What are the other Names for this Test? (Equivalent Terms)
- Anti-Factor Xa Heparin Blood Test
- Heparin Level Blood Test (see Heparin Anti-Xa Blood Test)
- Xa Inhibition Blood Test
What is Heparin Anti-Xa Blood Test? (Background Information)
- Heparin is an anticoagulant drug that both prevents and treats internal blood clots (thromboses). Levels of heparin in blood may be indirectly monitored by measuring inhibition of clotting factor Xa
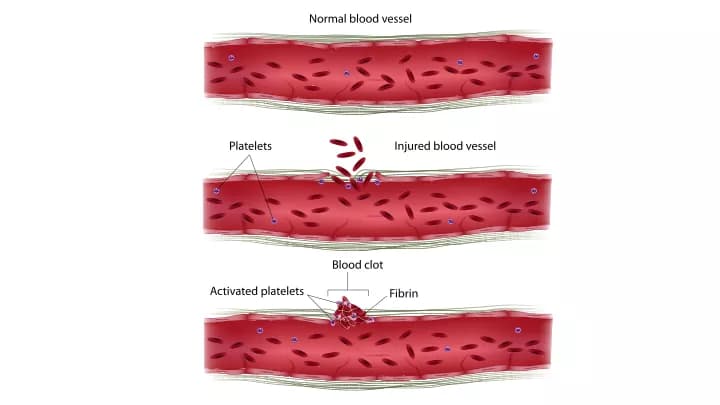
- Clotting factors are proteins that help form blood clots at the site of blood vessel injury. ‘Factor Xa’ is one of twelve such factors. Blood clots stop blood loss and allow the blood vessel to continue functioning
- Injury to a blood vessel causes the blood vessel to constrict. Called the vascular phase, this is the first reaction of a blood vessel to any damage of injury. It reduces the flow of blood to the site of injury, minimizing blood loss
- Next, circulating platelets clump along the site of the blood vessel injury. Platelets form a foundation for a blood clot and release chemicals that stimulate clotting
- The coagulation phase then causes a blood clot to form. Clotting occurs when an enzyme called thrombin converts a soluble protein, fibrinogen, into its insoluble form, fibrin. Fibrin proteins make up the bulk of a blood clot
- A counter pathway ensures that the size of the growing blood clot stays in check. Problems with this regulatory pathway may lead to a dangerous condition, where blood clots form within the blood vessels (called thrombosis). Antithrombin (a type of protein) inactivates factor Xa, as well as thrombin and other compounds, and is essential in keeping the clotting process under control
Heparin acts as an anticoagulant by drastically increasing the activity of antithrombin. There are two types of heparin:
- Low molecular weight heparin (LMWH): Typically administered via injections under the skin, it is made up of smaller heparin molecules. It has a narrower range of function and is more predictable
- Unfractionated heparin (UFH): Administered intravenously, UFH is made up of various types of heparin. It is less predictable and levels must be closely monitored using the partial thromboplastin time (PTT) and activated clotting time (ACT) blood tests
The Heparin Anti-Xa Blood Test indirectly measures heparin levels by assessing inactivation of clotting factor Xa by antithrombin. It is used to ensure that heparin levels stay within an acceptable range.
What are the Clinical Indications for performing the Heparin Anti-Xa Blood Test?
Clinical indicators for performing the Heparin Anti-Xa Blood Test include monitoring heparin therapy.
How is the Specimen Collected for Heparin Anti-Xa Blood Test?
Following is the specimen collection process for Heparin Anti-Xa Blood Test:
Sample required: Blood
Process of obtaining blood sample in adults:
- A band is wrapped around the arm, 3-4 inches above the collection site (superficial vein that lies within the elbow pit)
- The site is cleaned with 70% alcohol in an outward spiral, away from the zone of needle insertion
- The needle cap is removed and is held in line with the vein, pulling the skin tight
- With a small and quick thrust, the vein is penetrated using the needle
- The required amount of blood sample is collected, by pulling the plunger of the syringe out slowly
- The wrap band is removed, gauze is placed on the collection site, and the needle is removed
- The blood is immediately transferred into the blood container, which has the appropriate preservative/clot activator/anti-coagulant
- The syringe and the needle are disposed into the appropriate “sharp container” for safe and hygienic disposal
Preparation required: No special preparation is needed prior to the test.
What is the Significance of the Heparin Anti-Xa Blood Test Result?
Excessive heparin anti-Xa levels may indicate that:
- Too much heparin is being administered
- Or, the individual is processing heparin more slowly than expected
The laboratory test results are NOT to be interpreted as results of a "stand-alone" test. The test results have to be interpreted after correlating with suitable clinical findings and additional supplemental tests/information. Your healthcare providers will explain the meaning of your tests results, based on the overall clinical scenario.
Additional and Relevant Useful Information:
- The Heparin Anti-Xa Blood Test is not entirely standardized. Thus, different laboratories may come up with different results, which may not be interchangeable (across the labs)
Certain medications that you may be currently taking may influence the outcome of the test. Hence, it is important to inform your healthcare provider, the complete list of medications (including any herbal supplements) you are currently taking. This will help the healthcare provider interpret your test results more accurately and avoid unnecessary chances of a misdiagnosis.
Please visit our Laboratory Procedures Center for more physician-approved health information:
http://www.dovemed.com/common-procedures/procedures-laboratory/
Related Articles
Test Your Knowledge
Asked by users
Related Centers
Related Specialties
Related Physicians
Related Procedures
Related Resources
Join DoveHubs
and connect with fellow professionals

0 Comments
Please log in to post a comment.