What are the other Names for this Condition? (Also known as/Synonyms)
- Hypersomnia with Periodic Respiration
- Mixed Sleep Apnea
- Sleep Hypopnea
What is Sleep Apnea? (Definition/Background Information)
- Sleep Apnea is a cessation (stoppage) or near cessation of respiratory airflow lasting 10 seconds or longer during sleep. The term apnea indicates a pause in breathing
- There are three forms of Sleep Apnea:
- Central Sleep Apnea (CSA): It is the absence of breathing due to deficient brain activity
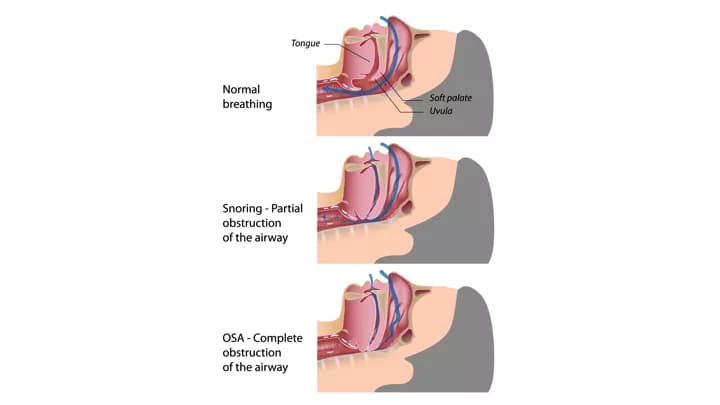
- Obstructive Sleep Apnea (OSA): It is the absence of respiratory airflow during sleep, despite respiratory effort, due to upper airway obstruction and snoring is commonly observed
- Complex Sleep Apnea
- Snoring, the lay term for obstructive breathing during sleep, is a widely prevalent phenomena. It is 3-times more common in obese individuals, than those who are less obese
- The most severe and exaggerated form of snoring, known as Obstructive Sleep Apnea, places the affected individual at increased risks for high blood pressure, heart attack, stroke, headaches, sexual impotence, and a diminished quality of life
- Spouses and roommates of the affected individuals may describe that with Obstructive Sleep Apnea there is not just snoring, but choking as well. They may describe a frightening struggle to breathe, while being asleep. After a number of seconds, a loud snort (resuscitative snort) occurs as the individual awakens and takes a breath again. Whereas, snoring means a partial obstruction of the airway; with apnea, there is a total obstruction
Who gets Sleep Apnea? (Age and Sex Distribution)
- Statistically, in a 30-35 year old population group - 20% of men and 5% of women may snore. By the age of 60 years - 60% of men and 40% of women may snore habitually
- Men tend to have Sleep Apnea much more frequently than women; the general accepted ratio is 10:1 (men to women)
What are the Risk Factors for Sleep Apnea? (Predisposing Factors)
Risk factors for Sleep Apnea include:
- Obstructive Sleep Apnea is common in individuals, who are overweight
- A family history of Sleep Apnea also increases the risk for this condition. Family traits that predisposes one to Obstructive Sleep Apnea, includes being overweight, diabetes, and various skeletal abnormalities that can cause obstruction of the airways
- Hypothyroidism also contributes to poor muscle tone, obstruction to breathing, and snoring
- Individuals suffering from neurological disorders that include cerebral palsy, myasthenia (an autoimmune disorder), and muscular dystrophy
- Space-occupying masses or tissues, impinging on the airways can contribute to snoring. In children, snoring is normally from enlarged tonsils and adenoids. Fat accumulation underneath the surfaces, causes narrowing of the air passageways
- Insufficient muscle tone of the palate, tongue, and pharynx, is the cause of most adult-onset snoring. In deep sleep stages, such muscles fail to participate in the breathing cycle, to open the airway during inspiration. This is exaggerated when an individual consumes alcoholic beverages or sedating medications, like sleeping pills, or antihistamines
- A large neck size puts you at risk for Sleep Apnea
It is important to note that having a risk factor does not mean that one will get the condition. A risk factor increases ones chances of getting a condition compared to an individual without the risk factors. Some risk factors are more important than others.
