Double Stem-Cell Transplant Improves Outcomes for Children With High-Risk Neuroblastoma
CHICAGO – Historically, less than 50% of children with high-risk neuroblastoma live five or more years after diagnosis. A National Cancer Institute (NCI) funded phase III trial performed by the Children’s Oncology Group found that adding a second autologous stem-cell transplant (ASCT, a transplant that uses the patient’s own stem cells) to standard therapy improves outcomes for these patients.
At 3 years, 61.4% of patients who received a double transplant were alive and cancer-free, compared to 48.4% of those who received a single transplant. Side effects were similar between single and double transplant.
These data will be presented in ASCO’s Plenary Session, which features 4 abstracts deemed to have the greatest potential to impact patient care, out of the more than 5,000 abstracts featured as part of the ASCO Annual Meeting.
“This finding will change the way we treat children with high-risk neuroblastoma in North America, which still claims many young lives and is in urgent need of better treatments,” said lead study author Julie R. Park, MD, an attending physician at Seattle Children’s Hospital and professor in pediatrics at the University of Washington School of Medicine in Seattle, Washington. “However, the regimen we use for high-risk neuroblastoma is also the most aggressive and toxic regimen we give to children with cancer. For that reason, future research needs to focus on both exploring possible lateeffects of current therapy and developing newer less toxic therapies.”
About the Study
The trial enrolled children newly diagnosed with high-risk neuroblastoma, who were a median age of 3.1 years. The majority of patients (88%) had Stage 4 disease and 38.2% had a tumor high-risk genetic abnormality called MYCN amplification.
All patients received 6 cycles of a multi-agent induction chemotherapy regimen including an initial 2 cycles of high-dose cyclophosphamide/topotecan followed by collection of stem cells from the blood to be used for subsequent transplantation. At completion of the induction therapy, patients were randomly assigned to receive a single ASCT with carboplatin-etoposide-melphalan (CEM) chemotherapy or a double (tandem) ASCT with thiotepa–cyclophosphamide prior to the first ASCT followed by a modified CEM chemotherapy prior to second ASCT. In the tandem ASCT group, patients received the two transplants in the span of 6 to 8 weeks.
In the single ASCT group, 129 out of 179 patients were subsequently enrolled onto a trial delivering anti-GD2 (dinutuximab) plus cytokine immunotherapy after single transplant consolidation therapy. A similar proportion of patients, 121 out of 176, received this immunotherapy following a tandem transplant consolidation therapy.
The primary endpoint of the study was 3-year event-free survival (EFS) or the percentage of patients who have not had an “event” at three years after randomization. An “event” was defined as worsening or recurrence of cancer, diagnosis of a second cancer, or death from any cause.
Key Findings
Among all patients on the study, the 3-year EFS from enrollment was 51% and 3-year overall survival (OS) was 68.3%. Among patients randomized, the 3-year EFS rate from time of randomization was significantly higher following tandem transplant (61.4%) compared to single transplant (48.4%). The 3-year overall survival rate was slightly higher in the tandem transplant group than the single transplant group (74% vs. 69.1%), but the difference was not statistically significant.
“We know that most neuroblastoma recurrences occur within two to three years from diagnosis and that patients who had not had a recurrence at three years have a better chance of long-term survival. The study was not designed to observe a difference in overall survival, as this would take many years and can not be adequately controlled for additional therapies received after an initial disease recurrence,” said Dr. Park. The researchers will continue following patients on this study for 10 years.
Outcomes were generally better among patients who enrolled onto the immunotherapy trial that included anti-GD2 antibody plus cytokines after the transplant. Among those patients, the 3-year EFS rate was significantly higher for those who had been assigned to tandem transplant (73.2%) compared to those assigned to single transplant (55.5%). The 3-year overall survival rate was significantly higher with a tandem transplant than with a single transplant (85.6% vs. 75.8%).
The rates of severe toxicities were similar between treatment groups. Fewer treatment-related deaths occurred among patients who received a tandem transplant than among those who received a single transplant (2 vs. 8).
About Neuroblastoma
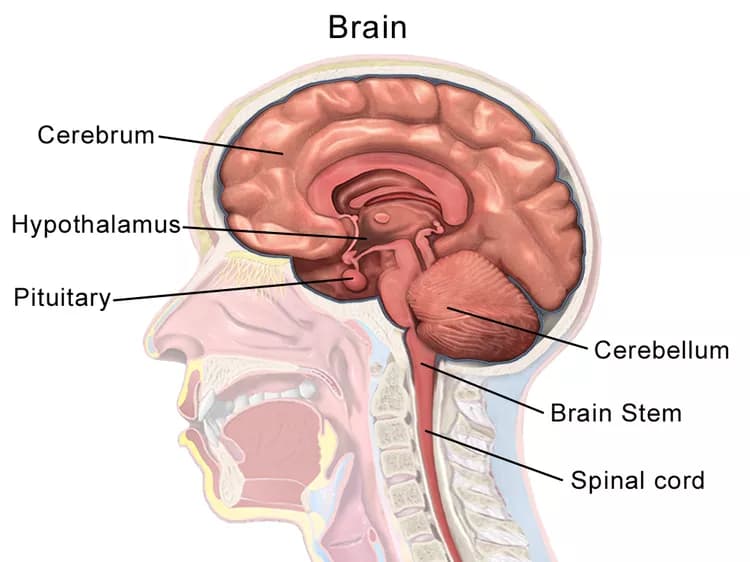
Neuroblastoma is a tumor that begins in nerve cells outside of the brain. Although neuroblastoma is a rare cancer overall, with only 700 new diagnoses per year in the United States, it is the second most common solid tumor in children and the most common cancer in infancy.1 Neuroblastoma most often occurs in children younger than six years.
A combination of clinical, pathologic and genetic markers is used to define neuroblastoma. Children with high-risk neuroblastoma usually receive an intensive treatment regimen, which may include surgery, chemotherapy, radiation therapy, and/or stem-cell transplantation.
The study received funding from the National Institutes of Health and was performed through the Children’s Oncology Group consortium.
View the full abstract.
Related Articles
Test Your Knowledge
Asked by users
Related Centers
Related Specialties
Related Physicians
Related Procedures
Related Resources
Join DoveHubs
and connect with fellow professionals

0 Comments
Please log in to post a comment.