What are the other Names for this Condition? (Also known as/Synonyms)
- Non-Melanotic Spinal Schwannoma
- Schwann Cell Tumor of the Spine
- Schwannoma of the Spine
What is Spinal Schwannoma? (Definition/Background Information)
- Schwannomas are benign tumors that arise from the Schwann cells around the nerves; these tumors are nerve sheath tumors. In a majority of cases, these tumors are solitary. The tumors can occur in the peripheral nerves (arms and legs) and the spinal nerves; intracranial tumors occur in the head
- Spinal Schwannomas are among the most common type of schwannomas and they occur from the nerves of the spinal cord; they constitute around one-third of the schwannomas. These tumors generally affect the cervical and lumbar region, rather than the thoracic spine. They are not usually associated with neurofibromatosis type 2 (NF2)
- A majority of Spinal Schwannomas are conventional schwannomas, which are typically benign and rarely turn malignant. Currently, no causative factors have been identified for Spinal Schwannoma. The risk factors for the tumor include a positive family history of schwannoma
- Spinal Schwannomas may be symptomatic or asymptomatic. The signs and symptoms are commonly based upon the location of the tumor on the spine. The tumor can cause lower back pain and urination difficulty (if the tumor is in the lumbar region), and breathing difficulty (if the tumor is in the cervical region)
- In rare cases, Spinal Schwannomas are known to develop into malignant tumors. The tumors can also compress the nerve on which it lies and cause nerve dysfunction
- In a majority of cases, a complete excision by surgery can be curative and the prognosis of Spinal Schwannoma is excellent. However, this may be influenced by the location of the spinal tumor
Who gets Spinal Schwannoma? (Age and Sex Distribution)
- Spinal Schwannoma is typically observed between the age ranges of 30-50 years. It is observed in young and middle-aged adults
- Both males and females are equally affected in a majority of cases
- However, against a background of neurofibromatosis type 2, the tumors may be observed with a higher incidence in females than males. Also, with respect to intracranial schwannomas, females are affected more than males
- Schwannomas have no known geographical, racial, or ethnic preference; they are seen worldwide
- The incidence of Spinal Schwannoma is reported to be around 3-4 cases per million population. They are among the more common intradural spinal cord tumors in adults (i.e., occurring within the outermost brain and spinal cord membrane)
What are the Risk Factors for Spinal Schwannoma? (Predisposing Factors)
The risk factors for Spinal Schwannoma may include:
- A family history of the tumor
- In some rare cases, the presence of neurofibromatosis type 2, a genetic condition that is characterized by the formation of non-cancerous tumors that affect the nervous system
- Schwannomatosis: It is a genetic condition that is a usually seen in adults and manifests as multiple schwannomas
- Gorlin-Koutlas syndrome: A complex genetic disorder of multiple tumors in the body including multiple Schwannomas
Note: Usually the tumors are single; but, if they are associated with NF2 or schwannomatosis, they can be multiple. However, this is very uncommon.
It is important to note that having a risk factor does not mean that one will get the condition. A risk factor increases one's chances of getting a condition compared to an individual without the risk factors. Some risk factors are more important than others.
Also, not having a risk factor does not mean that an individual will not get the condition. It is always important to discuss the effect of risk factors with your healthcare provider.
What are the Causes of Spinal Schwannoma? (Etiology)
The exact cause and mechanism of Spinal Schwannoma formation, in a majority of cases, is unknown; they are known to be the result of sporadic mutations. This implies that they do not have a preceding family history of the condition.
- Abnormalities in chromosome 22 is the most common finding
- Multiple schwannomas are known to occur in a background of genetic disorders, such as neurofibromatosis type 2 (NF2), Gorlin-Koutlas syndrome, or a positive family history
- In general, the tumor is believed to be caused by the overproduction of Schwann cells that wrap around the nerve
What are the Signs and Symptoms of Spinal Schwannoma?
Spinal Schwannoma may not present any signs and symptoms in some cases, and may be detected incidentally. In tumors with signs and symptoms, it may be dependent upon the location on the spine. These may include:
- The tumors are mostly slow-growing and solitary; they may range in size from 2-10 cm and appear as a firm mass
- Approximately, 30% of schwannomas are spinal tumors and 8% are intracranial tumors (occurring inside the head)
- Spinal Schwannomas are mostly observed in the cervical and lumbar region and may cause associated signs and symptoms. Pain from these tumors may be confined to the tumor site or spread across the region
- Lumbar plexus tumor can lead to weakness, numbness, walking difficulties, and severe shooting pain in the back, due to compression of the nerve
- If the sacral plexus nerve of the lower back is affected, it can cause back pain, alteration in bowel movements and bowel control, alteration in urinary bladder control, etc.
- If the tumor occurs in the neck region at the base of the brain, it can compress the brainstem and cause breathing difficulties
How is Spinal Schwannoma Diagnosed?