Also, not having a risk factor does not mean that an individual will not get the condition. It is always important to discuss the effect of risk factors with your healthcare provider.
What are the Causes of Sleep Apnea? (Etiology)
- In Central Sleep Apnea the brain's respiratory centers are imbalanced during sleep. The brain stem controls breathing. Conditions that can cause Central Sleep Apnea are stroke affecting the brain stem, heart failure, any irritation or injury to the brain stem, kidney failure, and neurological diseases, such as Parkinson's disease, Alzheimer's disease
- Chronic opiate use causes depression of respiratory center in the brain; hence, the respiratory centre does not react quickly enough, to maintain breathing
- Relaxation of muscles, during sleep, narrows the upper airway and air cannot flow into the lungs. Under normal conditions, this does not prevent the air from flowing. But, if the individual has Sleep Apnea, the throat muscles relax more than normal, preventing a proper flow
- Some individuals may experience mild Sleep Apnea during infection of the upper respiratory tract, like due to allergies, nasal congestion, and sinusitis
- It has been observed that occasional, brief apnea events are harmless; these are also quiet common in the normal adult population
- Individuals with a body mass index lower than 26 are unlikely to have moderate or severe Obstructive Sleep Apnea
What are the Signs and Symptoms of Sleep Apnea?
Signs and symptoms of Sleep Apnea include:
- Daytime sleepiness is a common feature with Sleep Apnea
- Individuals may admit to consistently falling asleep, while doing other activities like reading, watching television, or even while driving a vehicle
- Snoring is the other common feature of Obstructive Sleep Apnea
- Frequent urination during the night, is a common occurrence in those with moderate to severe Sleep Apnea
- Morning headaches, memory or learning problems, feeling irritable, depressed, and mood swings, are other signs and symptoms
How is Sleep Apnea Diagnosed?
A diagnosis of Sleep Apnea would involve:
- Physical examination with a good medical history: A general head and neck physical exam may help the physicians diagnose Sleep Apnea. Individuals may be questioned about their sleep habits and relevant history. They are recommended to maintain a ‘sleep diary’, which may help the physician evaluate, if there is a sleep disorder
- Polysomnography (sleep study) may be considered in all those, who are suspected of having Obstructive Sleep Apnea Syndrome, in order to verify the presence of the disorder and to determine its severity
- Usually, a consult with physicians’ specializing in sleep disorders is necessary
Many clinical conditions may have similar signs and symptoms. Your healthcare provider may perform additional tests to rule out other clinical conditions to arrive at a definitive diagnosis.
What are the possible Complications of Sleep Apnea?
Complications due to Sleep Apnea might include:
- High blood pressure, heart failure, heart attacks, impotence, and depression
- A diminished quality of life: Consequences of sleep deprivation could possibly include impaired intellectual function, social maladjustments, psychological depression, and motor vehicle accidents
How is Sleep Apnea Treated?
There are three categories of treatment options available to treat individuals with Sleep Apnea:
- Behavioral modification
- The use of devices
- Surgical options
Behavioral modification: Behavioral modifications principally include sleep position therapy, weight-loss (where appropriate), and the avoidance of sedatives, alcohol, and large meals, before bedtime.
- In sleep position therapy, individuals are advised to sleep on their sides or stomach, as opposed to sleeping on their backs, since obstructions occur more in the supine position
- Individuals are encouraged to lose weight, if they are overweight. Weight loss can help reduce the bulk of tissues in the neck that narrows the airway, and thus reduce airway collapse
Use of devices: Two devices are available to help maintain airway patency and reduce the incidence of sleep-disordered breathing. These include positive airway pressure and oral appliances.
