What are the other Names for this Condition? (Also known as/Synonyms)
- Cutaneous Squamous Cell Carcinoma
- Dermal Squamous Cell Carcinoma
- SCC of Skin
What is Squamous Cell Carcinoma of Skin? (Definition/Background Information)
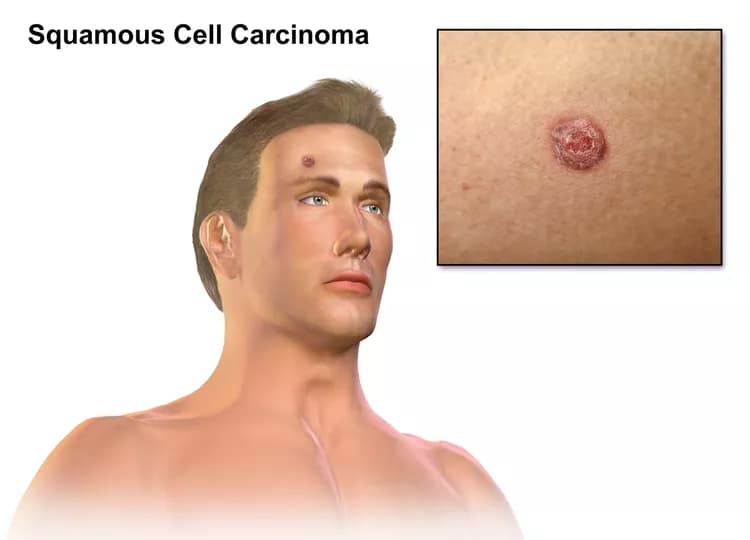
- Squamous Cell Carcinoma (SCC) of Skin is a common malignant tumor of skin that most commonly affects elderly men and women. It is also seen in many younger patients
- Prolonged exposure to the sun’s ultraviolet rays may result in damage of skin DNA causing the condition. Other factors that may influence its development include skin tanning, radiation treatment for other illnesses, previous burn injuries, and exposure to coal tar and arsenic
- Squamous Cell Carcinoma of Skin may appear as slow-growing skin lesions, commonly on the sun-exposed areas, such as the face, neck, hands, and even the chest. The lesions may ulcerate and cause scarring of skin
- The treatment of choice is a surgical excision with clear margins followed by radiation therapy or chemotherapy, as decided by the healthcare provider. In majority of the cases, the prognosis is excellent with appropriate treatment
- Nevertheless, the prognosis of Squamous Cell Carcinoma of Skin depends upon many factors including the stage of the tumor and health status of the affected individual. There is a possibility of local or regional metastasis, which can involve the lymph nodes. This may dictate the course of the condition
There are multiple types of Squamous Cell Carcinoma of Skin. These include:
- Acantholytic Squamous Cell Carcinoma of Skin
- Spindle Cell Squamous Cell Carcinoma of Skin
- Verrucous Squamous Cell Carcinoma of Skin
- Pseudovascular Squamous Cell Carcinoma of Skin
- Adenosquamous Carcinoma of Skin
Who gets Squamous Cell Carcinoma of Skin? (Age and Sex Distribution)
- Squamous Cell Carcinoma of Skin generally affects elderly or older adults; some cases rarely develop in children too
- It can occur in both males and females
- SCC of Skin is prevalent worldwide, though dark-skinned individuals (Asians and Africans) are affected less than lighter-skinned individuals (Europeans and Americans)
What are the Risk Factors for Squamous Cell Carcinoma of Skin? (Predisposing Factors)
The risk factors for Squamous Cell Carcinoma of Skin include:
- Exposure to intense sun for long periods during the course of work or due to regular participation in outdoor sports activities
- Frequent use of tanning beds, tanning parlors
- People living in geographical regions where hot-dry, desert-like climatic conditions prevail
- Radiation therapy
- Previous burn sites
- Arsenic exposure
- Coal tar exposure
- Smoking, tobacco chewing
- Individuals with weak immune system, which could be due to cancer treatment, AIDS, or those on immunosuppressant drugs after receiving an organ transplant
- Those with sensitive skin, who get easily sunburned
- Caucasians are more vulnerable compared to other darker-toned individuals
It is important to note that having a risk factor does not mean that one will get the condition. A risk factor increases one's chances of getting a condition compared to an individual without the risk factors. Some risk factors are more important than others.
