause is unknown and Secondary Glaucoma, when the underlying cause is known
The following are the common causes of Glaucoma:
- Failure of the eye to maintain a proper balance between the amount of intraocular fluid produced and the amount that drains away
- Decreased blood flow to the optic nerve
- Poor blood flow within the eye
- Buildup of beta-amyloid protein in the eyes and in brain tissues
What are the Signs and Symptoms of Glaucoma?
The signs and symptoms differ for Open-Angle Glaucoma and Closed-Angle Glaucoma.
The signs and symptoms for Primary Open-Angle Glaucoma include:
- Both the eyes are affected, and the affected individual gradually loses his/her peripheral vision
- In extreme or severe cases, the affected individual experiences tunnel vision
The signs and symptoms of Closed-Angle Glaucoma include:
- Severe eye pain
- Blurred vision
- Eye pain that is accompanied by nausea and vomiting
- Lights appear to have a halo-like glow around them
- Red eyes
- Sudden eye problems, especially under poor lighting
How is Glaucoma Diagnosed?
The following tests are conducted to diagnose Glaucoma:
- Physical examination with complete medical (and family) history
- Eye pressure test: The physician uses an instrument, called a tonometer, to measure the intraocular pressure
- The corneal thickness is also measured to obtain a corneal-corrected IOP. Thinner corneas tend to underestimate the true IOP, which increases the risk for Glaucoma. Thicker corneas tend to overestimate the true IOP, which decreases the risk for Glaucoma
- Gonioscopy: The area where the fluid drains out of the eye is checked to determine whether there is a block in the angle between the cornea and iris
- Perimetry test or visual field test: This is done to check the individual’s peripheral vision. Specific visual field defects are consistent with glaucomatous damage to the optic nerve
- Optic nerve damage assessment: An ophthalmologist uses instruments to see the back part of the eye (optic disc examination), in order to determine if either optic nerve has been damaged, which can be taken as a sign of Glaucoma-onset
- Ocular Coherence Tomography (OCT): an instrument used to scan the optic nerve to measure the thickness of the nerve fiber layer. This assesses if there has been any thinning of the nerve fiber layer, which correlates to optic nerve damage
Many clinical conditions may have similar signs and symptoms. Your healthcare provider may perform additional tests to rule out other clinical conditions to arrive at a definitive diagnosis.
What are the possible Complications of Glaucoma?
Glaucoma, if left untreated, may lead to the following complications:
- Blind spots in the peripheral vision
- Tunnel vision
- Total blindness
How is Glaucoma Treated?
There is no permanent cure for Glaucoma; nevertheless, regular check-ups and treatments, as advised by the physician, can keep the condition under control. The treatment for Glaucoma is aimed at improving the flow of fluid inside the eye and/or reducing its production.
The treatment measures that are planned by the healthcare provider may include:
- The use of eye drops such as:
- Prostaglandin analogues: This contains prostaglandin-like compounds as active ingredients, which help in increasing the outflow of the fluid inside the eye
- Beta blockers: This reduces fluid production in the eye
- Alpha agonists: This increases outflow and decreases production of fluid in the eye
- Patients with asthma or lung conditions, such as emphysema or bronchitis, may be given a different medication
- Diabetes patients, who are taking insulin, may also be given an alternative drug
- Carbonic anhydrase inhibitors: These help in reducing the fluid production in the eye
- Cholinergic agents or miotic agents: They help in the movement of fluid out of the eye
Surgery becomes essential for patients who are non-compliant with their drops or do not respond to the above treatments and medications. The purpose of surgical intervention is to bring down the pressure inside the eye. Surgical interventions may include:
- Trabeculoplasty: High-energy laser beams (such as argon laser trabeculoplasty and diode laser trabeculoplasty) are used to remove the blocks in the drainage canals, allowing for the free flow of liquids
- Filtering surgery (trabeculectomy): The surgeon creates an opening in the white of the eye and removes a small piece of the trabecular meshwork, which allows the eye fluid to leave through the opening. This can be performed using a surgery called Nd:YAG laser iridotomy
- Drainage implant (aqueous shunt implant): This is generally used for children or patients with Secondary Glaucoma. A small silicon tube is inserted into the eye to drain out the fluids