A diagnosis of Spinal Schwannoma is made using the following tools:
- Complete physical examination with thorough evaluation of the individual’s medical history (including family history of neurofibromatosis type 2 or schwannoma)
- Neurological exam of the entire body
- Radiological studies (CT, MRI scan) of the affected region
- Nerve conduction studies of the affected nerve
- Other specific tests may be conducted based on the location of the spinal tumor
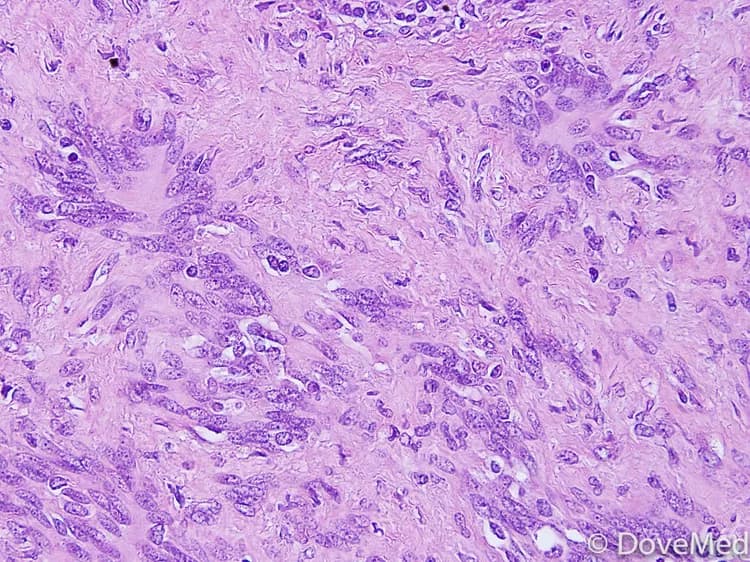
- Tissue biopsy: A tissue biopsy is performed and sent to a laboratory for a pathological examination, who examines the biopsy under a microscope. After putting together clinical findings, special studies on tissues (if needed) and with microscope findings, the pathologist arrives at a definitive diagnosis
Note: Spinal Schwannomas are usually not of plexiform histological pattern; plexiform schwannoma is a subtype of schwannoma.
Many clinical conditions may have similar signs and symptoms. Your healthcare provider may perform additional tests to rule out other clinical conditions to arrive at a definitive diagnosis.
What are the possible Complications of Spinal Schwannoma?
The complications can depend on where the tumors are located on the spine. The complications from Spinal Schwannoma could include:
- Severe compression of the brainstem can cause severe breathing problems, which can be life-threatening
- Compression of the underlying nerve can affect nerve function
- Damage to the nerve during surgery to remove the tumor. Sometimes, removing the tumor can worsen the signs and symptoms in some individuals
- Infrequently, recurrence of the tumor after surgery, if the tumor is incompletely removed
- Very rarely, Spinal Schwannomas can become malignant (malignant transformation of schwannoma)
How is Spinal Schwannoma Treated?
Treatment measures for Spinal Schwannoma may depend upon the type and location of the tumor on the spine. In many cases, if the tumor is small-sized and there are no symptoms, no treatment may be necessary. Periodic observations can be maintained through regular check-ups.
Surgical excision and tumor removal is the usual mode of treatment of Spinal Schwannoma. A very important criterion for surgery is to preserve nerve function that is affected by the tumor. Surgical treatment options may include the following:
- Microsurgery: The surgery is performed using microsurgical techniques, which can help minimize damage to the accompanying nerve. Since the tumor mostly affects the covering around the nerves, it can be completely removed without affecting the nerve in most cases. The following techniques may be employed:
- Subtotal removal; when the tumor is incompletely removed
- Near total removal; when most of the tumor is removed and there is very little tumor remnants
- Total tumor removal; when the tumor is removed completely
- Craniotomy: It is a surgical procedure wherein a tiny hole is created in the cranium to remove the tumor
- Stereotactic radiosurgery is a relatively new treatment method that can be helpful in some individuals. It is a radiation therapy technique and not an invasive surgical procedure. It can be administered using a Gamma Knife (Gamma Knife radiosurgery)
- Laminectomy: Surgical removal of the tumor can be attempted through a decompressive laminectomy for Spinal Schwannomas. This intervention tool can help relieve pressure and compression caused by the tumor on the spinal cord. It is only performed when severe symptoms are noted
In case of malignancy, additional treatment options, such as chemotherapy and/or radiation therapy, may be considered.
- Chemotherapy may be used to destroy the tumor cells
- Radiation therapy may be useful in individuals who are not candidates for surgery. Such cases include:
- Individuals with overall poor health status
- Individuals with minimal symptoms
- Treatment of the underlying neurofibromatosis type 2, if present
- Post-operative care is important: One must maintain minimum activity levels, until the surgical wound heals
- Follow-up care with regular screening and check-ups are important and encouraged
How can Spinal Schwannoma be Prevented?
Current medical research has not established a way of preventing Spinal Schwannoma.
What is the Prognosis of Spinal Schwannoma? (Outcomes/Resolutions)
- The prognosis of Spinal Schwannoma (benign tumor) is excellent, if the tumor can be removed without damaging the underlying nerve. However, this also depends upon the tumor site on the spinal cord and the severity of the associated signs and symptoms
- Asymptomatic tumors may require no treatment; unless they cause discomfort, affect the quality of life, or affect functioning of the underlying nerve. In such cases, close monitoring of the schwannoma is a treatment option
- If benign schwannomas transform to malignant tumors (in very rare occasions), then the prognosis may depend upon a set of several factors including the stage of the tumor, its location on the spine, overall health of the individual, and response to therapy
Additional and Relevant Useful Information for Spinal Schwannoma:
Please visit our Cancer & Benign Tumor Health Center for more physician-approved health information:
Related Articles
Test Your Knowledge
Asked by users
Related Centers
Related Specialties
Related Physicians
Related Procedures
Related Resources
Join DoveHubs
and connect with fellow professionals

0 Comments
Please log in to post a comment.