Also, not having a risk factor does not mean that an individual will not get the condition. It is always important to discuss the effect of risk factors with your healthcare provider.
What are the Causes of Squamous Cell Carcinoma of Skin? (Etiology)
- Squamous Cell Carcinoma (SCC) of Skin is caused when skin cells (the keratinocytes that form the epidermis) are burnt or damaged from prolonged (frequently severe) exposure to the ultraviolet component of the sun, over many decades
- The source of UV may be from lamps and other such devices, apart from the sun, and their effect on the skin may cumulatively add-up
- Sometimes, individuals working in certain industries may be exposed to chemicals or x-rays for a long duration. This may also contribute to the formation of the skin cancer
- Scientific research has indicated that the human papillomavirus (HPV) along with other risk factors, such as sun-exposure, skin color, and an advancing age, seem to greatly multiply the chance of an individual being affected by SCC of Skin. Nevertheless, the reason behind how the virus is responsible for influencing the condition’s development is not well-established
What are the Signs and Symptoms of Squamous Cell Carcinoma of Skin?
The signs and symptoms of Squamous Cell Carcinoma (SCC) of Skin include:
- In majority of the cases, Cutaneous SCC is asymptomatic and does not present any signs or symptoms (during the initial period)
- Generally, it is a slow-growing tumor
- The tumor may be single; though, it is not uncommon to find multiple tumors in an individual
- The skin lesions may appear as crusted ulcer, plaques, and nodules
- It may ulcerate and bleed. Occasionally, after the ulcer heals, it may become ulcerated again
- These lesions or tumors are common in sun-exposed areas (such as face, neck, and chest), but can appear in non-sun exposed areas too
- The size of the lesions range from 1-10 cm; average size is usually less than 3 cm
- In some cases, the squamous cell carcinoma may appear more pigmented than surrounding skin
- Individuals with immunocompromised states have more aggressive tumors
The tumors that arise in a sun-damaged skin area have low risk of metastasis than tumors that are present in non-sun exposed areas.
How is Squamous Cell Carcinoma of Skin Diagnosed?
A diagnosis of Squamous Cell Carcinoma of Skin is made by:
- Complete physical examination with detailed medical history evaluation
- Examination by a dermatologist using a dermoscopy, a special device to examine the skin
- Wood’s lamp examination: In this procedure, the healthcare provider examines the skin using ultraviolet light. It is performed to examine the change in skin pigmentation
Although the above modalities can be used to make an initial diagnosis, a tissue biopsy of the tumor is necessary to make a definitive diagnosis to begin treatment.
Tissue biopsy:
- A tissue biopsy of the tumor is performed and sent to a laboratory for a pathological examination. A pathologist examines the biopsy under a microscope. After putting together clinical findings, special studies on tissues (if needed) and with microscope findings, the pathologist arrives at a definitive diagnosis. Examination of the biopsy under a microscope by a pathologist is considered to be gold standard in arriving at a conclusive diagnosis
- Biopsy specimens are studied initially using Hematoxylin and Eosin staining. The pathologist then decides on additional studies depending on the clinical situation
- Sometimes, the pathologist may perform special studies, which may include immunohistochemical stains, molecular testing, and very rarely, electron microscopic studies to assist in the diagnosis
In case of metastatic SCC, the following diagnostic procedures can be used to procure the tissue sample:
- Fine needle aspiration (FNA) biopsy of the tumor: A FNA biopsy may not be helpful, because one may not be able to visualize the different morphological areas of the tumor. Hence, a FNA biopsy as a diagnostic tool has certain limitations, and an open surgical biopsy is preferred
- Core biopsy or open biopsy of the tumor: Generally, these methods are not suited or preferred
Many clinical conditions may have similar signs and symptoms. Your healthcare provider may perform additional tests to rule out other clinical conditions to arrive at a definitive diagnosis.
What are the possible Complications of Squamous Cell Carcinoma of Skin?