Management of Acute Angle Closure Glaucoma:
- This condition is treated as a medical emergency
- Pressure reducing medications are administered immediately
- A laser procedure is done to create a hole in the iris, allowing fluids to pass into the trabecular meshwork; this procedure is called laser iridotomy
The treatment of Glaucoma using medications and eye drops may cause certain side effects. These could include:
- Side effects of eye drops, such as prostaglandin analogues, include:
- Reddening and stinging of the eyes
- Swelling around the rim of the eye
- Photophobia, blurred vision
- Darkening of the iris; change in the color of the eyelids
- Side effects of eye drops, such as beta blockers, include:
- Breathing problems, fatigue
- Drop in blood pressure
- Hair loss
- Depression, memory loss
- Impotence
- Side effects of medications, such as carbonic anhydrase inhibitors, include:
- Nausea
- Eye irritation
- Dry mouth, strange taste in the mouth
- Frequent urination
- Tingling in the fingers and toes
- Side effects of medications, such as cholinergic agents or miotic agents, include:
- Pain in and around the eye; ache around the eyebrows
- Myopia, blurred vision
- Blocked nose
- Digestive problems
- Increased sweating and salivation
- Side effects of medications, such as sympathomimetic drugs (alpha agonists), include:
- Painful red eye
How can Glaucoma be Prevented?
The following preventive measures may be used to minimize the risk of Glaucoma:
- Regular eye examination: A regular checkup with an ophthalmologist or optometrist helps in the early detection of Glaucoma-onset; also, this can help prevent any further complications. It is generally recommended that a dilated fundus examination be performed every year for individuals over 50 years of age
- Treat elevated eye pressure: Glaucoma eye drops are very effective in reducing the risk of Glaucoma development. These eye drops should be used regularly, even when there are no symptoms
- Control body weight and blood pressure: Research has revealed that hypertension and obesity are closely linked with elevated intraocular pressures
- Wear eye protection gear: Serious injury or trauma to the eye may lead to Glaucoma. It is always recommended to wear protective gears while using power tools or while playing high speed racket sports, so as to minimize the risk of being hit in the eye
What is the Prognosis of Glaucoma? (Outcomes/Resolutions)
The prognosis of Glaucoma depends on the type and severity:
- Open-Angle Glaucoma cannot be cured, but regular consultation with an ophthalmologist or optometrist and an eye examination can put arrest to further complications
- Primary Open Angle Glaucoma can be graded according to severity of signs and symptoms:
- Mild Primary Open Angled Glaucoma: The individual has early visual field defects on a perimetry test or visual field test. The prognosis is usually excellent with early detection and treatment
- Moderate Primary Open Angled Glaucoma: The individual has a presence of specific findings by the eye specialist called arcuate scotoma (abnormal visual field loss, which affects the central visual field on a perimetry test or visual field test) and thinning of an area called the neuroretinal rim in the back of the eye on an optic disc examination. The prognosis can be excellent with early detection and treatment
- Severe Primary Open Angled Glaucoma: The individual has significant visual field loss on a perimetry test or visual field test and marked thinning of the neuroretinal rim in the back of the eye on an optic disc examination. The prognosis can be good with early detection and treatment
- End-Stage Primary Open Angled Glaucoma: The individual has a presence of only small residual visual field on a perimetry test or visual field test, and there may be very little neuroretinal rim remaining in the back of the eye on a optic disc examination. The prognosis is poor in spite of treatment
- Angle Closure Glaucoma is treated as a medical emergency; treatment should be immediately provided to save vision
- Babies with Congenital Glaucoma cure well, when early surgery is performed
- The recovery of individuals affected with Secondary Glaucoma depends on the severity of the condition
Additional and Relevant Useful Information for Glaucoma:
The following DoveMed website link is a useful resource for additional information:
Related Articles
Test Your Knowledge
Asked by users
Related Centers
Related Specialties
Related Physicians
Related Procedures
Related Resources
Join DoveHubs
and connect with fellow professionals

0 Comments
Please log in to post a comment.