- Continuous positive airway pressure (CPAP) provides positive pressure to the airway through a device worn on the face. CPAP keeps the upper airway passages open, preventing apnea. This is the most common treatment for moderate to severe Obstructive Sleep Apnea
- Bilevel positive airway pressure (BPAP) can be used for those, who are unable to adapt to CPAP. BPAP provides more pressure during inhalation, and less during exhalation
- Adaptive servo ventilation (ASV) is a new device that monitors the normal breathing pattern and saves the information in a computer. ASV prevents any pauses in the breathing. It can be useful in patients, who develop Central Apnea when treated with CPAP, as well as in those, who require medications that can suppress respiration. In individuals, who fail or do not tolerate CPAP, a trial of ASV is suggested
- Oral appliances, principally a mandibular repositioning device, can also be used for Sleep Apnea. This device advances the mandible anteriorly, which brings forward the tongue and other muscles of the throat
Surgical options: Surgical treatment appears to be most effective in patients, who have Obstructive Sleep Apnea, due to a severe, surgically correctable, obstructing lesion.
- Uvulopalatopharyngoplasty is one of the most common surgical procedures performed in this context. It involves a resection of the uvula, redundant retro-lingual soft tissue, and palatine tonsillar tissue
- Other common surgical procedures for Obstructive Sleep Apnea include:
- Septoplasty
- Rhinoplasty
- Nasal turbinate reduction
- Nasal polypectomy
- Tonsillectomy
- Tongue reduction
How can Sleep Apnea be Prevented?
- Weight-loss should be recommended in all individuals, who are overweight or obese. This is based on the evidence that weight loss improves overall health, decreases the apnea, improves quality of life, and probably decreases daytime sleepiness
- Sleeping in a non-supine position (e.g. lateral recumbent) may correct or improve Obstructive Sleep Apnea. Sleeping on ones’ back can cause the tongue and soft palate to rest against the back of the throat, blocking the airways
- Individuals are advised to maintain regular sleep hours and avoid alcohol, sedatives, sleeping pills, before bedtime, because they tend to relax the muscles of the throat
- In some cases, the use of a cervical pillow may help. Also, elevating the head of the bed by 4-6 inches, may prevent Sleep Apnea
- If you suspect that you may have Sleep Apnea, discuss the issue with your primary care physician, or a lung/sleep specialist
What is the Prognosis of Sleep Apnea? (Outcomes/Resolutions)
- There is high-quality evidence that positive airway pressure therapy reduces the frequency of Sleep Apnea and significantly improves both subjective and objective sleepiness, the quality of life, cognitive function, and depression
- Patients, who elect to be treated with positive airway pressure, should be evaluated frequently, especially during the first few weeks of therapy. This may be through frequent telephone calls and need-based opportunities to directly interact with the healthcare provider. Frequent evaluations may help in quickly identifying and managing any side effects that develop
- Once the patient's positive airway pressure therapy has been optimized and symptoms resolved, a regimen of long-term follow-up should be established. Annual visits are reasonable; with more frequent visits in between, if new issues arise. The purpose of long-term follow-up is to assess usage and monitor for recurrent Sleep Apnea, air leaks, and fluctuations in body weight
- The frequency of surgical follow-up is determined by the type of surgery, but should include assessment of wound healing, the anatomical result, side effects, and complications. Once the surgical team determines that the swelling has been resolved and healing is complete, the efficacy of the procedure should be assessed by enquiring whether the symptoms of Obstructive Sleep Apnea have resolved, and by performing a full sleep study
- If Sleep Apnea is left untreated, it can cause serious and life-threatening consequences, like heart disease, stroke, high blood pressure, and even motor vehicle accidents
Additional and Relevant Useful Information for Sleep Apnea:
Apnea of Prematurity is a disorder where there is stoppage (cessation) of breathing for more than 20 seconds in a premature/preterm infant, born before 34 weeks of gestation.
The following article link will help you understand Apnea of Prematurity.
http://www.dovemed.com/diseases-conditions/apnea-of-prematurity-aop/
Related Articles
Test Your Knowledge
Asked by users
Related Centers
Related Specialties
Related Physicians
Related Procedures
Related Resources
Join DoveHubs
and connect with fellow professionals

0 Comments
Please log in to post a comment.