The possible complications due to Squamous Cell Carcinoma (SCC) of Skin could be:
- Discomfort, irritability of the affected skin
- Large lesions may ulcerate and bleed resulting in superimposed bacterial or fungal infections
- Permanent scarring might occur with SCC and cosmetic surgery may be required to restore the skin functionally and cosmetically
- They can metastasize to the lymph nodes
- Tumors that proliferate along the nerves (perineurial invasion) or around the blood vessels have higher chances of recurrence and metastasis
- SCC of Skin in certain locations has higher chances of metastasis and they include:
- On the lips
- On the penile skin
- In the region of radiation scar
- In the region of scar due to burns
- Vulvar skin
- Perianal skin
- Tumors that are over 2 cm in size have a higher incidence of recurrence and metastasis, than tumors that are less than 2 cm in size
How is Squamous Cell Carcinoma of Skin Treated?
Early diagnosis and treatment of Squamous Cell Carcinoma of Skin is important to avoid complications such as metastasis to other regions. The treatment measures may include:
- In most cases, a wide surgical excision and removal of the entire tumor is the preferred treatment option. This may be followed by radiation therapy and/or chemotherapy
- If the tumor has metastasized (in rare cases), then a combination of chemotherapy, radiation therapy, and invasive procedures may be used to treat the tumor
- Targeted therapy medications are generally used for locally-infiltrated or metastatic SCCs. This therapy destroys the tumor cells by acting against the proteins that are responsible for tumor growth
- Use of photodynamic light or laser therapy: Light destroys the damaged cells after they are treated with a special medical application
- Curettage and cautery surgical procedure, in which the tumor is physically ‘shelled out’ from the surrounding healthy tissue and the base cauterized
- Cryotherapy: The controlled use of liquid nitrogen to force spontaneous peeling and removal of skin
- Removal of the entire affected skin layer, by cancer removal procedure (called Moh's micrographic surgery)
- Large tumors after complete skin excision may need skin grafting
- Post-operative care is important, until the surgical wound heals
Follow-up care with regular screening and check-ups are important and encouraged.
How can Squamous Cell Carcinoma of Skin be Prevented?
Currently, it may be difficult to prevent Squamous Cell Carcinoma of Skin. However, the risk for the condition may be lowered through the following measures:
- Avoiding prolonged and chronic exposure to the sun. If this is unavoidable (such as due to an occupational requirement), then take safety steps to reduce exposure to the UV rays, by using sunscreens with high sun-protection factor, using wide-brimmed hats, and protective clothing
- Being aware of the hazards of prolonged sun exposure and taking steps to protect yourself. Plan and modify your work tasks to stay out of the sun during the period, when it is the most intense
- Avoiding excessive sunbathing (particularly if you are fair-skinned), use of tanning beds, sun lamps, and chemical agents, that accelerate sun tanning
- Individuals, who are regularly exposed to the sun or work under the sun, should get their skin periodically examined by a physician. This is crucial if they suspect or notice any skin changes
Regular medical screening at periodic intervals with blood tests, scans, and physical examinations, are mandatory, due to its high metastasizing potential and possibility of recurrence. Often several years of active vigilance is necessary.
What is the Prognosis of Squamous Cell Carcinoma of Skin? (Outcomes/Resolutions)
- In general, the prognosis of Squamous Cell Carcinoma (SCC) of Skin is excellent, if it is detected and treated early. However, if it metastasizes (such as to the local lymph nodes), the prognosis is guarded or unpredictable
- In such cases of metastatic SCC of Skin, its prognosis depends upon a set of several factors that include:
- Stage of tumor: With lower-stage tumors, when the tumor is confined to site of origin, the prognosis is usually excellent with appropriate therapy. In higher-stage tumors, such as tumors with metastasis, the prognosis is poor
- The surgical resectability of the tumor (meaning, if the tumor can be removed completely)
- Overall health of the individual: Individuals with overall excellent health have better prognosis compared to those with poor health
- Age of the individual: Older individuals generally have poorer prognosis than younger individuals
- Whether the tumor is occurring for the first time or is a recurrent tumor. Recurring tumors have a poorer prognosis compared to tumors that do not recur
- Response to treatment: Tumors that respond to treatment have better prognosis compared to tumors that do not respond so well to treatment
Additional and Relevant Useful Information for Squamous Cell Carcinoma of Skin:
The following DoveMed website link is a useful resource for additional information:
Related Articles
Test Your Knowledge
Asked by users
Related Centers
Related Specialties
Related Physicians
Related Procedures
Related Resources
Join DoveHubs
and connect with fellow professionals


0 Comments
Please log in to post a comment.